Abstract
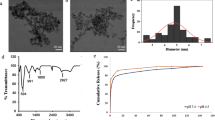
Magnetic nanoparticles (MNPs) could support the traditional brain cancer (e.g., glioblastoma) therapy; however, the efficient cell loading remains a crucial point. We aimed to relate the impact of the in vitro setup conditions to the long-term MNP loading of different glioblastoma cell lines. For this reason, three human glioblastoma and one astrocyte primary cell cultures were incubated with two different MNP types and various concentrations for 1–3 days. The resulting cellular iron load and cytotoxicity was determined. We found that the time dependence of the cell loading was governed by a variable cell growth behavior in vitro, whereas the impact of the MNP concentration was mostly MNP type-dependent. The growth as well as the membrane integrity of the cancer cells was not remarkably affected, but in astrocytes, although the metabolic activity was altered in all cell types. Consequently, we stated that the cell behavior and a comprehensive in vitro setup are key challenges for a proper design of MNPs and their medical application.







Similar content being viewed by others
References
Stupp, R., Mason, W. P., van den Bent, M. J., et al. (2005). Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. The New England Journal of Medicine, 352(10), 987–996. doi:10.1056/NEJMoa043330.
Maier-Hauff, K., Ulrich, F., Nestler, D., et al. (2011). Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. Journal of Neuro-Oncology, 103(2), 317–324. doi:10.1007/s11060-010-0389-0.
Chertok, B., David, A. E., Yang, V. C. (2011). Brain tumor targeting of magnetic nanoparticles for potential drug delivery: effect of administration route and magnetic field topography. Journal of controlled release, 155(3), 393–399.
Fu, A., Wilson, R. J., Smith, B. R., et al. (2012). Fluorescent magnetic nanoparticles for magnetically enhanced cancer imaging and targeting in living subjects. ACS Nano, 6(8), 6862–6869. doi:10.1021/nn301670a.
Shevtsov, M. A., Nikolaev, B. P., Yakovleva, L. Y., et al. (2015). Recombinant interleukin-1 receptor antagonist conjugated to superparamagnetic iron oxide nanoparticles for theranostic targeting of experimental glioblastoma. Neoplasia, 17(1), 32–42. doi:10.1016/j.neo.2014.11.001.
Stephen, Z. R., Kievit, F. M., Veiseh, O., et al. (2014). Redox-responsive magnetic nanoparticle for targeted convection-enhanced delivery of O6-benzylguanine to brain tumors. ACS Nano, 8(10), 10383–10395. doi:10.1021/nn503735w.
Kaluzova, M., Bouras, A., Machaidze, R., et al. (2015). Targeted therapy of glioblastoma stem-like cells and tumor non-stem cells using cetuximab-conjugated iron-oxide nanoparticles. Oncotarget, 6(11), 1–19.
Abakumov, M. A., Grinenko, N. F., Baklaushev, V. P., et al. (2012). Tumor-specific contrast agent based on ferric oxide superparamagnetic nanoparticles for visualization of gliomas by magnetic resonance tomography. Bulletin of Experimental Biology and Medicine, 153(1), 89–93.
Davda, J., & Labhasetwar, V. (2002). Characterization of nanoparticle uptake by endothelial cells. International Journal of Pharmaceutics, 233(1-2), 51–59. doi:10.1016/S0378-5173(01)00923-1.
Salvati, A., Åberg, C., dos Santos, T., et al. (2011). Experimental and theoretical comparison of intracellular import of polymeric nanoparticles and small molecules: toward models of uptake kinetics. Nanomed-Nanotechnol, 7(6), 818–826. doi:10.1016/j.nano.2011.03.005.
Kalambur, V. S., Longmire, E. K., Bischof, J. C. (2007). Cellular level loading and heating of superparamagnetic iron oxide nanoparticles. Langmuir, 23(24), 12329–12336. doi:10.1021/la701100r.
Jordan, A., Scholz, R., Wust, P., et al. (1999). Endocytosis of dextran and silan-coated magnetite nanoparticles and the effect of intracellular hyperthermia on human mammary carcinoma cells in vitro. Journal of Magnetism and Magnetic Materials, 194(1-3), 185–196. doi:10.1016/S0304-8853(98)00558-7.
Simpson, J., Horton, J., Scott, C., et al. (1993). Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive radiation therapy oncology group (RTOG) clinical trials. International journal of radiation oncology, 26(2), 239–244. doi:10.1016/0360-3016(93)90203-8.
Di Tomaso, E., Snuderl, M., Kamoun, W. S., et al. (2011). Glioblastoma recurrence after cediranib therapy in patients: lack of “rebound” revascularization as mode of escape. Cancer Research, 71(1), 19–28. doi:10.1158/0008-5472.CAN-10-2602.
Laurent, S., Burtea, C., Thirifays, C., et al. (2012). Crucial ignored parameters on nanotoxicology: the importance of toxicity assay modifications and “cell vision”. PloS One, 7(1), e29997. doi:10.1371/journal.pone.0029997.
Wilhelm, C., Gazeau, F., Roger, J., et al. (2002). Interaction of anionic superparamagnetic nanoparticles with cells: kinetic analyses of membrane adsorption and subsequent internalization. Langmuir, 18(21), 8148–8155. doi:10.1021/la0257337.
Weis, C., Blank, F., West, A., et al. (2014). Labeling of cancer cells with magnetic nanoparticles for magnetic resonance imaging. Magnetic Resonance in Medicine, 71(5), 1896–1905. doi:10.1002/mrm.24832.
Grudzinski, I. P., Bystrzejewski, M., Cywinska, M. A., et al. (2014). Comparative cytotoxicity studies of carbon-encapsulated iron nanoparticles in murine glioma cells. Colloids and Surfaces. B, 117, 135–143.
Berry, C. C., Wells, S., Charles, S., et al. (2003). Dextran and albumin derivatised iron oxide nanoparticles: influence on fibroblasts in vitro. Biomaterials, 24(25), 4551–4557. doi:10.1016/S0142-9612(03)00237-0.
Sun, Z., Yathindranath, V., Worden, M., et al. (2013). Characterization of cellular uptake and toxicity of aminosilane-coated iron oxide nanoparticles with different charges in central nervous system-relevant cell culture models (IJN: 961–970). doi:10.2147/IJN.S39048.
Das, G. K., Chan, P. P. Y., Teo, A., et al. (2009). In vitro cytotoxicity evaluation of biomedical nanoparticles and their extracts. Journal of Biomedical Materials Research, 9999, 337–346. doi:10.1002/jbm.a.32533.
Soenen, S. J., Himmelreich, U., Nuytten, N., et al. (2011). Cytotoxic effects of iron oxide nanoparticles and implications for safety in cell labelling. Biomaterials, 32(1), 195–205. doi:10.1016/j.biomaterials.2010.08.075.
Dringen, R., Bishop, G. M., Koeppe, M., et al. (2007). The pivotal role of astrocytes in the metabolism of iron in the brain. Neurochemical Research, 32(11), 1884–1890. doi:10.1007/s11064-007-9375-0.
Geppert, M., Hohnholt, M. C., Thiel, K., et al. (2011). Uptake of dimercaptosuccinate-coated magnetic iron oxide nanoparticles by cultured brain astrocytes. Nanotechnology, 22(14), 145101. doi:10.1088/0957-4484/22/14/145101.
Kress, G. J., Dineley, K. E., Reynolds, I. J. (2002). The relationship between intracellular free iron and cell injury in cultured neurons, astrocytes, and oligodendrocytes. Journal of Neuroscience, 22(14), 5848–5855.
Au, C., Mutkus, L., Dobson, A., et al. (2007). Effects of nanoparticles on the adhesion and cell viability on astrocytes. Biological Trace Element Research, 120(1-3), 248–256. doi:10.1007/s12011-007-0067-z.
Pickard, M. R., Jenkins, S. I., Koller, C. J., et al. (2011). Magnetic nanoparticle labeling of astrocytes derived for neural transplantation. Tissue Eng Pt C-Meth, 17(1), 89–99. doi:10.1089/ten.tec.2010.0170.
Bica, D., Vékás, L., Avdeev, M. V., et al. (2007). Sterically stabilized water based magnetic fluids: synthesis, structure and properties. Journal of Magnetism and Magnetic Materials, 311(1), 17–21. doi:10.1016/j.jmmm.2006.11.158.
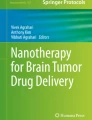
Avdeev, M. V., Mucha, B., Lamszus, K., et al. (2010). Structure and in vitro biological testing of water-based ferrofluids stabilized by monocarboxylic acids. Langmuir, 26(11), 8503–8509. doi:10.1021/la904471f.
Westphal, M., Hänsel, M., Hamel, W., et al. (1994). Karyotype analyses of 20 human glioma cell lines. Acta Neurochirurgica, 126(1), 17–26.
Riemer, J., Hoepken, H. H., Czerwinska, H., et al. (2004). Colorimetric ferrozine-based assay for the quantitation of iron in cultured cells. Analytical Biochemistry, 331(2), 370–375. doi:10.1016/j.ab.2004.03.049.
Safi, M., Courtois, J., Seigneuret, M., et al. (2011). The effects of aggregation and protein corona on the cellular internalization of iron oxide nanoparticles. Biomaterials, 32(35), 9353–9363. doi:10.1016/j.biomaterials.2011.08.048.
Kim, J. A., Åberg, C., Salvati, A., et al. (2011). Role of cell cycle on the cellular uptake and dilution of nanoparticles in a cell population. Nature Nanotechnology, 7(1), 62–68. doi:10.1038/nnano.2011.191.
Soenen, S. J. H., Nuytten, N., de Meyer, S. F., et al. (2010). High intracellular iron oxide nanoparticle concentrations affect cellular cytoskeleton and focal adhesion kinase-mediated signaling. Small, 6(7), 832–842. doi:10.1002/smll.200902084.
Geppert, M., Hohnholt, M. C., Nürnberger, S., et al. (2012). Ferritin up-regulation and transient ROS production in cultured brain astrocytes after loading with iron oxide nanoparticles. Acta Biomaterialia, 8(10), 3832–3839. doi:10.1016/j.actbio.2012.06.029.
Arbab, A. S., Bashaw, L. A., Miller, B. R., et al. (2003). Characterization of biophysical and metabolic properties of cells labeled with superparamagnetic iron oxide nanoparticles and transfection agent for cellular MR imaging1. Radiology, 229(3), 838–846. doi:10.1148/radiol.2293021215.
Kroll, A., Pillukat, M. H., Hahn, D., et al. (2012). Interference of engineered nanoparticles with in vitro toxicity assays. Archives of Toxicology, 86(7), 1123–1136. doi:10.1007/s00204-012-0837-z.
Legendre, C., & Garcion, E. (2015). Iron metabolism: a double-edged sword in the resistance of glioblastoma to therapies. Trends in Endocrinology and Metabolism, 26(6), 322–331. doi:10.1016/j.tem.2015.03.008.
Crichton, R. R., Wilmet, S., Legssyer, R., et al. (2002). Molecular and cellular mechanisms of iron homeostasis and toxicity in mammalian cells. Journal of Inorganic Biochemistry, 91(1), 9–18. doi:10.1016/S0162-0134(02)00461-0.
Le, N., & Richardson, D. R. (2002). The role of iron in cell cycle progression and the proliferation of neoplastic cells. BBA-Reviews Cancer, 1603(1), 31–46. doi:10.1016/S0304-419X(02)00068-9.
Kiessling, M. K., Klemke, C. D., Kaminski, M. M., et al. (2009). Inhibition of constitutively activated nuclear factor-B induces reactive oxygen species- and iron-dependent cell death in cutaneous T-cell lymphoma. Cancer Research, 69(6), 2365–2374. doi:10.1158/0008-5472.CAN-08-3221.
Acknowledgments
Dr. Ladislau Vékás from the Laboratory of Magnetic Fluids (Timisoara, Romania) kindly provided the MA used in this study and supported the study by discussions about the properties of MA. The authors want to thank Svenja Zapf for her assistance in cell culture and Heike Helmholz for the critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was funded by the Technology Transfer Fund of Helmholtz-Zentrum Geesthacht GmbH, which has no involvement in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
ESM 1
Suppl. Fig. 1 MNP loading of glioblastoma cell types and astrocytes. The means + standard deviations of MNP loading with 5, 25 or 50 μg/mL MA (A) or FS (B) for 1, 2 or 3 d, n = 6; *p < 0.05 compared with control, lines between the conditions, two-way ANOVA (Holm-Sidak post-hoc analysis). Suppl. Fig. 2 Cell counts after MNP loading. The means ± standard deviations of MNP loadings of glioblastom cell type and astrocytes, n = 6; #p < 0.05 compared with control, lines between the conditions, two-way ANOVA (Holm-Sidak post-hoc analysis). Suppl. Fig. 3 Time dependency of cell counts after MN. The means ± standard deviations of cell number in percent of control for all concentrations after 1, 2 or 3 d, n = 6. Suppl. Fig. 4 Correlation between Fe/cell and cell numbe sample was compared with the control mean ± standard deviation. Iron loads of samples with lower (loss), higher (gain) or similar (neutral) cell numbers were compared by ANOVA, horizontal lines indicate p < 0.05 Suppl. Fig. 5 Membrane integrity after MNP loading. The means ± standard deviations of the membrane integrity for glioblastoma cell types and astrocytes (Astro) for 5, 25 and 50 μg/mL and 1-3 d of incubation, n = 6, the lines between samples p < 0.05, two-way ANOVA (Holm-Sidak post post-hoc analysis). Suppl. Fig. 6 Metabolic activity after MNP loading. The means ± standard deviations of the metabolic activity for glioblastoma cells and astrocytes (Astro) for 5, 25 and 50 μg/mL and 1-3 d of incubation, n = 8, # p < 0.05 compared with control and lines between samples, two-way ANOVA (Holm Holm-Sidak post-hoc analysis). (PDF 2586 kb)
Rights and permissions
About this article
Cite this article
Scharfenberg, D., Luthringer, B., Lamszus, K. et al. Glioblastoma Cell Type-Specific Loading with Iron Oxide Magnetic Nanoparticles. BioNanoSci. 6, 297–307 (2016). https://doi.org/10.1007/s12668-016-0363-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-016-0363-1