Abstract
Purpose
A nationwide shortage of oxytocin in Canada resulted in a temporary switch from oxytocin to carbetocin for all postpartum women at our institution. This change offered a unique opportunity to conduct a pragmatic comparative assessment of the efficacy of carbetocin and oxytocin.
Methods
In a retrospective before-after study, we reviewed the medical records from 641 women in the carbetocin group and 752 women in the oxytocin group . The standard carbetocin dosing was 100 µg iv following vaginal and intrapartum Cesarean delivery, while for elective Cesarean delivery it was 50 µg, with an additional 50 µg if required. The standard oxytocin dosing was 5 IU iv followed by 2.4 IU·hr-1 for four to six hours after vaginal delivery, while for Cesarean delivery it was 1–3 IU iv, three minutes apart, up to 10 IU if required, followed by the same maintenance. In both modalities of delivery, if uterine tone was suboptimal, the maintenance dose of oxytocin could be increased to 4.8 IU·hr-1. In both groups, additional uterotonics were used as required. The primary outcome was the need for additional uterotonics. Secondary outcomes included estimated and calculated blood loss, the occurrence of postpartum hemorrhage, and the need for blood transfusion.
Results
The incidence of additional uterotonic use was not different between the carbetocin and oxytocin groups (12.0% vs 8.8%; P = 0.05; odds ratio, 1.39; 95% confidence interval, 0.97 to 2.00). The incidence of postpartum hemorrhage was higher in the carbetocin group than in the oxytocin group (10.3% vs 6.6%; P = 0.01). Blood transfusion was more common in the carbetocin group (1.4% vs 0.3%; P = 0.02).
Conclusion
There was no difference in the use of additional uterotonics when carbetocin or oxytocin were used in a cohort of women undergoing vaginal deliveries and both elective and emergency Cesarean deliveries.
Résumé
Objectif
Une pénurie nationale d’ocytocine au Canada a entraîné l’utilisation temporaire de la carbétocine en remplacement de l’ocytocine pour toutes les femmes en post-partum dans notre établissement. Grâce à cette substitution, nous avons bénéficié d’une occasion unique de mener une évaluation comparative pragmatique de l’efficacité de la carbétocine et de l’ocytocine.
Méthode
Dans une étude rétrospective avant-après, nous avons examiné les dossiers médicaux de 641 femmes dans le groupe carbétocine et de 752 femmes dans le groupe ocytocine. Le dosage standard de carbécotine était de 100 μg iv après un accouchement vaginal et pendant un accouchement par césarienne intrapartum, tandis que pour un accouchement par césarienne élective, le dosage était de 50 μg, avec 50 μg supplémentaires au besoin. Le dosage standard d’ocytocine était de 5 UI iv suivi de 2,4 UI·h-1 pendant quatre à six heures après un accouchement vaginal, tandis que pour un accouchement par césarienne, il était de 1 à 3 UI iv, à trois minutes d’intervalle, jusqu’à 10 UI au besoin, suivi du même dosage d’entretien. Dans les deux types d’accouchement, si le tonus utérin était sous-optimal, la dose d’entretien d’ocytocine pouvait être augmentée à 4,8 UI·h-1. Dans les deux groupes, des utérotoniques supplémentaires ont été utilisés au besoin. Le critère d’évaluation principal était le besoin d’utérotoniques supplémentaires. Les critères d’évaluation secondaires comprenaient la perte de sang estimée et calculée, la survenue d’une hémorragie du post-partum et la nécessité d’une transfusion sanguine.
Résultats
L’incidence d’utilisation d’utérotoniques supplémentaires n’était pas différente entre les groupes carbétocine et ocytocine (12,0 % vs 8,8 %; P = 0,05; rapport de cotes,1,39; intervalle de confiance à 95 %, 0,97 à 2,00). L’incidence d’hémorragie du post-partum était plus élevée dans le groupe carbétocine que dans le groupe ocytocine (10,3 % vs 6,6 %; P = 0,01). Les transfusions sanguines étaient plus fréquentes dans le groupe carbétocine (1,4 % vs 0,3 %; P = 0,02).
Conclusion
Aucune différence dans l’utilisation d’utérotoniques supplémentaires n’a été observée lors de l’utilisation de carbétocine ou d’ocytocine dans une cohorte de femmes accouchant par voie vaginale ou par césarienne élective ou en urgence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Postpartum hemorrhage (PPH) is the most common cause of maternal mortality worldwide and accounts for nearly one-quarter of all maternal pregnancy-related deaths.1 It is most often a result of uterine atony, which occurs in at least 75% of PPH cases.2 Aside from increased mortality, increased rates of PPH can also increase maternal and neonatal morbidity via potential blood transfusion, increased length of hospital stay, and reduced ability to care for the newborns. Resource utilization may also be increased because of these factors.
Oxytocin is the most widely available and used uterotonic drug to prevent and treat PPH due to uterine atony.1 It binds to myometrial oxytocin receptors and stimulates uterine muscle contraction by increasing the intracellular calcium concentration.3,4 Nevertheless, oxytocin has a short half-life (3–17 min); as a result, a continuous intravenous infusion is necessary to maintain uterotonic activity.4,5,6 Moreover, large doses of oxytocin are associated with adverse effects such as hypotension, nausea, vomiting, tachycardia, arrhythmias, ST-T changes, pulmonary edema, water intoxication, and convulsions.5,7,8
Carbetocin (1-deamino-1-carba-2-tyrosine [O-methyl]-oxytocin) is a synthetic oxytocin analogue that binds to the myometrial oxytocin receptors with a similar affinity to oxytocin.3,4 Its main advantage over oxytocin is a four-fold longer half-life, which means there is no need for a continuous infusion.9,10 Carbetocin has been shown to reduce the need for additional uterotonics and the incidence of PPH compared with oxytocin, both in vaginal11,12,13 and Cesarean deliveries.8,14,15,16,17,18
An unprecedented, nationwide shortage of oxytocin in Canada in October–November 2019 prompted an acute and complete switch from oxytocin to carbetocin as the primary uterotonic drug for a finite period at our institution, for both vaginal and Cesarean deliveries. Carbetocin had seen minimal usage at our institution until then because it was not on formulary. Nevertheless, our obstetricians, anesthesiologists, and nurses were very familiar with the drug, given the many collaborative research projects involving carbetocin and oxytocin conducted over the years. Hence, all stakeholders promptly adhered to the change in practice without concerns.
This oxytocin shortage, and the resulting abrupt switch to carbetocin usage, presented a unique opportunity to compare oxytocin and carbetocin in both vaginal and Cesarean deliveries in a pragmatic before-after study, something not previously reported in the literature to date. We hypothesized that carbetocin would outperform oxytocin by reducing the use of additional uterotonics, the incidence of PPH, and the need for blood transfusion.
Methods
This study was approved by the Mount Sinai Hospital Research Ethics Board (REB 19-0334-C; approval date, 8 January 2020). This was a retrospective, single centre, before-after study comparing the efficacy of oxytocin and carbetocin as first line uterotonic drugs following both vaginal and Cesarean deliveries.
We identified the exact period of time when carbetocin became the primary postpartum uterotonic drug, which was between 10 October 2019 and 19 November 2019. Women delivering during this time had their medical records reviewed. We also reviewed medical records of a similar number of women who received oxytocin as the primary uterotonic during a similar period of time prior to oxytocin shortage (between 30 August 2019 and 10 October 2019). During the aforementioned periods of time, either oxytocin or carbetocin was the first-line uterotonic used for all women, irrespective of their mode of delivery, comorbidities, or risk factors for PPH.
We excluded women who had a planned Cesarean-hysterectomy, those undergoing induction of labour with misoprostol, those undergoing termination of pregnancy, and those recruited for an ongoing randomized controlled trial on uterotonic usage at our institution.
During both periods of time, the primary uterotonic drug—either oxytocin or carbetocin—was used as per institutional protocol. The standard dosing for oxytocin following vaginal delivery was 5 IU iv bolus followed by 20 IU·L-1 maintenance at a rate of 120 mL·hr-1 for four to six hours; if uterine tone was suboptimal, the maintenance solution could be changed to 40 IU·L-1 with the same infusion rate. In Cesarean deliveries, the intravenous bolus dose of oxytocin was titrated to uterine tone, 1–3 IU boluses, three minutes apart, up to 10 IU total dose, followed by 20 IU·L-1 maintenance infusion at a rate of 120 mL·hr-1; similarly, if uterine tone was suboptimal, the maintenance solution could be changed to 40 IU·L-1 with the same infusion rate. The standard carbetocin dosing following vaginal and intrapartum Cesarean deliveries was 100 μg iv. Women undergoing elective Cesarean deliveries received 50 μg iv bolus, and if required, an additional 50 μg bolus was used. In both vaginal and Cesarean deliveries, in cases where uterine tone was deemed unsatisfactory following the recommended doses of either oxytocin or carbetocin, additional uterotonic drugs such as ergonovine maleate, carboprost tromethamine, and misoprostol were used at the discretion of the attending obstetrician.
Demographic and obstetrical data were obtained for the purposes of characterizing the two groups.
Our primary outcome was the use of additional uterotonics (ergonovine, carboprost, or misoprostol). Secondary outcomes included estimated blood loss (EBL) and calculated blood loss (only for Cesarean deliveries), the occurrence of PPH, and the need for blood transfusion. Other outcomes of interest included interventions to treat PPH other than uterotonic drugs such as interventional radiology and surgical interventions.
Blood loss during Cesarean deliveries was calculated by measuring the hematocrit values before and 24 hr after Cesarean and using the following formula: EBV x (preoperative hematocrit − postoperative hematocrit)/preoperative hematocrit, where EBV is estimated blood volume (mL), which was calculated as the patient’s body weight x 85.19 Blood loss was also visually estimated by the obstetrician in both vaginal and Cesarean deliveries. We used the traditional definition for PPH, which is blood loss exceeding 500 mL following vaginal delivery and 1,000 mL following Cesarean delivery,20 given that this was still the definition used at our institution at the time.
All eligible women were distributed into two groups, carbetocin or oxytocin. Patient demographics, antepartum risk factors for PPH, and obstetric outcomes were compared between the two groups. Furthermore, we conducted a subgroup comparison for antepartum risk factors for PPH and obstetric outcomes in those women presenting with PPH. Frequency (percentage), mean (standard deviation [SD]) or median [interquartile range] are reported. We assessed differences between categorical variables with the Pearson Chi square test or, in instances of 25% of the cells having expected counts < 5, Fisher’s exact test; for comparisons between Gaussian or non-Gaussian continuous variables, we used Student’s t test or the Wilcoxon rank test, respectively. For the primary outcome, we applied univariate and multivariate logistic regression to assess the effects of risk factors. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) with a two-sided significance level of 0.05.
Results
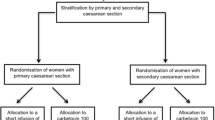
We reviewed the medical records of 827 women in the carbetocin group and 837 women in the oxytocin group for eligibility. After exclusion criteria were applied, 641 and 752 women were included in the analysis in the carbetocin and oxytocin groups, respectively (Figure). Patients’ demographics are presented in Table 1.
Antepartum risk factors for PPH in both groups are presented in Table 2. The incidences of women with history of previous uterine surgery, uterine fibroids, and chorioamnionitis were significantly higher in the carbetocin group.
The main obstetric outcomes for the entire cohort are shown in Table 3. Cesarean deliveries were more frequent in the carbetocin group, with no difference between the incidence of elective and intrapartum Cesarean deliveries. More women in the carbetocin group required a second uterotonic drug compared with those in the oxytocin group (12.0% vs 8.8%, respectively; P = 0.05). Mean (SD) EBL was higher in the carbetocin group for women with vaginal delivery (332 [172] mL vs 298 [149] mL; P = 0.003); however, there was no difference in estimated or calculated blood loss at Cesarean deliveries in both groups. The incidence of PPH was higher in the carbetocin group compared with the oxytocin group (10.3% vs 6.6%; P = 0.01). Nine women in the carbetocin group needed blood transfusion (1.4%) compared with two women (0.3%) in oxytocin group (P = 0.02).
Antepartum risk factors in PPH cases are shown in Table 4. There was no significant difference in antepartum risk factors between PPH cases from both study groups.
Obstetrical outcomes in PPH cases are shown in Table 5. There was no significant difference in the incidence of Cesarean and vaginal deliveries in both groups. Similarly, in this subset of women, there were no significant differences between both groups in the need for additional uterotonics, estimated or calculated blood loss, and blood transfusion.
The most common etiology for PPH in both groups was uterine atony. The incidence of uterine atony was significantly higher in the oxytocin group than in the carbetocin group (72.0% vs 53.0%; P = 0.03). Other possible etiologies for PPH were not significantly different between groups. There was no difference in PPH management between both groups. Postpartum complications were comparable in both groups, with only one patient (1.5%) in carbetocin group developing acute kidney injury that needed intensive care unit admission.
Table 6 shows the results of univariate and multivariate logistic regression (ORs and 95% CIs) applied to assess the effect of risk factors associated with our primary outcome. The use of additional uterotonics was not different between the oxytocin and carbetocin groups.
Discussion
To the best of our knowledge, this is the first pragmatic before-after study comparing carbetocin and oxytocin in both vaginal and Cesarean deliveries. This study was only possible because of a shortage of oxytocin in Canada, and the unique decision made at our institution to switch from oxytocin to carbetocin for all patients at once and revert back to oxytocin when availability had normalized.
Contrary to our hypothesis that carbetocin would outperform oxytocin, our results suggest that carbetocin and oxytocin are not different when assessed in a pragmatic way. The use of additional uterotonics, our primary outcome, was not different between the carbetocin and oxytocin groups.
It is important to highlight that our study assessed the efficacy of two uterotonic regimens, hence assessed both initiation and maintenance of uterine contraction. While the carbetocin regimen used a bolus of carbetocin to initiate and maintain uterine contraction, the oxytocin regimen used the drug as a bolus followed by maintenance infusion.
Our results are in keeping with a few studies that show similar efficacy for both drugs used during Cesarean delivery.14,21,22 Delorme et al.14 compared carbetocin and oxytocin for the prevention of PPH following Cesarean delivery and showed the non-superiority of carbetocin. The primary outcome was more than 2 g·dl-1 drop in hemoglobin level after delivery. Pizzagalli et al.21 compared carbetocin and oxytocin for the prevention of PPH following Cesarean delivery and observed no difference in effectiveness; their primary outcome was the difference between pre- and postoperative hematocrit in each group. Whigham et al.22 compared carbetocin and oxytocin at non-elective Cesarean deliveries and found no difference in the need for additional uterotonic drugs, EBL, change in hemoglobin values, or need for blood transfusion.
Our results are in contrast with several studies that show superiority of carbetocin while used both for Cesarean and vaginal deliveries.8,11,12,13,15,16,17,18,23 Dansereau et al.8 compared carbetocin and oxytocin for the prevention of uterine atony following elective Cesarean delivery. They showed that carbetocin was more effective than oxytocin as assessed by their primary outcome, which was the need for a second uterotonic drug. Holleboom et al.15 compared carbetocin and oxytocin in several dosing regimens for the prevention of uterine atony following elective Cesarean delivery and observed that carbetocin reduced the need for additional uterotonic drugs by more than 50%. In this study, however, most patients in the oxytocin group received only an oxytocin bolus without a maintenance infusion. This is not in keeping with the standard of practice in most institutions, where a bolus dose is followed by continuous infusion of oxytocin, given its short half-life. van der Nelson et al.16 compared carbetocin and oxytocin for prevention of PPH following Cesarean delivery and reported that carbetocin appears to improve clinical outcomes and save costs. Nevertheless, this study took efficacy data from a published Cochrane meta-analysis24 and there was a variability in method and dosing of oxytocin across different studies. Larciprete et al.17 compared carbetocin and oxytocin at Cesarean delivery in women at high risk of PPH and observed that carbetocin was more effective than continuous infusion of oxytocin at preventing PPH, although there was no significant difference in EBL or hemoglobin drop. They observed that more women were given additional uterotonic drugs in the oxytocin group. In this study, no oxytocin bolus was given, instead oxytocin was only given as a continuous infusion (20 IU·L-1 at a rate of 150 mL·hr-1). Widmer et al.11 compared carbetocin and oxytocin in the prevention of PPH following vaginal delivery and found that carbetocin was not inferior to oxytocin in preventing blood loss > 500 ml. Nevertheless, noninferiority was not shown for the outcome of blood loss > 1,000 mL. Maged et al.12 and Boucher et al.23 compared carbetocin and oxytocin following vaginal delivery and showed that carbetocin was superior in preventing PPH. The oxytocin dosing and the small sample size in both studies might have influenced their results. Boucher et al. administered (10 IU) of oxytocin as an infusion for two hours without any bolus while Maged et al. administered only a single 5 IU dose of oxytocin intramuscularly. On the other hand, the carbetocin dose in both studies was 100 μg intramuscularly. Amornpetchakul et al.13 compared carbetocin and oxytocin for the prevention of atonic PPH after vaginal delivery in women with singleton pregnancies and at least one risk factor for PPH. They found that intravenous carbetocin was more effective than intravenous oxytocin at preventing atonic PPH. In this study, oxytocin was administered as a bolus of 5 IU, without any maintenance infusion.
Gallos et al.25 have recently conducted a meta-analysis reviewing the efficacy of most commonly used uterotonic drugs in the prevention of PPH and showed that oxytocin-ergonovine combination, carbetocin, and oxytocin-misoprostol combination were more effective than oxytocin alone in preventing blood loss > 500 mL. In addition, an oxytocin- ergonovine combination was more effective than oxytocin alone in preventing blood loss > 1,000 mL. Of note, carbetocin had the most favourable side effect profile. Nevertheless, most carbetocin studies were small and at high risk of bias.
While our results are in contrast with most studies in the literature, we do not believe they are surprising. Although the literature suggests that carbetocin may be marginally superior to oxytocin, the evidence is weak.25 Most studies have compared carbetocin with oxytocin regimens that do not reflect the common practice and are not in keeping with the pharmacology of oxytocin (different doses, lack of oxytocin bolus dose, or lack of oxytocin infusion). As discussed by Gallos et al.,25 the literature comparing carbetocin and oxytocin carries a high risk of bias.
One may argue that the oxytocin and carbetocin regimens used in our study are different from the literature. They are, however, in keeping with best practices, as recommended by a recent international consensus on the use of uterotonics.26 The dose of 50 µg of carbetocin used at elective Cesarean deliveries, while different from most studies in the literature, is supported by a dose-finding study19 and a randomized controlled trial27 conducted by our group. If anything, the carbetocin dose used in this pragmatic before-after study was higher than that suggested by both studies19,27 and should have favoured the carbetocin group.
It is important to note that the differences observed between carbetocin and oxytocin in our study were only observed while comparing the entire cohort of women. When we compared only women with the diagnosis of PPH, we found the ante/intrapartum risk factors for PPH to be similar in both groups. Similarly, all the outcomes of interest, including primary and secondary outcomes, were similar in both groups. This likely is a direct consequence of the reduced sample size for those women presenting PPH.
Our study has some limitations. Given its pragmatic nature, we could not control the groups for ante/intrapartum risk factors for PPH. Overall, the carbetocin group had a higher incidence of women with previous uterine surgery, chorioamnionitis, and uterine fibroids, and such differences could have influenced the obstetrical outcomes. The univariate and multivariate analysis identified risk factors associated with our primary outcome, and some of these were more prevalent in the carbetocin group. Furthermore, given that the rate of uterine atony among women with PPH was substantially higher in the oxytocin group than in the carbetocin group, it is likely that this may, in part, explain the lack of effect of carbetocin.
In conclusion, our pragmatic before-after study suggests that when used according to our institutional protocol for both vaginal and Cesarean deliveries, carbetocin and oxytocin are not different. Nevertheless, given the confounders identified in this study, particularly the risk factors associated with PPH, our results should be interpreted with caution and further studies are warranted. Irrespective of its inherent limitations, this study offers a unique perspective into the comparison between carbetocin and oxytocin.
References
World Health Organization. Recommendations for the prevention and treatment of postpartum haemorrhage. WHO Press 2012.
Al-zirqi I, Vangen S, Forsen L, Stray-Pedersen B. Prevalence and risk factors of severe obstetric haemorrhage. Br J Obstet Gynaecol 2008; 115: 1265-72.
Barth T, Krejci I, Kupkova B, Jost K. Pharmacology of cyclic analogues of deamino-oxytocin not containing a disulphide bond (carba analogues). Eur J Pharmacol 1973; 24: 183-8.
Atke A, Vilhardt H. Uterotonic activity and myometrial receptor affinity of 1-deamino-1-carba-2-tyrosine(Omethyl)-oxytocin. Acta Endocrinol (Copenh) 1987; 115: 155-60.
Peters NC, Duvekot JJ. Carbetocin for the prevention of postpartum hemorrhage: a systematic review. Obstet Gynecol Surv 2009; 64: 129-35.
Rath W. Prevention of postpartum haemorrhage with the oxytocin analogue carbetocin. Eur J Obstet Gynecol Reprod Biol 2009; 147: 15-20.
Moran C, Ni Bhuinneain M, Geary M, Cunningham S, McKenna P, Gardiner J. Myocardial ischemia in normal patients undergoing elective caesarean section: a peripartum assessment. Anaesthesia 2001; 56: 1051-8.
Dansereau J, Joshi AK, Helewa ME, et al. Double-blind comparison of carbetocin versus oxytocin in prevention of uterine atony after cesarean section. Am J Obstet Gynecol 1999; 180(3 Pt 1): 670-6.
van Dongen PW, Verbruggen MM, de Groot AN, van Roosmalen J, Sporken JM, Schulz M. Ascending dose tolerance study of intramuscular carbetocin administered after normal vaginal birth. Eur J Obstet Gynecol Reprod Biol 1998; 77: 181-7.
Ferring Inc. Product monograph: Duratocin (Carbetocin Injection). Date of revision: FEB 21, 2020. Available from URL: https://www.ferring.ca/media/1253/eng-duratocin-vial-pm-eng-21feb2020.pdf (accessed September 2021).
Widmer M, Piaggio G, Nguyen TM, et al. Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med 2018; 379: 743-52.
Maged AM, Hassan AM, Shehata NA. Carbetocin versus oxytocin for prevention of postpartum hemorrhage after vaginal delivery in high risk women. J Matern Fetal Neonatal Med 2016; 29: 532-6.
Amornpetchakul P, Lertbunnaphong T, Boriboonhiransarn D, et al. Intravenous carbetocin versus intravenous oxytocin for preventing atonic postpartum hemorrhage after normal vaginal delivery in high-risk singleton pregnancies: a triple-blind randomized controlled trial. Arch Gynecol Obstet 2018; 29: 319-27.
Delorme P, Kayem G, Legardeur H, et al. Carbetocin versus oxytocin for the prevention of postpartum hemorrhage in cesarean deliveries: a retrospective study of two consecutive periods. AJP Rep 2020; 10: e241-6.
Holleboom CA, Van Eyck J, Koenen SV, et al. Carbetocin in comparison with oxytocin in several dosing regimens for the prevention of uterine atony after elective caesarean section in the Netherlands. Arch Gynecol Obstet 2013; 287: 1111-7.
van der Nelson HA, Draycott T, Siassakos D, Yau CW, Hatswell AJ. Carbetocin versus oxytocin for prevention of postpartum haemorrhage at caesarean section in the United Kingdom: an economic impact analysis. Eur J Obstet Gynecol Reprod Biol 2017; 210: 286-91.
Larciprete G, Montagnoli C, Frigo M, et al. Carbetocin versus oxytocin in caesarean section with high risk of post-partum haemorrhage. J Prenat Med 2013; 7: 12-8.
Voon HY, Suharjono HN, Shafie AA, Bujang MA. Carbetocin versus oxytocin for the prevention of postpartum hemorrhage: a meta-analysis of randomized controlled trials in cesarean deliveries. Taiwan J Obstet Gynecol 2018; 57: 332-9.
Khan M, Balki M, Ahmed I, Farine D, Seaward G, Carvalho JC. Carbetocin at elective cesarean delivery: a sequential allocation trial to determine the minimum effective dose. Can J Anesth 2014; 61: 242-8.
Rath WH. Postpartum hemorrhage--update on problems of definitions and diagnosis. Acta Obstet Gynecol Scand 2011; 90: 421-8.
Pizzagalli F, Agasse J, Marpeau L, et al. Carbetocin versus oxytocin during caesarean section for preventing postpartum haemorrhage (French). Gynecol Obstet Fertil 2015; 43: 356-60.
Whigham CA, Gorelik A, Loughnan TA, Trivedi A. Carbetocin versus oxytocin to reduce additional uterotonic use at non-elective cesarean section: a double-blind, randomised trial. J Matern Fetal Neonatal Med 2016; 29: 3866-9.
Boucher M, Nimrod CA, Tawagi GF, et al. Comparison of carbetocin and oxytocin for the prevention of postpartum hemorrhage following vaginal delivery: a double-blind randomized trial. Am J Obstet Gynaecol Can 2004; 26: 481-8.
Su LL, Chong YS, Samuel M. Carbetocin for preventing postpartum haemorrhage. Cochrane Database Syst Rev 2012; DOI: https://doi.org/10.1002/14651858.CD005457.pub3.
Gallos ID, Williams HM, Price MJ, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev 2018; DOI: https://doi.org/10.1002/14651858.CD011689.pub2.
Heesen M, Carvalho B, Carvalho JC, et al. International consensus statement on the use of uterotonic agents during caesarean section. Anaesthesia 2019; 74: 1305-19.
Tabl S, Balki M, Downey K, et al. Uterotonics in elective caesarean delivery: a randomised non-inferiority study comparing carbetocin 20 μg and 100 μg. Anaesthesia 2019; 74: 190-6.
Author contributions
Ahmad Ben Tareef, Kristi Downey, and Jose C.A. Carvalho contributed to study conception and interpretation of data. Ahmad Ben Tareef, Kristi Downey, Wendy L. Whittle, and Jose C.A. Carvalho contributed to study design. Ahmad Ben Tareef, Kristi Downey, and Bernard Ma contributed to research conduct and acquisition of data. Ahmad Ben Tareef and Jose C.A. Carvalho contributed to drafting the manuscript.
Disclosures
None.
Funding statement
This study was funded internally by the Department of Anesthesia and Pain Management, Mount Sinai Hospital. Jose C.A. Carvalho MD, PhD is sponsored by the Merit Awards Program from the Department of Anesthesiology and Pain Medicine, University of Toronto.
Editorial responsibility
This submission was handled by Dr. Ronald George, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben Tareef, A., Downey, K., Ma, B. et al. Carbetocin versus oxytocin following vaginal and Cesarean delivery: a before-after study. Can J Anesth/J Can Anesth 69, 97–105 (2022). https://doi.org/10.1007/s12630-021-02127-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02127-7