Abstract
Objective
The goal of this study was to compare the stress distribution of three or four implants in the anterior region of the mandible that was grafted with a free vascularized fibula flap.
Methods
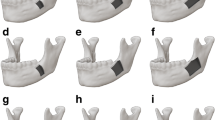
Two three-dimensional finite element models were designed based on cone-beam computed tomography of a patient whose anterior region of the mandible was restored with a free vascularized fibula flap. In both three- (G1) and four-implant (G2) models, the fixtures were connected with a fixed suprastructure. Occlusal loads were simulated using 300N.cm vertical and 50 N cm oblique forces. Implant micromotion and von Mises stress (VMS) distribution were measured. Inter-model comparisons were performed.
Results
Regarding vertical forces for G1 and G2, the supporting bone volume at maximum VMS was 2.44 mm3 and 3.04 mm3; the fixture volume undergoing maximum VMS was 160 mm3 and 175 mm3. For oblique forces, in the G1 and G2, respectively, the maximum VMS resulted in 7.09 mm3 and 7.73 mm3, and the fixture volume was 7.23 mm3 and 1.56 mm3. In G1, the most distal and middle implants showed the highest and lowest displacement; whereas in G2, the most distal implant displaced under vertical forces, showing the least micromotion under oblique loads. The inter-model comparison showed G2 had lower micromotion on average.
Conclusion
Employing the three-implant concept in rehabilitating the anterior region of a fibula-reconstructed mandible resulted in less VMS concentration under vertical and oblique forces; however, using four implants would be better for minimizing the fixture displacement. It is suggested new studies compare new scenarios matching different types of bone grafts and dental implants placed in the mandible and maxilla, trying to keep the heterogeneous complexity of the biomaterials to have better mimics and reality, increasing the reliability of the study.



Similar content being viewed by others
References
Borges H, Correia ARM, Castilho RM, Fernandes GVO (2020) Zirconia implants and marginal bone loss: a systematic review and meta-analysis of clinical studies. Int J Oral Maxillofac Implants 35(4):707–720. https://doi.org/10.11607/jomi.8097
Remísio MJS, Borges T, Castro F, Gehrke SA, Fernandes JCH, Fernandes GVO (2023) Histologic osseointegration level comparing titanium and zirconia dental implants: meta-analysis of preclinical Studies. Int J Oral Maxillofac Implants 38(4):667–680. https://doi.org/10.11607/jomi.10142
Fernandes GVO, Costa BMGN, Trindade HF, Castilho RM, Fernandes JCH (2022) Comparative analysis between extra-short implants (≤6 mm) and 6 mm-longer implants: a meta-analysis of randomized controlled trial. Aust Dent J 67(3):194–211. https://doi.org/10.1111/adj.12900
Farwell DG, Futran ND (2000) Oromandibular reconstruction. Facial Plast Surg 16(2):115–126
Kumar BP, Venkatesh V, Kumar KA, Yadav BY, Mohan SR (2016) Mandibular reconstruction: overview. J Maxillofac Oral Surg 15(4):425–441
Fernandes GVO, Castro F, Pereira RM, Teixeira W, Gehrke S, Joly JC, Carrion JB, Fernandes JCH (2023) Critical-size defects reconstruction with four different bone grafts associated with e-PTFE membrane: A histomorphometric experimental in vivo study. Clin Oral Impl Res. https://doi.org/10.1111/CLR.14210
Chiapasco M, Biglioli F, Autelitano L, Romeo E, Brusati R (2006) Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin Oral Implants Res 17(2):220–228
Latifi F, Tabrizi R, Hosseinikordkheili M (2023) How does the number of implants affect stress distribution in fibula graft at the posterior of the mandible? a finite element analysis. J Maxillofac Oral Surg 22(2):304–312. https://doi.org/10.1007/s12663-022-01743-0
Alqahtani AR, Desai SR, Patel JR, Alqhtani NR, Alqahtani AS, Heboyan A, Fernandes GVO, Mustafa M, Karobari MI (2023) Investigating the impact of diameters and thread designs on the Biomechanics of short implants placed in D4 bone: a 3D finite element analysis. BMC Oral Health 23(1):686. https://doi.org/10.1186/s12903-023-03370-8
Desai SR, Koulgikar KD, Alqhtani NR, Alqahtani AR, Alqahtani AS, Alenazi A, Heboyan A, Fernandes GVO, Mustafa M (2023) Three-dimensional FEA analysis of the stress distribution on titanium and graphene frameworks supported by 3 or 6-implant models. Biomimetics 8:15. https://doi.org/10.3390/biomimetics8010015
Gehrke SA, Dedavid BA, Fernandes GVO (2021) A new design of a multifunctional abutment to morse taper implant connection: experimental mechanical analysis. J Mechan Behavior Biomed Mat 116:104347. https://doi.org/10.1016/j.jmbbm.2021.104347
Chang Y, Tambe AA, Maeda Y, Wada M, Gonda T (2018) Finite element analysis of dental implants with validation: to what extent can we expect the model to predict biological phenomena? A literature review and proposal for classification of a validation process. Int J Implant Dent 4(1):7
Cepic LZ, Frank M, Reisinger A, Pahr D, Zechner W, Schedle A (2022) Biomechanical finite element analysis of short-implant-supported, 3-unit, fixed CAD/CAM prostheses in the posterior mandible. Int J Implant Dent 8:8. https://doi.org/10.1186/s40729-022-00404-8
Choi S-M, Choi H, Lee D-H, Hong M-H (2021) Comparative finite element analysis of mandibular posterior single zirconia and titanium implants: a 3-dimensional finite element analysis. J Adv Prosthodont 13(6):396–407. https://doi.org/10.4047/jap.2021.13.6.396
Pirjamalineisiani A, Sarafbidabad M, Jamshidi N, Esfahani FA (2017) Finite element analysis of post dental implant fixation in drilled mandible sites. Comput Biol Med 81:159–166. https://doi.org/10.1016/j.compbiomed.2016.11.012
Rho JY, Ashman RB, Turner CH (1993) Young’s modulus of trabecular and cortical bone material: ultrasonic and microtensile measurements. J Biomech 26(2):111–119
Nagasao T, Kobayashi M, Tsuchiya Y, Kaneko T, Nakajima T (2002) Finite element analysis of the stresses around endosseous implants in various reconstructed mandibular models. J Craniomaxillofac Surg 30(3):170–177
Park YS, Kwon HB (2013) Three-dimensional finite element analysis of implant-supported crown in fibula bone model. J Adv Prosthodont 5(3):326–332
Wu JC, Chen CS, Yip SW, Hsu ML (2012) Stress distribution and micromotion analyses of immediately loaded implants of varying lengths in the mandible and fibular bone grafts: a three-dimensional finite element analysis. Int J Oral Maxillofac Implants 27(5):e77-84
Walsh K, Jar C, Vafaeian B, Wolfaardt J, Aalto D, Adeeb S (2019) Use of patient-specific finite element models in dental rehabilitation to investigate stresses of a fibula free flap for mandibular reconstruction. Int J Oral Maxillofac Implants 34(3):e21–e31
Nesappan T, Ariga P (2014) Comparison of stresses around dental implants placed in normal and fibula reconstructed mandibular models using finite element analysis. J Clin Diagn Res 8(8):Zc45-50
Menicucci G, Mossolov A, Mozzati M, Lorenzetti M, Preti G (2002) Tooth-implant connection: some biomechanical aspects based on finite element analyses. Clin Oral Implants Res 13(3):334–341
Geng JP, Tan KB, Liu GR (2001) Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent 85(6):585–598
Papavasiliou G, Kamposiora P, Bayne SC, Felton DA (1997) 3D-FEA of osseointegration percentages and patterns on implant-bone interfacial stresses. J Dent 25(6):485–491
Eazhil R, Swaminathan SV, Gunaseelan M, Kannan GV, Alagesan C (2016) Impact of implant diameter and length on stress distribution in osseointegrated implants: a 3D FEA study. J Int Soc Prev Community Dent 6(6):590–596
Rosen EB, Kyle Gazdeck R, Goldman DA, Panchal H, Jones E, Nguyen JP et al (2022) An anatomic analysis of fibula flap mandible reconstructions: implications for endosseous implant placement. Plast Reconstr Surg 149(6):1419–1428
Sugiura T, Yamamoto K, Horita S, Murakami K, Kirita T (2018) Micromotion analysis of different implant configuration, bone density, and crestal cortical bone thickness in immediately loaded mandibular full-arch implant restorations: a nonlinear finite element study. Clin Implant Dent Relat Res 20(1):43–49
Shokri T, Stahl LE, Kanekar SG, Goyal N (2019) Osseous changes over time in free fibular flap reconstruction. Laryngoscope 129(5):1113–1116
Kumar VV, Ebenezer S, Kämmerer PW, Jacob PC, Kuriakose MA, Hedne N et al (2016) Implants in free fibula flap supporting dental rehabilitation—Implant and peri-implant related outcomes of a randomized clinical trial. J Craniomaxillofac Surg 44(11):1849–1858
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Latifi, F., Tabrizi, R., Kordkheili, M.H. et al. The Influence of Implant Number on Stress Distribution in the Anterior Region of Mandible Reconstructed with Fibula Bone Graft: A Finite Element Analysis. J. Maxillofac. Oral Surg. (2024). https://doi.org/10.1007/s12663-024-02162-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-024-02162-z