Abstract
It is now well established that a significant number of nurses have less than optimal levels of wellness as a result of the stressful nature of their work. Identifying effective workplace strategies to help improve the resilience of nurses is therefore a high priority. In this study, we evaluated the feasibility of a mindfulness-based intervention aimed at reducing compassion fatigue and improving emotional well-being in nurses. A total of 21 nurses recruited from a large teaching hospital in Western Australia, participated in a mindful self-care and resiliency (MSCR) intervention. The intervention consisted of a 1-day compassion fatigue prevention educational workshop, followed by a series of weekly mindfulness training seminars conducted over 4 weeks (12 h total intervention time). Participants completed a number of standardized measures at pre, post, and 1-month follow-up. Significant improvements were observed following the intervention for compassion satisfaction, burnout, trait-negative affect, obsessive passion, and stress scores. At pre-intervention, 45 % of the sample had high burnout scores, but this reduced to just 15 % by post-intervention. No significant changes were observed for general resilience, anxiety, or secondary traumatic stress post-intervention or at follow-up. The results of this preliminary study indicate that MSCR may represent a feasible approach to improving resilience and well-being among nurses. Further research utilizing a control group is required to strengthen conclusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While occupational stress is not unique to any one specific professional group, it is particularly prevalent among the helping professions (Santos et al. 2010) and nurses (Beck 2011; Hooper et al. 2010). Nurses working in acute care hospitals and similar environments are routinely exposed to organizational change, patient distress, patient trauma, unrealistic patient expectations, and high workload stressors (McVicar 2003). Such stressors experienced by healthcare workers and nurses can take a high professional and emotional toll and can result in the acute syndrome known as compassion fatigue (CF: Figley 1995).
Figley (1995) defined CF as a combination of secondary traumatic stress (STS) and burnout. Compassion fatigue in this conception develops from the negative aspects of care provision and is the consequence of the demands of caregiving to distressed individuals. Secondary traumatic stress is an acute condition that can occur for carers and health professionals frequently exposed to the stress and trauma of others, and may include anxiety, intrusive images, cognitive and behavioral avoidance, and symptoms similar to those of the person that has been traumatized. On the other hand, burnout is a work-related stress symptom involving emotional exhaustion, frustration, depressed mood, and an inability to work effectively (Maslach, Schaufeli, and Leiter 2001). These two conditions are highly related and together are considered to be representative of CF (Stamm 2010).
In the nursing profession, research has shown that CF is associated with a number of deleterious effects including psychological distress, reduced productivity, increased absenteeism, and therefore the potential for increased risks to patient safety (Adams et al. 2006; Leiter and Maslach 2009). A prominent view that informs how CF might be understood and addressed is the stress process model (Figley 2002). In this conception, the process of empathy towards a traumatized client’s experience results in physiological and cognitive responses, and if not managed adaptively may result in a residue of negative emotional energy that can lead to CF. Similarly, Zeidner et al. (2013) have argued that personality-related characteristics involving difficulties with modulating and coping with emotional responses to stress may be central to the development of CF.
Research has typically investigated the environmental and psychological correlates of CF as a way of understanding risk and protective factors, and therefore informing interventions that build resilience. Exposure to traumatized individuals is one obvious environmental factor that has been previously linked to CF development (Adams et al. 2006, 2008). However, numerous other factors have been associated with CF and burnout, such as personal trauma history, support, policy, leadership, coping, self-efficacy, and sense of mastery (Adams et al. 2008; Adriaenssens et al. 2014; Laschinger and Fida 2014). Studies have also linked the personality disposition of neuroticism and the related construct of trait-negative affect (TNA: proneness to experience negative emotion, Watson and Clark 1984) to occupational stress (Swider and Zimmerman 2010) and CF symptoms in health care workers and nurses (Breslau and Schultz 2013; Craigie et al. 2015). These findings are consistent with past research that suggests difficulties with emotion regulation and coping underlie the development of stress-related mood disorders (Barlow 2004; Carver and Connor-Smith 2010) and CF more specifically (Zeidner et al. 2013).
In contrast, one’s way of engaging work tasks and of identifying with work may protect or contribute to occupational stress. Vallerand et al. (2003) have shown that a willing engagement in activity that has been freely accepted as important and free of contingencies, referred to as harmonious passion, predicted greater positive affect and less negative affect when engaging tasks. Harmonious passion in nurses also predicted higher work satisfaction and lower burnout at a later time (Vallerand et al. 2010). Conversely, intense engagement in an activity that is perceived as outside one’s control and reflects contingent self-esteem, social acceptance, or performance, referred to as obsessive passion (Vallerand et al. 2003), predicted higher negative cognition and emotion when engaging in a passionate activity (Mageau et al. 2005; Vallerand et al. 2003). In addition, higher obsessive passion predicted higher emotional exhaustion (Lavigne et al. 2012) and greater work-life role conflict (Vallerand et al. 2010). Vallerand et al. (2010) have therefore argued that harmonious passion protects against burnout, as it facilitates work satisfaction and positive affect, whereas obsessive passion contributes to burnout through role conflict and negative affect.
As a whole, the research suggests a complex process of CF development involving a multitude of environmental and individual factors. Interventions that focus on changes to the work environment may assist in reducing negative affect and therefore risk for CF. However, the role of nursing in acute care settings invariably requires frequent contact with distressed/traumatized patients and their families (Beck 2011). Zeller and Levin (2013) proposed that for nurses, it is more feasible and effective to develop interventions that focus on building psychological resilience and adaptive coping to stress, rather than work environment interventions alone.
A challenge for designing interventions aimed at increasing psychological resilience has been the complex and multidimensional nature of resilience (Southwick and Charney 2012). The American Psychological Association (APA 2015, p.1) defined resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress”. In this paradigm, psychological resilience is not considered a fixed trait, but rather involves adaptive ways of thinking and behaving that can be learned (Southwick and Charney 2012). A recently proposed general model of individual resilience to occupational stress put forward by Rees et al. (2015) has provided one way of organizing key individual difference variables likely to act as positive/protective (e.g., self-efficacy, harmonious passion) and negative factors (e.g., TNA, obsessive passion) for adjustment to work stress. Rees et al. argued that while some variables in the model are more stable and hence less amenable to change (e.g., personality traits), others are malleable and represent candidates for interventions aimed at increasing workplace well-being. Notably, compassion satisfaction (positive feelings about one’s role as a carer, Stamm 2010) is a positive indicator of adjustment and personal coping resources in caregivers (Tremblay and Messervey 2011) and has been previously associated with lower CF symptoms in nurses (Craigie et al. 2015), higher levels of positive reappraisal, positive affect (Samios, Abel, and Rodzik 2013), and mindfulness (Thomas and Otis 2010).
Interventions that target adaptive emotion regulation and patterns of thinking in response to stressors and foster new ways of relating to work may be central to the prevention and amelioration of CF. However, relatively few studies have evaluated such interventions. For example, Flarity et al. (2013) evaluated a CF resiliency intervention for emergency nurses based on Gentry and Baranowsky’s (1998) original CF recovery protocol, but delivered as a brief 4-h educational seminar. This program focused on teaching skills for identifying symptoms of CF and implementing adaptive ways of regulating anxious arousal and problematic thinking in order to reduce habitual and obsessive responding to stressors, and increase self-care and actions in harmony with core values. The study reported significant reductions in CF symptoms and improvements in compassion satisfaction. A parallel study by Potter et al. (2013) yielded similar results in oncology nurses. Longer (12-week) multimodal interventions for nurses have also demonstrated significant benefits (Berger and Gelkopf 2011; Mealer et al. 2014), although complexity and length may limit their broader adoption.
While these recent approaches are promising, a central process underlying CF appears to relate to difficulties with regulating emotional reactions when confronting stressors and traumatized patients (Figley 2002), and perhaps an obsessive and rigid engagement with work (Vallerand et al. 2010). Mindfulness training is one approach designed to enhance emotion regulation and recovery from stressors (Teper, Segal, and Inzlicht 2013). Mindfulness has also been linked to more flexible cognitive and behavioral responses to stress eliciting tasks (Good et al. 2015), and it has been argued may play an important role in resilience to trauma (Thompson, Arnkoff, and Glass 2011).
To the present time, mindfulness-based stress reduction (MBSR: Kabat-Zinn 1990) and mindfulness-based cognitive therapy (MBCT: Segal et al. 2002) are the most prominent mindfulness-based interventions aimed at enhancing mindfulness. Mindfulness in these paradigms has been defined as the “awareness that emerges through paying attention on purpose, in the present moment, and nonjudgementally” (Kabat‐Zinn 2003, p. 145). Clinical research has shown MBSR/MBCT to yield benefits in terms of reducing negative mood and preventing depression (Khoury et al. 2013) and increasing mindfulness, self-compassion, and positive affect (van der Velden et al. 2015). Moreover, mindfulness has been associated with reduced impulsivity to stressors (Mantzios 2014) and increased positive reappraisal of stressors (Garland et al. 2010). In occupational settings, mindfulness-based interventions have also resulted in lower stress (Wolever et al. 2012) and burnout (Goodman and Schorling 2012; Ruths et al. 2013) and higher job satisfaction (Hülsheger et al. 2013).
Notwithstanding, a number of issues may prevent group-based programs like MBSR and MBCT from being effectively delivered to acute care nurses. First, both programs involve eight weekly sessions of 2-h duration (and a 1-day retreat), with participants encouraged to perform up to 40 min of formal mindfulness practice per day. Zeller and Levin (2013) have recognized the challenge of recruiting and retaining busy workers such as nurses in such intensive programs. In addition, there is uncertainty about whether longer programs are any more effective than shorter programs (Carmody and Baer 2009; Dharmawardene et al. 2015). Second, the rationale for MBSR/MBCT relates to clinical health conditions and depression, not occupational stress or CF. Transferring such protocols into work settings without an appropriate rationale and modification may conceivably limit their relevance and acceptability to nurses. Fortunately, a few studies have shown that briefer and less intensive mindfulness-based interventions lead to significant reductions in burnout symptoms in nurses and health care workers (Gauthier et al. 2015; Mackenzie et al. 2006) and increased resilience in physicians (Sood et al. 2011). However, there has been a paucity of such intervention studies for nurses that integrate CF education and explain the role of mindfulness for resiliency.
Given the deleterious effects of CF in the nursing workforce and relatively few interventions specifically designed for CF resiliency, the primary aim of this study was to extend the work of previous research (e.g., Flarity et al. 2013; Mackenzie et al. 2006) by augmenting CF resiliency psychoeducation with a brief mindfulness-based intervention. The present study involved an initial pilot evaluation of the feasibility of a mindful self-care and resiliency (MSCR) program for CF prevention in a nurse sample working at an acute care tertiary hospital. It was predicted that MSCR would be associated with reduced burnout, STS, and negative mood symptoms. Moreover, MSCR would be associated with a decrease in established risk factors associated with burnout, namely TNA and obsessive passion. Similarly, we were interested in exploring if MSCR would be associated with improvement in positive/protective factors for occupational stress, such as compassion satisfaction, harmonious passion, and the broader construct of general resilience.
Method
Participants
Twenty-five nurses expressed interest in the MSCR program, and of these, 24 met inclusion criteria. After final scheduling of the intervention groups, a total of 21 nurses commenced the program. The mean age of this sample was 48.6 years (SD = 9.94, range 24 to 62 years), 95.2 % (n = 20) were female, 61.9 % were married or in a de facto relationship, 76.2 % had Australian citizenship, and 42.9 % had a dependent person who affected their capacity to work. Inclusion criteria were working as a registered nurse, in either a full-time or part-time capacity at the study hospital. Participants were excluded if screening measures revealed clinical levels of depression, or symptoms consistent with post-traumatic stress disorder (PTSD), or the presence of substance abuse. Similarly, nurses were excluded if they reported currently receiving treatment for a mental health condition or reported circumstances likely to interfere with their regular attendance at intervention sessions. The work profile characteristics of nurses commencing the program are presented in Table 1. As can be seen, more than 80 % of nurses were working full-time, more than half were senior registered nurses, and the large majority of the sample had more than 15 years of nursing experience.
Procedure
This study employed a pre–post-follow-up within-subjects design. The primary dependent variable of interest was CF (burnout and STS) with the independent variable being time (pre-intervention vs. post-intervention and pre-intervention vs. 1-month follow-up).
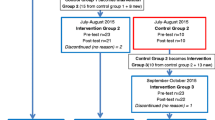
Following ethics approval from both the university and hospital ethics committees, potential participants were recruited via distribution of an advertisement outlining the program and start dates of the two intervention groups being offered. This information was circulated via the hospital intranet to the senior nurse staffing group. All interested parties were asked to contact the researcher who then organized for the information sheet and consent form to be sent. On receipt of the consent form, the name, contact details, and group allocation of the potential participant were sent to the program coordinator who then undertook telephone screening interviews to assess inclusion/exclusion criteria.
Two intervention groups were conducted, with 10 and 11 participants in each group. Prior to the intervention, participants were requested to complete a paper-based survey consisting of several self-report questionnaires and a short demographic section. The same survey (without the demographics) was repeated at the completion of the last session and 1 month following the last session for each group. Intervention groups were conducted in a private seminar room of a multifunction research building located on the hospital grounds.
The MSCR intervention was a total of 12 h in duration and comprised a 1-day educational workshop on compassion fatigue resiliency (three 1.75-h sessions) and introduction to mindfulness (1.75-h session), followed immediately by a series of weekly mindfulness skills seminars conducted over a period of 4 weeks. The content and materials of the first three sessions of the workshop were adapted with permission from Eric Gentry’s Compassion Fatigue Prevention and Resiliency, Fitness for the Frontline (CFPR-FF) workshop (J. E. Gentry, personal email communication, November 7–9, 2013). The CFPR-FF workshop has been previously described by Flarity et al. (2013). The content of this component involved PowerPoint slides and information/worksheets used for mini-lectures and group exercises (Gentry 2013). Each participant was provided with a client manual that included intervention educational materials. The 1-day workshop comprised education about CF and its causes, and skills to build CF resiliency, referred to as the five “antibodies” ((1) self-regulation; (2) intentionality; (3) perceptual maturation; (4) connection and social support; and (5) self-care and revitalisation). Supplemental Tables S1 and S2 provide a detailed break-down of activities for all intervention sessions. However, for standardization, ease of dissemination, and cultural relevance to an Australian nurse population reasons, a short introductory video that was used in the Flarity et al. (2013) study was not included.
The MSCR mindfulness seminars were adapted from the eight-session Segal et al. (2002) MBCT program, and in part aligned with the format of an abbreviated four-session protocol evaluated by Mackenzie et al. (2006). The first seminar occurred in the fourth session of the 1-day workshop. The remaining four seminars began 1 week later, occurring midafternoon on a weekly basis. A central aim of the seminars was to learn mindfulness to support CF resiliency skills. Each seminar was 1.5 h in duration and involved both experiential activities and didactic discussion and generally involved briefer mindfulness practices (about 10 to 25 min) as described by Williams and Penman (2011).
Learning objectives of the mindfulness seminars were increasing awareness of automatic pilot and stress-related reactions, and applying mindful responses to be more present/intentional (e.g., breathing space, 3 sighs) so as to promote perceptual maturation, values-based actions, and self-care. Seminar themes were introduction to mindfulness, staying present, allowing/letting be, thoughts as thoughts, and review and planning for the future. Each participant was provided with the book, Mindfulness a Practical Guide to Finding Peace in a Frantic World by Williams and Penman (2011), which includes a practice CD. For homework, participants were encouraged to complete a mindfulness practice each day using the CD (typically about 10 to 20 min in duration), as well informal practices. The MSCR client manual described key session themes and home-based practice tasks.
The MSCR program structure and format were developed and facilitated by the first author of this study. The facilitator is a registered clinical psychologist with more than 6 years of experience facilitating MBCT groups in an outpatient mental health setting, as well as experience in delivering mindfulness-based training to health professionals. Moreover, he had previously completed a CFPR-FF 1-day workshop conducted by Eric Gentry. Treatment adherence was maintained by closely following a timetable of activities and tasks as outlined in Table S1 and S2 of the supplemental materials, and described in the MSCR client manual.
Measures
The Patient Health Questionnarie-9 (PHQ-9, Kroenke and Spitzer 2002), Short Screening Scale for DSM-IV PTSD (SSSP, Breslau et al. 1999), and the CAGE questionnaire (Mayfield, McLeod, and Hall 1974) adapted for drug use (CAGE-AID, Brown and Rounds 1995) were used to assess exclusion criteria pertaining to core symptoms/features of clinical depression, PTSD, and alcohol and substance misuse, respectively. A recommended cutoff score for each of the measures was used to assess if participants met criteria for the presence of clinically significant symptoms. Research has shown that the PHQ-9 is a valid clinical depression screening tool for the general population (Martin et al. 2006). Likewise, research suggests the SSSP is a reliable and valid measure for screening of PTSD symptoms (Kimerling et al. 2006) and the CAGE-AID for identifying the presence of alcohol and substance use problems (Hinkin et al. 2001).
The Demographic Questionnaire included age, sex, marital status, country of citizenship, dependents, current position, employment hours, inpatient or outpatient unit, highest qualification, post-registration qualifications, length of time in nursing, length of time at study hospital, length of time in current position, and expected time to work in nursing.
The Professional Quality of Life Scale version 5
(ProQoL5; Stamm 2010). The ProQoL5 comprises three subscales that measure levels of compassion satisfaction and CF; the latter concept is composed of burnout and STS subscales. Compassion satisfaction is a positive indicator of work adjustment, reflecting feelings of satisfaction, and pleasure in caring for others and doing work well. In contrast, the burnout subscale reflects the negative aspects of caring involving feelings of exhaustion, frustration, and depressed mood. The STS subscale reflects avoidance and negative feelings driven by fear and work-related trauma. The ProQoL5 utilizes 30 items on a 5-point scale to measure each of these three subscale components (10 items each). Respondents are asked to rate each statement in relation to how frequently it applies to them over the last 30 days. The ProQoL scale has been psychometrically validated in different health professional populations (Stamm 2010) and has previously demonstrated sound psychometric properties for nurses working in an Australian hospital (Hegney et al. 2014). The reliabilities at pre-intervention for each subscale in this study were compassion satisfaction α = .89, burnout α = .75, and STS α = .60.
Depression Anxiety Stress Scales
(DASS, Lovibond and Lovibond 2004). The DASS is a widely used instrument used to measure levels of depression, anxiety, and stress symptoms over the past week. The DASS21 was used in this study and is a 21-item version of the longer 42-item DASS. The DASS21 consists of three 7-item subscales: depression, anxiety, and stress. Participants are asked to rate each item statement on a 4-point scale. Each subscale is summed to obtain a total score for the respective subscale. Higher scores represent higher levels of negative symptomatology. DASS subscale scores have been previously shown to be strongly correlated with burnout and STS in an Australian nurse sample (Hegney et al. 2014). The DASS has demonstrated strong psychometric properties in both clinical and general adult populations (Lovibond and Lovibond 2004). DASS21 scores are multiplied by a factor of 2 to obtain a DASS full-scale score. The reliabilities at pre-intervention for each subscale in this study were depression α = .72, anxiety α = .40, and stress α = .82.
Spielberger State-Trait Anxiety Inventory form Y2
(STAI-Y2, Spielberger, Gorsuch, Lushene, Vagg, and Jacobs 1983) The STAI-Y2 was used to measure the construct of trait-negative affect (TNA)—the tendency to experience a variety of negative emotions across a range of situations (Watson and Clark 1984). The STAI-Y2 represents a general negative emotionality variable related to negative self-appraisals of coping with emotion eliciting stressors (Carver and Connor-Smith 2010) and consists of 20 items both positively and negatively worded that are measured on a 4-point scale. Respondents rate statements according to how the statements describe how they “generally feel”. Items are summed to produce a total scale score. Higher scores represent higher levels of TNA. The STAI-Y2 has been frequently used to assess anxiety management interventions (Manzoni et al. 2008). The measure has also demonstrated sound psychometrics in a range of populations (Spielberger et al. 1983), and research supports its validity as a measure of TNA (Bados, Gómez-Benito, and Balaguer 2010). The reliability at pre-intervention for this study was α = .92.
Connor-Davidson Resilience Scale
(CD-RISC, Connor and Davidson 2003). The CD-RISC is self-report measure of general psychological resilience that reflects positive self-beliefs in regard to dealing with problems, recovering from hardship, and tolerating negative emotion. Previous studies suggest the scale is a valid and reliable measure of resilience for a range of normal and clinical populations (Connor et al. 2003; Gillespie 2007). The original 25-item scale uses a 5-point response format, with higher scores reflecting greater resilience. The present study used a shorter 10-item version (CD-RISC10) that assesses aspects of resilience pertaining to a central core resilience construct (Campbell‐Sills and Stein 2007). The CD-RISC has also been frequently used in resiliency interventions (Loprinzi et al. 2011; Sood et al. 2011). The pre-intervention reliability for the current study was α = .85.
Passion for Work Scale
(PWS, Vallerand et al. 2003). The PWS is a 14-item scale with a 7-point response format that measures harmonious and obsessive passion (7 items each). A passion is a strong inclination toward a self-defining activity that individuals like and value, and in which they invest time and energy (Vallerand et al. 2003). Harmonious passion results from the internalization of an important activity into one’s personal identity that produces a motivational force to engage in an activity willingly. Obsessive passion results from the control internalization of an activity into one’s identity that originates from intrapersonal or interpersonal pressure (Vallerand et al. 2003). Previous research suggests the PWS is a reliable and valid measure (Lavigne et al. 2012; Vallerand et al. 2003, 2010). In this study, the reliability at pre-intervention for harmonious passion was α = .87, and for obsessive passion was α = .93.
Data Analyses
All statistical analyses were performed with IBM-Statistical Package for the Social Sciences (IBM-SPSS) Windows version 21. Kolmogorov–Smirnov and Shapiro–Wilk tests were used to examine study variable distributions. These tests revealed significant departures from normality for most variables at one or more assessment points. As such, Wilcoxon signed-rank non-parametric tests were used to assess within-group changes for study variables from pre to post intervention, and pre to follow-up. Cohen’s (1988) d effect size was used to determine the magnitude of variable changes between assessment points (d = difference mean/standard deviation of difference mean; d = .3 is small, .5 is medium, .8 is large). To clarify the meaning of changes in burnout and STS, the descriptive frequency method used by Berger and Gelkopf (2011) was adopted. Following Stamm’s (2010, p.16) recommendations, ProQol5 scores at each assessment point were converted to standardized t scores and then assigned risk categories (low, average, high) based on percentile cut scores.
Results
A total of 20 nurses completed the MSCR intervention in terms of providing a complete set of questionnaire data, attending the 1-day workshop, and at least two of the weekly mindfulness seminars. Table 2 shows mean scores from pre-test to post-test and 1-month follow-up assessment points for program completers. Wilcoxon signed-rank paired sample test showed there were significant reductions for depression, burnout, and TNA scores at post-test. Effect sizes for these changes were in the medium range for depression and TNA, and in the large range for burnout. At 1-month follow-up, significant reductions were maintained for burnout and TNA, but not depression scores. In addition, significant reductions in obsessive passion and stress were observed from pre-test to 1-month follow-up, as well as a significant improvement in compassion satisfaction. The changes observed for obsessive passion, stress, and compassion satisfaction were all in the medium effect size range. However, there were no significant improvements for general resilience and harmonious passion from pre-test to post-test or at 1-month follow-up. Similarly, STS and anxiety symptoms did not significantly reduce from pre-test to post-test or follow-up.
Table 3 displays percentages and frequencies according to Stamm’s (2010) risk categories. As shown, 45 % of participants had burnout scores falling in the high range at pre-test, which reduced to 15 % at post-test and follow-up. For STS, only 20 % of participants had scores falling in the high range at pre-test, with no change by follow-up. Despite the lack of change for STS scores in the high range, Table 3 also shows that the rate of participants falling in the low range improved by 15 % at follow-up. For compassion satisfaction, 35 % of participants fell into the low range at pre-test. By follow-up this rate had reduced to 15 %, with a commensurate improvement of participants falling in the high range.
Discussion
Given the high rates of burnout and CF among health professionals, it is imperative that efforts are made to develop and test interventions that can ameliorate such negative outcomes. In this pilot study, we evaluated the feasibility of a brief mindfulness-based CF resiliency intervention for nurses working in a large teaching hospital in Australia. Our primary finding is that there were significant improvements across a number of symptom domains following the MSCR intervention. Importantly, a significant reduction in burnout scores (one aspect of CF) was observed following the intervention and at follow-up. In the current sample of nurses, nearly half had levels of burnout that were in the high category according to Stamm’s (2010) risk criteria. At post-intervention, only 15 % were reporting levels of burnout in the high category. The fact that this result was maintained at 1-month follow-up is promising because it suggests that the benefits of the intervention persist beyond the initial training period, although further studies with longer follow-ups and larger samples are required to strengthen such a conclusion.
Like burnout, we also found significant reductions in TNA levels, both directly after the intervention and maintained at 1-month follow-up. This, along with significant reductions in depressed mood post-intervention and reduction in stress and improvement in compassion satisfaction by 1-month follow-up, suggest that the intervention was associated with changes across a number of important areas of psychological functioning. The findings combined with a high completion rate provide preliminary evidence for the feasibility of integrating CF resiliency education with mindfulness skills training to nurses working in stressful environments. Moreover, the results help to generalize earlier intervention findings (e.g., Flarity et al. 2013; Mackenzie et al. 2006) to nurses in an Australian hospital.
Improvements in TNA and compassion satisfaction also appear consistent with the view that mindfulness-based interventions like MSCR may enhance regulation of negative affect as well as building positive affect related coping resources (e.g., Garland et al. 2010; Teper et al. 2013). Previous research has shown that TNA is strongly related to burnout and compassion satisfaction to lower TNA and lower burnout (Craigie et al. 2015). Therefore, it might be conjectured that MSCR may help to initially facilitate cognitive reappraisal of emotion eliciting stressors (e.g., Garland et al. 2010), which leads to higher compassion satisfaction and lower obsessive passion at a later time. In addition, given obsessive passion is related to higher negative cognition, negative affect, and work-life role conflict (Mageau et al. 2005; Vallerand et al. 2010), and compassion satisfaction reflects greater positive affect, it seems possible that improvement on these processes may have further contributed to reducing negative mood symptoms that typify burnout. Future controlled studies may wish to test such causal hypotheses.
However, no significant reductions were observed for STS and anxiety symptoms. Several ideas can be advanced as to these findings. First, STS scores were not particularly elevated at pre-intervention compared to burnout in terms of the rate of scores falling in the high range (e.g., 45 % for burnout vs. 20 % for STS). This feature combined with the small sample size suggests the study may have lacked power to capture modest effects that may have occurred at more moderate levels of STS as is suggested by the 15 % improvement in the rate of participants falling in the low STS range by follow-up. It is also noteworthy that the sample consisted predominantly of experienced senior nurses, and previous research by Hegney et al. (2014) has shown years in nursing is related to lower anxiety in an Australian nurse sample. Perhaps, longer experience as a nurse reflects the presence of higher levels of resiliency-based coping skills that prevent the acquisition of STS and anxiety. This is consistent with the observation that mean DASS mood scores all fell in the normal range at pre-test when compared to Australian adult norms (see Crawford et al. 2011), with anxiety lower than stress and depression symptoms. Conversely, it is conceivable that MSCR does not sufficiently address factors that maintain STS, and that much longer multicomponent interventions are required to address STS (e.g., Berger and Gelkopf 2011; Mealer et al. 2014).
In relation to the lack of improvement for general resilience and harmonious passion, a brief intervention like MSCR might not sufficiently address processes underlying protective factors that may be more character-based in nature. Alternatively, given the majority of participants were senior nurses, perhaps scores on these constructs were already elevated, and when combined with a small sample size, there was insufficient power to detect more modest effects. This hypothesis seems particularly pertinent to resilience given previous studies that have detected effects used the longer 25-item CD-RISC form (e.g., Loprinzi et al. 2011; Sood et al. 2011), rather than the short form used in the present study. Future studies may therefore require larger sample sizes or conversely more symptomatic samples to more definitively determine if MSCR can improve positive resources like resilience and harmonious passion.
A number of limitations of the study design temper strong conclusions. Replication studies with comparison/control conditions and longer follow-up periods are required to determine if the short-term improvements are maintained over the longer term and are not just the result of time or non-specific factors. Moreover, it will be important to determine if the findings can be generalized to other nurse populations that may be less experienced and or more symptomatic, especially in regard to STS. The preliminary nature of the study and imperative to minimise questionnaire burden meant that a broader range of constructs measuring positive resources purported to underlie resilience such as mindfulness, coping self-efficacy, self-compassion, positive emotion, or cognitive reappraisal were not included. Examining change on such constructs in the future might shed light on what may be some of the active ingredients underlying MSCR. As a first step, a follow-up phase of the current study (manuscript in preparation) involved interviews with participants about what they found helpful about the program to assist in identifying what might be some of the active ingredients from the perspective of participants.
The primary implication of the present findings is that a relatively brief workplace intervention may represent a feasible approach to improving resilience and well-being among nurses. As the MSCR intervention is a group program, it may also confer a cost-effective means for CF resiliency. Given there is a strong need to establish deliverable CF resiliency interventions for nurses, further controlled replication in larger samples appears warranted.
References
Adams, R. E., Boscarino, J. A., & Figley, C. R. (2006). Compassion fatigue and psychological distress among social workers: a validation study. American Journal of Orthopsychiatry, 76(1), 103–108. doi:10.1037/0002-9432.76.1.103.
Adams, R., Figley, C., & Boscarino, J. (2008). The compassion fatigue scale: its use with social workers following urban disaster. Research on Social Work Practice, 18(3), 238–250. doi:10.1177/1049731507310190.
Adriaenssens, J., De Gucht, V., & Maes, S. (2014). Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. International Journal of Nursing Studies, 52(2), 649–661. doi:10.1016/j.ijnurstu.2014.11.004.
American Psychological Association (2015). The road to resilience. Washington DC: American Psychological Association. http://www.apa.org/helpcenter/road-resilience.aspx. Accessed 20 September, 2015.
Bados, A., Gómez-Benito, J., & Balaguer, G. (2010). The state-trait anxiety inventory, trait version: does it really measure anxiety? Journal of Personality Assessment, 92(6), 560–567. doi:10.1080/00223891.2010.513295.
Barlow, D. H. (2004). Anxiety and its disorders: the nature and treatment of anxiety and panic (2nd ed.). New York: Guilford Press.
Beck, C. T. (2011). Secondary traumatic stress in nurses: a systematic review. Archives of Psychiatric Nursing, 25(1), 1–10. doi:10.1016/j.apnu.2010.05.005.
Berger, R., & Gelkopf, M. (2011). An intervention for reducing secondary traumatization and improving professional self-efficacy in well baby clinic nurses following war and terror: a random control group trial. International Journal of Nursing Studies, 48(5), 601–610. doi:10.1016/j.ijnurstu.2010.09.007.
Breslau, N., Peterson, E., Kessler, R., & Schultz, L. (1999). Short screening scale for PTSD. American Journal of Psychiatry, 156, 908–911. doi:10.1176/ajp.156.6.908.
Breslau, N., & Schultz, L. (2013). Neuroticism and post-traumatic stress disorder: a prospective investigation. Psychological Medicine, 43(8), 1697–1702. doi:10.1017/S0033291712002632.
Brown, R. L., & Rounds, L. A. (1995). Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wisconsin Medical Journal, 94(3), 135–140.
Campbell‐Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD‐RISC): validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. doi:10.1002/jts.20271.
Carmody, J., & Baer, R. A. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638. doi:10.1002/jclp.20555.
Carver, C. S., & Connor-Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61(1), 679–704. doi:10.1146/annurev.psych.093008.100352.
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences (second ed.). Lawrence Erlbaum Associates.
Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: the Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. doi:10.1002/da.10113.
Connor, K. M., Davidson, J. R. T., & Lee, L.-C. (2003). Spirituality, resilience, and anger in survivors of violent trauma: a community survey. Journal of Traumatic Stress, 16, 487–494. doi:10.1023/A:1025762512279.
Craigie, M., Osseiran-Moisson, R., Hemsworth, D., Aoun, S., Francis, K., Brown, J., Hegney, D., & Rees, C. (2015). The influence of trait-negative affect and compassion satisfaction on compassion fatigue in Australian nurses. Psychological Trauma: Theory, Research, Practice, and Policy. doi:10.1037/tra0000050.
Crawford, J. R., Cayley, C., Wilson, P. H., Lovibond, P. F., & Hartley, C. (2011). Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales. The Australian Psychologist, 46, 3–14. doi:10.1111/j.1742-9544.2010.00003.x.
Dharmawardene M., Givens J., Wachholtz A., Makowski, S., & Tjia, J. (2015). A systematic review and meta-analysis of meditative interventions for informal caregivers and health professionals. BMJ Supportive & Palliative Care, 1–10. doi:10.1136/bmjspcare2014-000819.
Figley, C. R. (2002). Treating compassion fatigue. New York, NY: Brunner-Routledge.
Figley, C. R. (1995). Compassion fatigue as secondary traumatic stress disorder: an overview. In C. R. Figley (Ed.), Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those who Treat the Traumatized (pp. 1–20). NY: Brunner.
Flarity, K., Gentry, J. E., & Mesnikoff, N. (2013). The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Advanced Emergency Nursing Journal, 35(3), 247–258. doi:10.1097/TME.0b013e31829b726f.
Garland, E. L., Fredrickson, B., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. doi:10.1016/j.cpr.2010.03.002.
Gauthier, T., Meyer, R. M., Grefe, D., & Gold, J. I. (2015). An on-the-job mindfulness-based intervention for pediatric ICU nurses: a pilot. Journal of Pediatric Nursing, 30(2), 402–409. doi:10.1016/j.pedn.2014.10.005.
Gentry, J. E. (2013). Powerpoint slides for compassion fatigue prevention and resilience. Retrieved from http://www.compassionunlimited.com/Resource/CF-PESI (2012).pptx, November 10, 2013.
Gentry, J., & Baranowsky, A. (1998). Treatment manual for the accelerated recovery program. Toronto ON: Psych Ink Resource.
Gillespie, B. M. (2007). The Predictors of Resilience in Operating Room Nurses. (PhD), Griffith, Gold Coast, Australia.
Goodman, M. J., & Schorling, J. B. (2012). A mindfulness course decreases burnout and improves well-being among healthcare providers. The International Journal of Psychiatry in Medicine, 43(2), 119–128. doi:10.2190/PM.43.2.b.
Good, D. J., Lyddy, C. J., Glomb, T. M., Bono, J. E., Brown, K. W., Duffy, M. K., & Lazar, S. W. (2015). Contemplating mindfulness at work: an integrative review. Journal of Management, Online, November. doi:10.1177/0149206315617003.
Hegney, D., Craigie, M., Osseiran-Moisson, R., Drury, V., Aoun, S., Hemsworth, D., & Francis, K. (2014). Compassion fatigue, compassion satisfaction, anxiety and depression in Western Australian nurses: a questionnaire survey. Journal of Nursing Management, 22, 506–518. doi:10.1111/jonm.12160.
Hinkin, C., Castellon, S., Dickson-Fuhrman, E., Daum, G., Jaffe, J., & Jarvik, L. (2001). Screening for drug and alcohol abuse among older adults using a modified version of the CAGE. American Journal of Addiction, 10(4), 319–326. doi:10.1111/j.1521-0391.2001.tb00521.x.
Hooper, C., Craig, J., Janvrin, D., Wetsel, M., & Reimels, E. (2010). Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. Journal of Emergency Nursing, 36(5), 420–427. doi:10.1016/j.jen.2009.11.027.
Hülsheger, U. R., Alberts, H. J., Feinholdt, A., & Lang, J. W. (2013). Benefits of mindfulness at work: the role of mindfulness in emotion regulation, emotional exhaustion, and job satisfaction. Journal of Applied Psychology, 98(2), 310. doi:10.1037/a0031313.
Kabat-Zinn, J. (1990). Full catastrophe living. New York: Dell Publishing.
Kabat‐Zinn, J. (2003). Mindfulness‐based interventions in context: past, present, and future. Clinical Psychology: Science and Practice, 10(2), 144–156. doi:10.1093/clipsy.bpg016.
Kimerling, R., Ouimette, P., Prins, A., Nisco, P., Lawler, C., Cronkite, R., & Moos, R. H. (2006). Utility of a short screening scale for DSM-IV PTSD in primary care. Journal of General Internal Medicine, 21(1), 65–67. doi:10.1111/j.1525-1497.2005.00292.x.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., & Hofmann, S. G. (2013). Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. doi:10.1016/j.cpr.2013.05.005.
Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 1–7. doi:10.3928/0048-5713-20020901-06.
Laschinger, H. K. S., & Fida, R. (2014). New nurses burnout and workplace well-being: the influence of authentic leadership and psychological capital. Burnout Research, 1, 19–28. doi:http://dx.doi.org/10.1016/j.burn.2014.03.002.
Lavigne, G. L., Forest, J., & Crevier-Braud, L. (2012). Passion at work and burnout: a two-study test of the mediating role of flow experiences. European Journal of Work and Organizational Psychology, 21(4), 518–546. doi:10.1080/1359432X.2011.578390.
Leiter, M. P., & Maslach, C. (2009). Nurse turnover: the mediating role of burnout. Journal of Nursing Management, 17(3), 331–339. doi:10.1111/j.1365-2834.2009.01004.x.
Loprinzi, C. E., Prasad, K., Schroeder, D. R., & Sood, A. (2011). Stress management and resilience training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clinical Breast Cancer, 11(6), 364–368. doi:10.1016/j.clbc.2011.06.008.
Lovibond, S. F., & Lovibond, P. F. (2004). Manual for the depression anxiety stress scales (2nd ed.). Sydney: The Psychology Foundation of Australia.
Mackenzie, C. S., Poulin, P. A., & Seidman-Carlson, R. (2006). A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Applied Nursing Research, 19, 105–109. doi:10.1016/j.apnr.2005.08.002.
Mageau, G. A., Vallerand, R. J., Rousseau, F. L., Ratelle, C. F., & Provencher, P. J. (2005). Passion and gambling: investigating the divergent affective and cognitive consequences of gambling. Journal of Applied Social Psychology, 35(1), 100–118. doi:10.1111/j.1559-1816.2005.tb02095.x.
Manzoni, G. M., Pagnini, F., Castelnuovo, G., & Molinari, E. (2008). Relaxation training for anxiety: a ten-years systematic review with meta-analysis. BMC Psychiatry, 8(1), 41. doi:10.1186/1471-244X-8-41.
Martin, A., Rief, W., Klaiberg, A., & Braehler, E. (2006). Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. General Hospital Psychiatry, 28(1), 71–77. doi:10.1016/j.genhosppsych.2005.07.003.
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52(1), 397–422. doi:10.1146/annurev.psych.52.1.397.
Mayfield, D., McLeod, G., & Hall, P. (1974). The CAGE questionnaire: validation of a new alcoholism screening instrument. American Journal of Psychiatry, 131(10), 1121–1123.
Mantzios, M. (2014). Exploring the relationship between worry and impulsivity in military recruits: the role of mindfulness and self‐compassion as potential mediators. Stress and Health, 30(5), 397–404. doi:10.1002/smi.2617.
McVicar, A. (2003). Workplace stress in nursing: a literature review. Journal of Advanced Nursing, 44(6), 633–642. doi:10.1046/j.0309-2402.2003.02853.x.
Mealer, M., Conrad, D., Evans, J., Jooste, K., Solyntjes, J., Rothbaum, B., & Moss, M. (2014). Feasibility and acceptability of a resilience training program for intensive care unit nurses. American Journal of Critical Care, 23(6), 97–105. doi:10.4037/ajcc2014747.
Potter, P., Deshields, T., Berger, J. A., Clarke, M., Olsen, S., & Chen, L. (2013). Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Forum, 40(2), 180–187. doi:10.1188/13.ONF.180-187.
Rees, C. S., Breen, L. J., Cusack, L., & Hegney, D. (2015). Understanding individual resilience in the workplace: the international collaboration of workforce resilience (ICWR) model. Frontiers in Psychology, 6, 73. doi:10.3389/fpsyg.2015.00073.
Ruths, F. A., de Zoysa, N., Frearson, S. J., Hutton, J., Williams, J. M. G., & Walsh, J. (2013). Mindfulness-based cognitive therapy for mental health professionals—a pilot study. Mindfulness, 4(4), 289–295. doi:10.1007/s12671-012-0127-0.
Santos, M. C., Barros, L., & Carolino, E. (2010). Occupational stress and coping resources in physiotherapists: a survey of physiotherapists in three general hospitals. Physiotherapy, 96(4), 303–310. doi:10.1016/j.physio.2010.03.001.
Samios, C., Abel, L. M., & Rodzik, A. K. (2013). The protective role of compassion satisfaction for therapists who work with sexual violence survivors: an application of the broaden-and-build theory of positive emotions. Anxiety, Stress, & Coping, 26(6), 610–623. doi:10.1080/10615806.2013.784278.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression. New York: The Guilford Press.
Sood, A., Prasad, K., Schroeder, D., & Varkey, P. (2011). Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. Journal of General Internal Medicine, 26(8), 858–861. doi:10.1007/s11606-011-1640-x.
Southwick, S. M., & Charney, D. S. (2012). Resilience: the science of mastering life’s greatest challenges. New York: Cambridge University Press, NY.
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R., & Jacobs, G. A. (1983). Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press.
Stamm, B. (2010). The Concise ProQOL Manual. In ProQoL.org (Ed.): Pocatello.
Swider, B., & Zimmerman, R. (2010). Born to burnout: a meta-analytic path model of personality, job burnout, and work outcomes. Journal of Vocational Behavior, 76(3), 487–506. doi:10.1016/j.jvb.2010.01.003.
Teper, R., Segal, Z. V., & Inzlicht, M. (2013). Inside the mindful mind: how mindfulness enhances emotion regulation through improvements in executive control. Current Directions in Psychological Science, 22(6), 449–454.
Thomas, J. T., & Otis, M. D. (2010). Intrapsychic correlates of professional quality of life: mindfulness, empathy, and emotional separation. Journal of the Society for Social Work and Research, 1(2), 83–98. http://www.jstor.org/stable/10.5243/jsswr.2010.7.
Thompson, R. W., Arnkoff, D. B., & Glass, C. R. (2011). Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma, Violence and Abuse, 12, 220–235. doi:10.1177/1524838011416375.
Tremblay, M. A., & Messervey, D. (2011). The job demands-resources model: further evidence for the buffering effect of personal resources. SA Journal of Industrial Psychology, 37(2), 10–19. doi:10.4102/sajip.v37i2.876.
Vallerand, R. J., Blanchard, C., Mageau, G. A., et al. (2003). Les passions de l’ame: on obsessive and harmonious passion. Journal of Personality and Social Psychology, 85(4), 756. doi:10.1037/0022-3514.85.4.756.
Vallerand, R. J., Paquet, Y., Philippe, F. L., & Charest, J. (2010). On the role of passion for work in burnout: a process model. Journal of Personality, 78(1), 289–312. doi:10.1111/j.1467-6494.2009.00616.x.
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., … & Piet, J. (2015). A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review, 37, 26–39. doi:10.1016/j.cpr.2015.02.001
Watson, D., & Clark, L. A. (1984). Negative affectivity: the disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. doi:10.1037/0033-2909.96.3.465.
Williams, J. M. G., & Penman, W. (2011). Mindfulness a practical guide to finding peace in a frantic world. London, UK: Piatkus.
Wolever, R. Q., Bobinet, K. J., McCabe, K., Mackenzie, E. R., Fekete, E., Kusnick, C. A., & Baime, M. (2012). Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. Journal of Occupational Health Psychology, 17(2), 246–258. doi:10.1037/a0027278.
Zeidner, M., Hadar, D., Matthews, G., & Roberts, R. D. (2013). Personal factors related to compassion fatigue in health professionals. Anxiety, Stress, & Coping, 26(6), 595–609. doi:10.1080/10615806.2013.777045.
Zeller, J. M., & Levin, P. F. (2013). Mindfulness interventions to reduce stress among nursing personnel: an occupational health perspective. Workplace Health & Safety, 61(2), 85–89. doi:10.1177/216507991306100207.
Acknowledgments
We acknowledge the work of Ms Sue Delhaize, MS Jan Low, and Ms Michelle Sin for assistance with recruitment and data collection. We also wish to acknowledge Ms Sue Davis, Nurse Director Corporate Nursing and the Nursing Executive Committee at the study hospital who funded the research and the International Collaboration for Workforce Resilience (ICWR-1). Finally, our thanks to the nurses who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval to conduct the study was obtained from the Sir Charles Gairdner Group Human Research Ethics Committee (HREC No: 2013-248) and Curtin University Human Research Ethics Committee (HR08/2014).
Funding
The study was funded internally at the study hospital.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 158 kb)
Rights and permissions
About this article
Cite this article
Craigie, M., Slatyer, S., Hegney, D. et al. A Pilot Evaluation of a Mindful Self-care and Resiliency (MSCR) Intervention for Nurses. Mindfulness 7, 764–774 (2016). https://doi.org/10.1007/s12671-016-0516-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-016-0516-x