Abstract
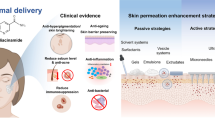
The drug delivery through the eye has been challenging due to the complex physiology of the eye. The ocular region is commonly considered the most advantageous site for the topical application of medicines for management of eye disorders. The effectiveness of this approach is commonly impeded by the strong protective mechanisms of eye, leading to restricted access of the drugs. Ocular fungal infections are commonly reported as one of the predominant eye illnesses caused by various fungal species like Fusarium species, Candida glabrata, Aspergillus flavus, and Aspergillus fumigatus. Liposomes are biocompatible lipid nanocarriers which have emerged as innovative therapeutic technologies in ophthalmology to overcome ocular obstacles, provide targeted drug delivery along with enhancement of drug’s safety margin. This review elucidates about causes of ocular fungal infection, fungal evasion by host immune system, pharmacological profile of drug used for treatment of ocular fungal infections, and challenges of existing formulations in management of ocular infections. This article focused upon the current advancements in domain of topical applications of liposomes of ophthalmic medicines in management of ocular fungal infection.


Similar content being viewed by others
Data Availability
No datasets were generated or analyzed during the current study.
Abbreviations
- AMB:
-
Amphotericin B
- AMCase:
-
Acidic mammalian chitinase
- DAmB:
-
Amphotericin B deoxycholate
- FLZ:
-
Fluconazole
- IL-1β:
-
Interleukin-1β
- L-AMB:
-
Liposomal amphotericin B
- MOP:
-
Microneedle ocular patch
- PAMPs:
-
Pathogen-associated molecular patterns
- PC:
-
Phosphatidylcholine
- PRR:
-
Pattern recognition receptors
References
Mishra, G. P., Bagui, M., Tamboli, V., & Mitra, A. K. (2011). Recent applications of liposomes in ophthalmic drug delivery. Journal of Drug Delivery, 2011.
Lai, S., Wei, Y., Wu, Q., Zhou, K., Liu, T., Zhang, Y., … Liu, Q. (2019). Liposomes for effective drug delivery to the ocular posterior chamber. Journal of Nanobiotechnology, 17, 1–12.
Garg, P. (2012). Fungal, mycobacterial, and Nocardia infections and the eye: An update. Eye (London, England), 26(2), 245–251.
Gower, E. W., Keay, L. J., Oechsler, R. A., Iovieno, A., Alfonso, E. C., Jones, D. B., … Lee, S. M. (2010). Trends in fungal keratitis in the United States, 2001 to 2007. Ophthalmology, 117(12), 2263–2267.
Srinivasan, M. (2004). Fungal keratitis. Current Opinion in Ophthalmology, 15(4), 321–327.
Mills, B., Radhakrishnan, N., Rajapandian, S. G. K., Rameshkumar, G., Lalitha, P., & Prajna, N. V. (2021). The role of fungi in fungal keratitis. Experimental Eye Research, 202, 108372.
Hariprasad, S. M., Mieler, W. F., Lin, T. K., Sponsel, W. E., & Graybill, J. R. (2008). Voriconazole in the treatment of fungal eye infections: A review of current literature. British Journal of Ophthalmology, 92(7), 871.
Sanap, S. N., Kedar, A., Bisen, A. C., Agrawal, S., & Bhatta, R. S. (2022). A recent update on therapeutic potential of vesicular system against fungal keratitis. Journal of Drug Delivery Science and Technology, 75, 103721.
Raj, N., Vanathi, M., Ahmed, N. H., Gupta, N., Lomi, N., & Tandon, R. (2021). Recent perspectives in the management of fungal keratitis. Journal of Fungi, 7(11), 907.
López-Cano, J. J., González-Cela-Casamayor, M. A., Andrés-Guerrero, V., Herrero-Vanrell, R., & Molina-Martínez, I. T. (2021). Liposomes as vehicles for topical ophthalmic drug delivery and ocular surface protection. Expert Opinion on drug Delivery, 18(7), 819–847.
Chang, E. H., Harford, J. B., Eaton, M. A. W., Boisseau, P. M., Dube, A., Hayeshi, R., … Lee, D. S. (2015). Nanomedicine: past, present and future–a global perspective. Biochemical and Biophysical Research Communications, 468(3), 511–517.
Wicki, A., Witzigmann, D., Balasubramanian, V., & Huwyler, J. (2015). Nanomedicine in cancer therapy: Challenges, opportunities, and clinical applications. Journal of Controlled Release, 200, 138–157.
Kumar, L., Verma, S., Bhardwaj, A., Vaidya, S., & Vaidya, B. (2014). Eradication of superficial fungal infections by conventional and novel approaches: A comprehensive review. Artificial Cells Nanomedicine and Biotechnology, 42(1), 32–46.
Soliman, G. M. (2017). Nanoparticles as safe and effective delivery systems of antifungal agents: Achievements and challenges. International Journal of Pharmaceutics, 523(1), 15–32.
Mueller, J. B., & McStay, C. M. (2008). Ocular infection and inflammation. Emergency Medicine Clinics of North America, 26(1), 57–72.
Klotz, S. A., Penn, C. C., Negvesky, G. J., & Butrus, S. I. (2000). Fungal and parasitic infections of the eye. Clinical Microbiology Reviews, 13(4), 662–685.
Atta, S., Perera, C., Kowalski, R. P., & Jhanji, V. (2022). Fungal keratitis: Clinical features, risk factors, treatment, and outcomes. Journal of Fungi, 8(9), 962.
Tabbara, K. F. (2014). Infections of the Lacrimal System. Ocular infections (pp. 45–49). Springer.
Sodhi, G., Liu, E., Renz, J., Heher, K., & Kapadia, M. (2016). Infections of the eyelids, orbit, and ocular adnexa. In N. Laver, & C. Specht (Eds.), The Infected Eye, 163–175.
Reginatto, P., Agostinetto, G. J., Fuentefria, R. N., Marinho, D. R., Pizzol, M. D., & Fuentefria, A. M. (2023). Eye fungal infections: A mini review. Archives of Microbiology, 205(6), 236.
Nayak, N. (2008). Fungal infections of the eye: Laboratory diagnosis and treatment. Nepal Medical College Journal : Nmcj, 10(1), 48–63.
Thomas, P. A., & Kaliamurthy, J. (2013). Mycotic keratitis: Epidemiology, diagnosis and management. Clinical Microbiology and Infection, 19(3), 210–220.
Maharana, P. K., Sharma, N., Nagpal, R., Jhanji, V., Das, S., & Vajpayee, R. B. (2016). Recent advances in diagnosis and management of mycotic keratitis. Indian Journal of Ophthalmology, 64(5), 346.
Qiao, G. L., Ling, J., Wong, T., Yeung, S. N., & Iovieno, A. (2020). Candida keratitis: Epidemiology, management, and clinical outcomes. Cornea, 39(7), 801–805.
Leck, A. K., Thomas, P. A., Hagan, M., Kaliamurthy, J., Ackuaku, E., John, M., … Kalavathy, C. M. (2002). Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. The British journal of ophthalmology, 86(11), 1211
Rai, M., Ingle, A. P., Ingle, P., Gupta, I., Mobin, M., Bonifaz, A., & Alves, M. (2021). Recent advances on mycotic keratitis caused by dematiaceous hyphomycetes. Journal of Applied Microbiology, 131(4), 1652–1667.
Durand, M. L. (2017). Bacterial and fungal endophthalmitis. Clinical Microbiology Reviews, 30(3), 597–613.
Sheu, S. J. (2017). Endophthalmitis. Korean Journal of Ophthalmology, 31(4), 283–289.
Mikosz, C. A., Smith, R. M., Kim, M., Tyson, C., Lee, E. H., Adams, E., … Grant-Greene, Y. (2014). Fungal endophthalmitis associated with compounded products. Emerging Infectious Diseases, 20(2), 248.
Park, H. J., Kim, S. H., Ju, H. W., Lee, H., Lee, Y., Park, S., … Yang, J. (2018). Microplasma jet arrays as a therapeutic choice for fungal keratitis. Scientific Reports, 8(1), 2422.
Farooq, A. V., Patel, R. M., Lin, A. Y., Setabutr, P., Sartori, J., & Aakalu, V. K. (2015). Fungal orbital cellulitis: Presenting features, management and outcomes at a referral center. Orbit, 34(3), 152–159.
Aimanianda, V., Bayry, J., Bozza, S., Kniemeyer, O., Perruccio, K., Elluru, S. R., … Kaveri, S. V. (2009). Surface hydrophobin prevents immune recognition of airborne fungal spores. Nature, 460(7259), 1117–1121.
Carrion, S. J., Leal, S. M., Ghannoum, M. A., Aimanianda, V., Latgé, J. P., & Pearlman, E. (2013). The rodA hydrophobin on aspergillus fumigatus spores masks dectin-1–and dectin-2–dependent responses and enhances fungal survival in vivo. The Journal of Immunology, 191(5), 2581–2588.
Fuchs, U., Czymmek, K. J., & Sweigard, J. A. (2004). Five hydrophobin genes in Fusarium verticillioides include two required for microconidial chain formation. Fungal Genetics and Biology, 41(9), 852–864.
Niu, L., Liu, X., Ma, Z., Yin, Y., Sun, L., Yang, L., & Zheng, Y. (2020). Fungal keratitis: Pathogenesis, diagnosis and prevention. Microbial Pathogenesis, 138, 103802.
Abbondante, S., Leal, S. M., Clark, H. L., Ratitong, B., Sun, Y., Ma, L. J., & Pearlman, E. (2023). Immunity to pathogenic fungi in the eye. Seminars in Immunology (Vol. 67, p. 101753). Elsevier.
Blango, M. G., Kniemeyer, O., & Brakhage, A. A. (2019). Conidial surface proteins at the interface of fungal infections. PLoS Pathogens, 15(9), e1007939.
Netea, M. G., Brown, G. D., Kullberg, B. J., & Gow, N. A. R. (2008). An integrated model of the recognition of Candida albicans by the innate immune system. Nature Reviews Microbiology, 6(1), 67–78.
Redfern, R. L., & McDermott, A. M. (2010). Toll-like receptors in ocular surface disease. Experimental eye Research, 90(6), 679–687.
Hardison, S. E., & Brown, G. D. (2012). C-type lectin receptors orchestrate antifungal immunity. Nature Immunology, 13(9), 817–822.
Yang, R.-B., Wu, L.-P., Lu, X.-X., Zhang, C., Liu, H., Huang, Y., … Zhao, S.-Z. (2021). Immunologic mechanism of fungal keratitis. International Journal of Ophthalmology, 14(7), 1100.
Brown, G. D. (2011). Innate antifungal immunity: The key role of phagocytes. Annual Review of Immunology, 29, 1–21.
Maneu, V., Yanez, A., Murciano, C., Molina, A., Gil, M. L., & Gozalbo, D. (2011). Dectin-1 mediates in vitro phagocytosis of Candida albicans yeast cells by retinal microglia. FEMS Immunology & Medical Microbiology, 63(1), 148–150.
Rubin-Bejerano, I., Abeijon, C., Magnelli, P., Grisafi, P., & Fink, G. R. (2007). Phagocytosis by human neutrophils is stimulated by a unique fungal cell wall component. Cell host & Microbe, 2(1), 55–67.
Sun, Y., Abbondante, S., Karmakar, M., de Jesus Carrion, S., Che, C., Hise, A. G., & Pearlman, E. (2018). Neutrophil caspase-11 is required for cleavage of caspase-1 and secretion of IL-1β in aspergillus fumigatus infection. The Journal of Immunology, 201(9), 2767–2775.
Bourgeois, C., Majer, O., Frohner, I. E., Lesiak-Markowicz, I., Hildering, K.-S., Glaser, W., … Müller, M. (2011). Conventional dendritic cells mount a type I IFN response against Candida spp. requiring novel phagosomal TLR7-mediated IFN-β signaling. The Journal of Immunology, 186(5), 3104–3112.
Karmakar, M., Katsnelson, M., Malak, H. A., Greene, N. G., Howell, S. J., Hise, A. G., … Pearlman, E. (2015). Neutrophil IL-1β processing induced by pneumolysin is mediated by the NLRP3/ASC inflammasome and caspase-1 activation and is dependent on K+ efflux. The Journal of Immunology, 194(4), 1763–1775.
Brissette-Storkus, C. S., Reynolds, S. M., Lepisto, A. J., & Hendricks, R. L. (2002). Identification of a novel macrophage population in the normal mouse corneal stroma. Investigative Ophthalmology & Visual Science, 43(7), 2264–2271.
Hamrah, P., & Dana, M. R. (2007). Corneal antigen-presenting cells. Immune Response and the Eye, 92, 58–70.
Mobeen, R., Stapleton, F., Chao, C., Madigan, M. C., Briggs, N., & Golebiowski, B. (2019). Corneal epithelial dendritic cell density in the healthy human cornea: A meta-analysis of in-vivo confocal microscopy data. The Ocular Surface, 17(4), 753–762.
Palomar, A. P., del, Montolío, A., Cegoñino, J., Dhanda, S. K., Lio, C. T., & Bose, T. (2019). The innate immune cell profile of the cornea predicts the onset of ocular surface inflammatory disorders. Journal of Clinical Medicine, 8(12), 2110.
Karmakar, M., Katsnelson, M., Malak, H. A., Greene, N. G., Howell, S. J., Hise, A. G., … Pearlman, E. (2015). Neutrophil IL-1β processing induced by pneumolysin is mediated by the NLRP3/ASC inflammasome and caspase-1 activation and is dependent on K+ efflux. The Journal of Immunology, 194(4), 1763–1775.
Leal Jr, S. M., Cowden, S., Hsia, Y. C., Ghannoum, M. A., Momany, M., & Pearlman, E. (2010). Distinct roles for Dectin-1 and TLR4 in the pathogenesis of aspergillus fumigatus keratitis. PLoS Pathogens, 6(7), e1000976.
Zhang, J., Zhao, G., Lin, J., Che, C., Li, C., Jiang, N., … Wang, Q. (2018). Role of PTX3 in corneal epithelial innate immunity against Aspergillus fumigatus infection. Experimental Eye Research, 167, 152–162.
de Jesus Carrion, S., Abbondante, S., Clark, H. L., Marshall, M. E., Mouyna, I., Beauvais, A., … Armstrong, B. (2019). Aspergillus fumigatus corneal infection is regulated by chitin synthases and by neutrophil–derived acidic mammalian chitinase. European journal of immunology, 49(6), 918–927.
Jin, X., Zhao, Y., Zhang, F., Wan, T., Fan, F., Xie, X., & Lin, Z. (2016). Neutrophil extracellular traps involvement in corneal fungal infection. Molecular Vision, 22, 944–952.
Brinkmann, V., Reichard, U., Goosmann, C., Fauler, B., Uhlemann, Y., Weiss, D. S., … Zychlinsky, A. (2004). Neutrophil extracellular traps kill bacteria. Science, 303(5663), 1532–1535.
Desai, J. V., & Lionakis, M. S. (2018). The role of neutrophils in host defense against invasive fungal infections. Current Clinical Microbiology Reports, 5, 181–189.
Lakhani, P., Patil, A., & Majumdar, S. (2019). Challenges in the polyene-and azole-based pharmacotherapy of ocular fungal infections. Journal of Ocular Pharmacology and Therapeutics, 35(1), 6–22.
Lewis, R. E. (2011). Current concepts in antifungal pharmacology. Mayo Clinic Proceedings (Vol. 86, pp. 805–817). Elsevier.
Gote, V., Sikder, S., Sicotte, J., & Pal, D. (2019). Ocular drug delivery: Present innovations and future challenges. Journal of Pharmacology and Experimental Therapeutics, 370(3), 602–624.
Mascarenhas, M., Chaudhari, P., & Lewis, S. A. (2023). Natamycin ocular delivery: Challenges and advancements in ocular therapeutics. Advances in Therapy, 40(8), 3332–3359.
Kaur, I. P., Rana, C., & Singh, H. (2008). Development of effective ocular preparations of antifungal agents. Journal of Ocular Pharmacology and Therapeutics, 24(5), 481–494.
Mehrandish, S., & Mirzaeei, S. (2021). A review on ocular novel drug delivery systems of antifungal drugs: Functional evaluation and comparison of conventional and novel dosage forms. Advanced Pharmaceutical Bulletin, 11(1), 28.
Mushtaq, A., Baseer, A., Zaidi, S. S., Khan, M. W., Batool, S., Elahi, E., … ud Din, F. (2022). Fluconazole-loaded thermosensitive system: In vitro release, pharmacokinetics and safety study. Journal of Drug Delivery Science and Technology, 67, 102972.
Farooq, M., Usman, F., Zaib, S., Shah, H. S., Jamil, Q. A., Akbar Sheikh, F., … El-Saber Batiha, G. (2022). Fabrication and evaluation of voriconazole loaded transethosomal gel for enhanced antifungal and antileishmanial activity. Molecules, 27(10), 3347.
Swaminathan, S., Sangwai, M., Wawdhane, S., & Vavia, P. (2013). Soluble itraconazole in tablet form using disordered drug delivery approach: Critical scale-up considerations and bio-equivalence studies. An Official Journal of the American Association of Pharmaceutical Scientists, 14, 360–374.
Nimtrakul, P., Williams, D. B., Tiyaboonchai, W., & Prestidge, C. A. (2020). Copolymeric micelles overcome the oral delivery challenges of amphotericin B. Pharmaceuticals, 13(6), 121.
Nikam, A. N., Jacob, A., Raychaudhuri, R., Fernandes, G., Pandey, A., Rao, V., … Mutalik, S. (2023). Topical Micro-Emulsion of 5-Fluorouracil by a Twin Screw Processor-Based Novel Continuous Manufacturing Process for the Treatment of Skin Cancer: Preparation and In Vitro and In Vivo Evaluations. Pharmaceutics, 15(9), 2175.
Bhandari, L., Patil, A. S., Bolmal, U., Masareddy, R., & Dandagi, P. (2022). Formulation and evaluation of natamycin solid dispersion incorporated ophthalmic films. Indian Journal of Pharmaceutical Education and Research, 56(1), 103–111.
Patil, A. ., Lakhani, P., Taskar, P., Avula, B., & Majumdar, S. (2020). Carboxyvinyl polymer and guar-borate gelling system containing natamycin loaded pegylated nanolipid carriers exhibit improved ocular pharmacokinetic parameters. Journal of Ocular Pharmacology and Therapeutics, 36(6), 410–420.
Chhonker, Y. S., Kumar, D., Shrivastava, P., Kumar, D., Singh, R., Chandasana, H., & Bhatta, R. S. (2013). LC–MS/MS assay for the determination of natamycin in rabbit and human plasma: Application to a pharmacokinetics and protein binding study. Journal of Pharmaceutical Analysis, 3(2), 144–148.
Meena, M., Prajapati, P., Ravichandran, C., & Sehrawat, R. (2021). Natamycin: a natural preservative for food applications—A review. Food Science and Biotechnology, 30, 1481–1496.
Hosoya, K., Lee, V. H. L., & Kim, K. J. (2005). Roles of the conjunctiva in ocular drug delivery: A review of conjunctival transport mechanisms and their regulation. European Journal of Pharmaceutics and Biopharmaceutics, 60(2), 227–240.
Patel, P., Shastri, D., Shelat, P., & Shukla, A. (2010). Ophthalmic drug delivery system: Challenges and approaches. Systematic Reviews in Pharmacy, 1(2), 113.
Chen, Y., Ye, Z., Chen, H., & Li, Z. (2024). Breaking barriers: Nanomedicine-based drug delivery for cataract treatment. International Journal of Nanomedicine 19, 4021–4040.
Akhter, M. H., Ahmad, I., Alshahrani, M. Y., Al-Harbi, A. I., Khalilullah, H., Afzal, O., … Karim, S. (2022). Drug delivery challenges and current progress in nanocarrier-based ocular therapeutic system. Gels, 8(2), 82.
Sahoo, S. K., Dilnawaz, F., & Krishnakumar, S. (2008). Nanotechnology in ocular drug delivery. Drug Discovery Today, 13(3–4), 144–151.
Wadhwa, S., Paliwal, R., Paliwal, S. R., & Vyas, S. P. (2009). Nanocarriers in ocular drug delivery: An update review. Current Pharmaceutical Design, 15(23), 2724–2750.
Din, F. U., Aman, W., Ullah, I., Qureshi, O. S., Mustapha, O., Shafique, S., & Zeb, A. (2017). Effective use of nanocarriers as drug delivery systems for the treatment of selected tumors. International Journal of Nanomedicine, 12, 7291–7309.
Bangham, A. D., Standish, M. M., & Watkins, J. C. (1965). Diffusion of univalent ions across the lamellae of swollen phospholipids. Journal of Molecular Biology, 13(1), 238-IN27.
Mainardes, R. M., Urban, M. C., Cinto, P. O., Khalil, N. M., Chaud, M. V., Evangelista, R. C., & Daflon Gremiao, M. P. (2005). Colloidal carriers for ophthalmic drug delivery. Current Drug Targets, 6(3), 363–371.
Jin, Q., Li, H., Jin, Z., Huang, L., Wang, F., Zhou, Y., … Wu, J. (2018). TPGS modified nanoliposomes as an effective ocular delivery system to treat glaucoma. International Journal of Pharmaceutics, 553(1–2), 21–28.
de Lima, P. H. C., Butera, A. P., Cabeça, L. F., & Ribeiro-Viana, R. M. (2021). Liposome surface modification by phospholipid chemical reactions. Chemistry and Physics of Lipids, 237, 105084.
Kaur, I. P., Garg, A., Singla, A. K., & Aggarwal, D. (2004). Vesicular systems in ocular drug delivery: An overview. International Journal of Pharmaceutics, 269(1), 1–14.
Habib, F. S., Fouad, E. A., Abdel-Rhaman, M. S., & Fathalla, D. (2010). Liposomes as an ocular delivery system of fluconazole: In-vitro studies. Acta Ophthalmologica, 88(8), 901–904.
Tan, G., Yu, S., Pan, H., Li, J., Liu, D., Yuan, K., … Pan, W. (2017). Bioadhesive chitosan-loaded liposomes: A more efficient and higher permeable ocular delivery platform for timolol maleate. International journal of biological macromolecules, 94, 355–363.
Agarwal, R., Iezhitsa, I., Agarwal, P., Abdul Nasir, N. A., Razali, N., Alyautdin, R., & Ismail, N. M. (2016). Liposomes in topical ophthalmic drug delivery: An update. Drug Delivery, 23(4), 1075–1091.
Mishra, A., Bano, M., Bisen, A. C., Verma, S., Sanap, S. N., Kishor, R., … Bhatta, R. S. (2020). Topical corneal targeted sustained release amphotericin B liposomal formulation for the treatment of fungal keratitis and its PK-PD evaluation. Journal of Drug Delivery Science and Technology, 60, 101944.
Jain, A. K., Chalasani, K. B., Khar, R. K., Ahmed, F. J., & Diwan, P. V. (2007). Muco-adhesive multivesicular liposomes as an effective carrier for transmucosal insulin delivery. Journal of drug Targeting, 15(6), 417–427.
Ebrahim, S., Peyman, G. A., & Lee, P. J. (2005). Applications of liposomes in ophthalmology. Survey of Ophthalmology, 50(2), 167–182.
Jensen, G. M. (2017). The care and feeding of a commercial liposomal product: Liposomal amphotericin B (AmBisome®). Journal of Liposome Research, 27(3), 173–179.
Sakai, D., Imai, H., & Nakamura, M. (2021). Multiple intravitreal liposomal amphotericin B for a case of Candida Glabrata Endophthalmitis. Case Reports in Ophthalmology, 12(2), 485–491.
Imago, M., Imai, H., Nakanishi, Y., & Azumi, A. (2009). Optical coherence tomography for monitoring the process of Candida Endophthalmitis. Acta Ophthalmologica, 87(6), 680–682.
Pappas, P. G., Kauffman, C. A., Andes, D. R., Clancy, C. J., Marr, K. A., Ostrosky-Zeichner, L., … Walsh, T. J. (2016). Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clinical Infectious Diseases, 62(4), e1–e50.
Axelrod, A. J., Peyman, G. A., & Apple, D. J. (1973). Toxicity of intravitreal injection of amphotericin B. American Journal of Ophthalmology, 76(4), 578–583.
Celenza, G., Iorio, R., Cracchiolo, S., Petricca, S., Costagliola, C., Cinque, B., … Bellio, P. (2020). Antimycotic Activity of Ozonized Oil in Liposome Eye Drops against Candida spp. Translational Vision Science & Technology, 9(8), 4.
Ando, T., Kawakami, H., Mochizuki, K., Murata, K., Manabe, Y., Takagi, D., … Ogura, S. (2021). Intraocular penetration of liposomal amphotericin B after intravenous injection in inflamed human eyes. Journal of Infection and Chemotherapy, 27(9), 1319–1322.
Ghosh, A. K., Rudramurthy, S. M., Gupta, A., Choudhary, H., Singh, S., Thakur, A., & Jatana, M. (2019). Evaluation of liposomal and conventional amphotericin B in experimental fungal keratitis rabbit model. Translational Vision Science & Technology, 8(3), 35.
Sanap, S. N., Bisen, A. C., Mishra, A., Biswas, A., Agrawal, S., Yadav, K. S., … Bhatta, R. S. (2022). QbD based antifungal drug-loaded ophthalmic liposomal formulation for the management of fungal keratitis: in vitro, ex vivo and in vivo pharmacokinetic studies. Journal of Drug Delivery Science and Technology, 74, 103517.
Salem, H. F., Ahmed, S. M., & Omar, M. M. (2016). Liposomal flucytosine capped with gold nanoparticle formulations for improved ocular delivery. Drug Design, Development and Therapy, 10, 277–295.
de Sá, F. A. P., Taveira, S. F., Gelfuso, G. M., Lima, E. M., & Gratieri, T. (2015). Liposomal voriconazole (VOR) formulation for improved ocular delivery. Colloids and Surfaces B: Biointerfaces, 133, 331–338.
Gelfuso, G. M., Ferreira-Nunes, R., Dalmolin, L. F., Re, A. C. dos S., Dos Santos, G. A., de Sá, F. A. P., … Anjos, J. L. V. (2020). Iontophoresis enhances voriconazole antifungal potency and corneal penetration. International Journal of Pharmaceutics, 576, 118991.
Leal, A. F. G., Leite, M. C., Medeiros, C. S. Q., Cavalcanti, I. M. F., Wanderley, A. G., Magalhães, S., N. S., & Neves, R. P. (2015). Antifungal activity of a liposomal itraconazole formulation in experimental aspergillus flavus keratitis with endophthalmitis. Mycopathologia, 179, 225–229.
Moustafa, M. A., Elnaggar, Y. S. R., El-Refaie, W. M., & Abdallah, O. Y. (2017). Hyalugel-integrated liposomes as a novel ocular nanosized delivery system of fluconazole with promising prolonged effect. International Journal of Pharmaceutics, 534(1–2), 14–24.
Moustafa, M. A., El-Refaie, W. M., Elnaggar, Y. S. R., & Abdallah, O. Y. (2018). Gel in core carbosomes as novel ophthalmic vehicles with enhanced corneal permeation and residence. International Journal of Pharmaceutics, 546(1–2), 166–175.
Roy, G., Galigama, R. D., Thorat, V. S., Mallela, L. S., Roy, S., Garg, P., & Venuganti, V. V. K. (2019). Amphotericin B containing microneedle ocular patch for effective treatment of fungal keratitis. International Journal of Pharmaceutics, 572, 118808.
Zhang, Z. H., Teng, F., Sun, Q. X., Wang, S. Z., Liu, C., & Zhao, G. Q. (2019). Rapamycin liposome gutta inhibiting fungal keratitis of rats. International Journal of Ophthalmology, 12(4), 536.
https://clinicaltrials.gov/. (https://clinicaltrials.gov/).
Jinzhong, Z., & Masaaki, K. (2018). Fungal keratitis prophylactic or therapeutic agent. CN108025000.
Mazumder, R., Swarupanjali Padhi, S., & Gupta, P. (2019). Glycerosomes of Natamycin for Treatment of Ophthalmic Fungal Keratitis. IN201911040868.
Chengye, C. H. E., & Leyu, L. Y. U. (2020). Application of secretoglobins in preparation of medicine for treating fungal keratitis. CN112057604.
Jin, Y., Xiaoxia, Z., Xuan, Z., Jing, Z., & Xin, Z. U. O. (2021). Medical material for treating fungal keratitis and preparation method thereof. CN112773778.
Weifen, Z., Xiuwen, G., Jinlong, M. A., Jingjing, Z., & Xiaoming, C. U. I. (2021). Contact lenses loaded with natamycin nanoparticles and preparation method thereof. CN112904590.
Guiqiu, Z., Cui, L. I., Daohao, L. I., Xudong, P., Kuiwen, S., & Qian, W. (2021). Voriconazole-coated carrageenan corneal contact lens and preparation method thereof. CN112999354.
Shengli, M. I., & Anyang, W. (2021). Ocular surface in-situ drug and preparation method thereof. CN113041215.
Guiqiu, Z., Cui, L. I., Daohao, L. I., Xudong, P., Jing, L. I. N., Min, Y. I. N., … Guibo, L. I. U. (2021). Natamycin-grafted oxidized alginic acid fiber membrane and preparation method thereof. CN113069556.
Cui, L. I., Guiqiu, Z., Daohao, L. I., Min, Y. I. N., Xudong, P., Chengye, C. H. E., & Zhaodong, D. U. (2021). Oxidized sodium alginate modified natamycin eye drops and preparation method thereof. CN113081956.
Jing, L. I. N., Guiqiu, Z., Xudong, P., Cui, L. I., Xing, L. I. U., & QIAN, W. (2021). Specific lectin-1 nano antibody as well as preparation method and application thereof. CN113354735.
Chengye, C. H. E., Qian, Z., & Leyu, L. Y. U. (2021). Application of C-type lectin-like receptor-1 as therapeutic marker of fungal keratitis. CN113156140.
Cui, L. I., Guiqiu, Z., Lingwen, G. U., Daohao, L. I., Nan, J., & Qiang, X. U. (2021). Nanometer mesoporous carbon eye drops loaded with natamycin and silver as well as preparation method and application thereof. CN113520997.
Ruibo, Y., Zhongwei, N. I. U., Xiaoyan, J. U., Shaozhen, Z., Ye, T., Liping, W. U., & Ning, G. A. O. (2021). Application of polysaccharide polypeptide conjugate in treatment of infectious keratitis. CN113577302.
Xiangrong, D. A. I., Lingzhen, D., Gang, L. I., & Xiaoyi, L. I. (2021). Voriconazole-containing ophthalmic gel as well as preparation method and application thereof. CN113662914.
Wal, P., Pandey, P., Singh, A., Pant, A., Gautam, A., Kr, D., Kushawah, D. K., Garg, D., Nivatya, H. K., Singh, H., Kumar, N., Kumar, P., & Rashmi, Sharma, V. (2022). A novel herbal microemulsion for ocular drug delivery. IN202211009279.
Cheng, L. I., Yi, H. A. N., Chenfang, X. U., & Yunlong, W. U. (2022). Amphotericin B nano-micelle as well as preparation method and application thereof. CN114788810.
Han, G. A. O. (2022). Preparation of glabridin eye-fixing medicine and application of glabridin eye-fixing medicine in treatment of fungal keratitis. CN114831936.
Olegovich, P. V., Nikolaevich, K. V., Leonidovich, T. V., & Andreevich, T. K. (2023). Drug for the treatment of resistant fungal keratitis and its method of use. RU0002790703.
Bhatta, R. S., Mishra, A., Sanap, S. N., Bisen, A., Verma, S., Kumar, M., Sharma, G., Shukla, S. K., Mugale, M. M., & Shukla, P. K. (2023). Polymeric liposomal formulation for keratitis. IN202111015517.
Sharma, U. K., Vishvakarma, P., Kumar, P., Dang, M., Dhurandhar, Y., Kumari, R., Antal, S., Mohapatra, L., Bhargava, J., Maurya, P., Tiwari, P., Srivastava, R., & Mandal, S. Non-irritating ocular nano emulsion with micafungin. IN202311024937.
Valeria, M., Vincenzo, P., Sudano, R. A., Donato, S., & Ilenia, A. (2023). Formulation based on polyhexamethylene biguanide for use in the treatment of acanthamoeba keratitis and/or fungal infections. EP4216966.
Boswell, G. W., Buell, D., & Bekersky, I. (1998). AmBisome (liposomal amphotericin B): a comparative review. The Journal of Clinical Pharmacology 38(7), 583–592.
Jadhav, M. P., Bamba, A., Shinde, V. M., Gogtay, N., Kshirsagar, N. A., Bichile, L. S., … Digumarathi, R. (2010). Liposomal amphotericin B (FungisomeTM) for the treatment of cryptococcal meningitis in HIV/AIDS patients in India: a multicentric, randomized controlled trial. Journal of postgraduate medicine, 56(2), 71–75.
Stone, N. R. H., Bicanic, T., Salim, R., & Hope, W. (2016). Liposomal amphotericin B (AmBisome®): A review of the pharmacokinetics, pharmacodynamics, clinical experience and future directions. Drugs, 76, 485–500.
Adler-Moore, J., & Proffitt, R. T. (2002). AmBisome: Liposomal formulation, structure, mechanism of action and pre-clinical experience. Journal of Antimicrobial Chemotherapy, 49(suppl_1), 21–30.
Sanath, S., Gogtay, N. J., & Kshirsagar, N. A. (2005). Post-marketing study to assess the safety, tolerability and effectiveness of FungisomeTM: An Indian liposomal amphotericin B Preparation. Journal of Postgraduate Medicine, 51(Suppl 1), S58–S63.
Acknowledgements
The authors would like to thank Department of Pharmaceutics, MM College of Pharmacy, Maharishi Markandeshwar (Deemed to be University), Mullana-Ambala, Haryana, India, 133207, for providing facilities for the completion of this review.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H.M., S.S., and N.S. conceived this study and wrote the final manuscript. L.K., M.D., and A.R. revised and edited this manuscript. H.M. and N.S. prepared figures.
Corresponding authors
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mehendiratta, H., Singh, S., Sharma, N. et al. Advances in Liposomes-Based-Therapeutics as Cutting-Edge for Ocular Fungal Infections: An Updated Review. BioNanoSci. (2024). https://doi.org/10.1007/s12668-024-01447-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s12668-024-01447-4