Abstract
Objectives
Frailty is a pervasive condition among older people worldwide. Despite the association between higher protein intake and lower frailty risk has been well documented, older individuals encounter barriers to enhancing their protein consumption due to reduced appetite and impaired digestive capacity. This study aims to delve into the potential correlation between dietary protein diversity, protein patterns, and the risk of frailty among older Chinese individuals.
Design
Prospective cohort study.
Setting
Community-based.
Participants
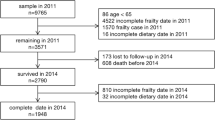
2,216 participants aged 65 and above and not frail at the baseline were recruited from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) dataset spanning from 2014 to 2018.
Measurements
Dietary protein diversity was evaluated utilizing a protein diversity score (PDS), calculated based on the results of a food frequency questionnaire. Dietary protein patterns were identified by employing principal component analysis (PCA). Frailty was ascertained using a 40-item frailty index (FI) where FI > 0.21 indicated frailty. Logistic analysis was employed to investigate the association between dietary variables and frailty.
Results
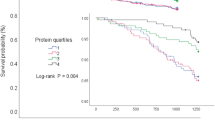
541 participants were identified as frail after a 4-year follow-up. After adjusting for confounders, each 1-unit increase in PDS was linked to a 10% decrease in frailty risk. Compared to individuals with PDS ≤ 1, those with PDS scores of 2–3, 4–5, and 6 had lower risks of frailty, with OR (95% CI) of 0.78 (0.58–1.06), 0.58 (0.38–0.87), 0.42 (0.20–0.81), respectively (P trend = 0.038). Individuals who consistently maintained high PDS demonstrated a lower frailty risk in contrast to those who maintained low PDS (OR = 0.60, 95% CI, 0.41–0.87). Additionally, the “meat-fish” pattern exhibited a protective association with frailty, with OR Q4 versus Q1 (95% CI) of 0.54 (0.40–0.74), P trend < 0.001.
Conclusion
Maintaining a variety of dietary protein sources and following a “meat-fish” protein pattern might decrease the likelihood of frailty among the older Chinese population.

Similar content being viewed by others
References
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi:https://doi.org/10.1093/gerona/56.3.m146.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013; 381: 752–62.
Middleton R, Poveda JL, Orfila Pernas F, et al. Mortality, Falls, and Fracture Risk Are Positively Associated With Frailty: A SIDIAP Cohort Study of 890,000 Patients. J Gerontol A Biol Sci Med Sci. 2022;77(1):148–154. doi:https://doi.org/10.1093/gerona/glab102.
Kojima G, Iliffe S, Jivraj S, Walters K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(7):716–721. doi:https://doi.org/10.1136/jech-2015-206717.
Liu M, Hou T, Nkimbeng M, et al. Associations between symptoms of pain, insomnia and depression, and frailty in older adults: A cross-sectional analysis of a cohort study. Int J Nurs Stud. 2021;117:103873. doi:https://doi.org/10.1016/j.ijnuretu.2021.103873.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727. doi:https://doi.org/10.1093/gerona/62.7.722.
Yannakoulia M, Ntanasi E, Anastasiou CA, Scarmeas N. Frailty and nutrition: From epidemiological and clinical evidence to potential mechanisms. Metabolism. 2017;68:64–76. doi:https://doi.org/10.1016/j.metabol.2016.12.005.
Konglevoll DM, Hjartåker A, Hopstock LA, et al. Protein Intake and the Risk of Pre-Frailty and Frailty in Norwegian Older Adults. The Tromsø Study 1994–2016. J Frailty Aging. 2022;11(3):256–266. doi:https://doi.org/10.14283/jfa.2022.16.
Mendonça N, Kingston A, Granic A, Jagger C. Protein intake and transitions between frailty states and to death in very old adults: the Newcastle 85+ study. Age Ageing. 2019;49(1):32–38. doi:https://doi.org/10.1093/ageing/afz142.
Coelho-Junior HJ, Calvani R, Picca A, Tosato M, Landi F, Marzetti E. Protein Intake and Frailty in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2022;14(13):2767. doi:https://doi.org/10.3390/nu14132767.
Coelho-Junior HJ, Marzetti E, Picca A, Cesari M, Uchida MC, Calvani R. Protein Intake and Frailty: A Matter of Quantity, Quality, and Timing. Nutrients. 2020;12(10):2915. doi:https://doi.org/10.3390/nu12102915.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. doi:https://doi.org/10.1016/S0140-6736(19)31785-4.
Landi F, Calvani R, Tosato M, et al. Protein Intake and Muscle Health in Old Age: From Biological Plausibility to Clinical Evidence. Nutrients. 2016;8(5):295. doi:https://doi.org/10.3390/nu8050295.
Keller HH. Promoting food intake in older adults living in the community: a review. Appl Physiol Nutr Metab. 2007;32(6):991–1000. doi:https://doi.org/10.1139/H07-067.
Zhou C, Wu Q, Ye Z, et al. Inverse Association Between Variety of Proteins With Appropriate Quantity From Different Food Sources and New-Onset Hypertension. Hypertension. 2022;79(5):1017–1027. doi:https://doi.org/10.1161/HYPERTENSIONAHA.121.18222.
Zhou C, Liu C, Zhang Z, et al. Variety and quantity of dietary protein intake from different sources and risk of new-onset diabetes: a Nationwide Cohort Study in China. BMC Med. 2022;20(1):6. doi:https://doi.org/10.1186/s12916-021-02199-8.
Isanejad M, Sirola J, Rikkonen T, et al. Higher protein intake is associated with a lower likelihood of frailty among older women, Kuopio OSTPRE-Fracture Prevention Study. Eur J Nutr. 2020;59(3):1181–1189. doi:https://doi.org/10.1007/s00394-019-01978-7.
Struijk EA, Fung TT, Rodríguez-Artalejo F, et al. Protein intake and risk of frailty among older women in the Nurses’ Health Study. J Cachexia Sarcopenia Muscle. 2022;13(3):1752–1761. doi:https://doi.org/10.1002/jcsm.12972
Zeng Y, Feng Q, Gu D, Vaupel JW. Demographics, phenotypic health characteristics and genetic analysis of centenarians in China. Mech Ageing Dev. 2017;165(Pt B):86–97. doi:https://doi.org/10.1016/j.mad.2016.12.010
Yi Z. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS). In: Yi Z, Poston DL, Vlosky DA, Gu D, editors. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Dordrecht: Springer Netherlands; 2008. pp. 23–38.
Lv X, Sun S, Wang J, et al. Anti-Inflammatory Dietary Diversity and Depressive Symptoms among Older Adults: A Nationwide Cross-Sectional Analysis. Nutrients. 2022;14(23):5062. doi:https://doi.org/10.3390/nu14235062
Yin Z, Fei Z, Qiu C, et al. Dietary Diversity and Cognitive Function among Elderly People: A Population-Based Study. J Nutr Health Aging. 2017;21(10):1089–1094. doi:https://doi.org/10.1007/s12603-017-0912-5
Wang XM, Zhong WF, Li ZH, et al. Dietary diversity and frailty among older Chinese people: evidence from the Chinese Longitudinal Healthy Longevity Study. Am J Clin Nutr. 2023;117(2):383–391. doi:https://doi.org/10.1016/j.ajcnut.2022.11.017.
Kennedy G, Ballard T, Dop MC. Guidelines for measuring household and individual dietary diversity. Food and Agriculture Organization of the United Nations; 2011. p26.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. doi:https://doi.org/10.1186/1471-2318-8-24.
Chen CL, Cai AP, Nie ZQ, Huang YQ, Feng YQ. Systolic Blood Pressure and Mortality in Community-Dwelling Older Adults: The Role of Frailty. J Nutr Health Aging. 2022;26(10):962–970. doi:https://doi.org/10.1007/s12603-022-1850-4
Liu ZY, Wei YZ, Wei LQ, et al. Frailty transitions and types of death in Chinese older adults: a population-based cohort study. Clin Interv Aging. 2018;13:947–956. doi:https://doi.org/10.2147/CIA.S157089
Hoover M, Rotermann M, Sanmartin C, Bernier J. Validation of an index to estimate the prevalence of frailty among community-dwelling seniors. Health Rep. 2013;24(9):10–17.
Zheng J, Zhou R, Li F, et al. Association between dietary diversity and cognitive impairment among the oldest-old: Findings from a nationwide cohort study. Clin Nutr. 2021;40(4):1452–1462. doi:https://doi.org/10.1016/j.clnu.2021.02.041
Gao J, Wang Y, Xu J, Jiang J, Yang S, Xiao Q. Life expectancy among older adults with or without frailty in China: multistate modelling of a national longitudinal cohort study. BMC Med. 2023;21(1):101. doi:https://doi.org/10.1186/s12916-023-02825-7
Nanri H, Yamada Y, Yoshida T, et al. Sex Difference in the Association Between Protein Intake and Frailty: Assessed Using the Kihon Checklist Indexes Among Older Adults. J Am Med Dir Assoc. 2018;19(9):801–805. doi:https://doi.org/10.1016/j.jamda.2018.04.005.
Sandoval-Insausti H, Pérez-Tasigchana RF, López-García E, García-Esquinas E, Rodríguez-Artalejo F, Guallar-Castillón P. Macronutrients Intake and Incident Frailty in Older Adults: A Prospective Cohort Study. J Gerontol A Biol Sci Med Sci. 2016;71(10):1329–1334. doi:https://doi.org/10.1093/gerona/glw033.
Wu SY, Yeh NH, Chang HY, et al. Adequate protein intake in older adults in the context of frailty: cross-sectional results of the Nutrition and Health Survey in Taiwan 2014–2017. Am J Clin Nutr. 2021;114(2):649–660. doi:https://doi.org/10.1093/ajcn/nqab070.
Beasley JM, LaCroix AZ, Neuhouser ML, et al. Protein intake and incident frailty in the Women’s Health Initiative observational study. J Am Geriatr Soc. 2010;58(6):1063–1071. doi:https://doi.org/10.1111/j.1532-5415.2010.02866.x.
Rahi B, Colombet Z, Gonzalez-Colaço Harmand M, et al. Higher Protein but Not Energy Intake Is Associated With a Lower Prevalence of Frailty Among Community-Dwelling Older Adults in the French Three-City Cohort. J Am Med Dir Assoc. 2016;17(7):672.e7–672.e11. doi:https://doi.org/10.1016/j.jamda.2016.05.005.
Cruz-Jentoft AJ, Michel JP. Sarcopenia: A useful paradigm for physical frailty. European Geriatric Medicine, 2013, 4(2):102–105. doi:https://doi.org/10.1016/j.eurger.2013.02.009.
Houston DK, Nicklas BJ, Ding J, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87(1):150–155.
Bollwein J, Diekmann R, Kaiser MJ, et al. Distribution but not amount of protein intake is associated with frailty: a cross-sectional investigation in the region of Nürnberg. Nutr J. 2013;12:109. doi:https://doi.org/10.1186/1475-2891-12-109.
Huang WC, Huang YC, Lee MS, Doong JY, Pan WH, Chang HY. The Combined Effects of Dietary Diversity and Frailty on Mortality in Older Taiwanese People. Nutrients. 2022;14(18):3825. doi:https://doi.org/10.3390/nu14183825.
Duan Y, Qi Q, Cui Y, Yang L, Zhang M, Liu H. Effects of dietary diversity on frailty in Chinese older adults: a 3-year cohort study. BMC Geriatr. 2023;23(1):141. doi:https://doi.org/10.1186/s12877-023-03875-5
Yokoro M, Otaki N, Yano M, et al. Low Dietary Variety Is Associated with Incident Frailty in Older Adults during the Coronavirus Disease 2019 Pandemic: A Prospective Cohort Study in Japan. Nutrients. 2023;15(5):1145. doi:https://doi.org/10.3390/nu15051145.
Motokawa K, Watanabe Y, Edahiro A, et al. Frailty Severity and Dietary Variety in Japanese Older Persons: A Cross-Sectional Study. J Nutr Health Aging. 2018;22(3):451–456. doi:https://doi.org/10.1007/s12603-018-1000-1.
Zhang J, Wang Q, Hao W, Zhu D. Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018. Nutrients. 2022;14(20):4279. doi:https://doi.org/10.3390/nu14204279.
Gorissen SHM, Crombag JJR, Senden JMG, et al. Protein content and amino acid composition of commercially available plant-based protein isolates. Amino Acids. 2018;50(12):1685–1695. doi:https://doi.org/10.1007/s00726-018-2640-5.
Dimina L, Rémond D, Huneau JF, Mariotti F. Combining Plant Proteins to Achieve Amino Acid Profiles Adapted to Various Nutritional Objectives-An Exploratory Analysis Using Linear Programming. Front Nutr. 2022;8:809685. doi:https://doi.org/10.3389/fnut.2021.809685.
Zhou C, Yang S, Zhang Y, et al. Relations of Variety and Quantity of Dietary Proteins Intake from Different Sources with Mortality Risk: A Nationwide Population-Based Cohort. J Nutr Health Aging. 2022;26(12):1078–1086. doi:https://doi.org/10.1007/s12603-022-1870-0.
Konglevoll DM, Andersen LF, Hopstock LA, et al. Fish intake and pre-frailty in Norwegian older adults - a prospective cohort study: the Tromsø Study 1994–2016. BMC Geriatr. 2023;23(1):411. Published 2023 Jul 5. doi:https://doi.org/10.1186/s12877-023-04081-z.
Lord C, Chaput JP, Aubertin-Leheudre M, et al. Dietary animal protein intake: association with muscle mass index in older women. J Nutr Health Aging. 2007;11:383–387.
Gorissen SHM, Witard OC. Characterising the muscle anabolic potential of dairy, meat and plant-based protein sources in older adults. Proc Nutr Soc. 2018;77(1):20–31. doi:https://doi.org/10.1017/S002966511700194X.
Moughan PJ, Wolfe RR. Determination of Dietary Amino Acid Digestibility in Humans. J Nutr. 2019;149(12):2101–2109. doi:https://doi.org/10.1093/jn/nxz211.
Lee S, Choi YS, Jo K, Yong HI, Jeong HG, Jung S. Improvement of meat protein digestibility in infants and the elderly. Food Chem. 2021;356:129707. doi:https://doi.org/10.1016/j.foodchem.2021.129707
Gupta YP. Anti-nutritional and toxic factors in food legumes: a review. Plant Foods Hum Nutr. 1987;37(3):201–228. doi:https://doi.org/10.1007/BF01091786.
Verlaan S, Aspray TJ, Bauer JM, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: A case-control study. Clin Nutr. 2017;36(1):267–274. doi:https://doi.org/10.1016/j.clnu.2015.11.013.
Ates Bulut E, Soysal P, Aydin AE, Dokuzlar O, Kocyigit SE, Isik AT. Vitamin B12 deficiency might be related to sarcopenia in older adults. Exp Gerontol. 2017;95:136–140. doi:https://doi.org/10.1016/j.exger.2017.05.017.
Higashida K, Inoue S, Nakai N. Iron deficiency attenuates protein synthesis stimulated by branched-chain amino acids and insulin in myotubes. Biochem Biophys Res Commun. 531(2):112–117. doi: https://doi.org/10.1016/j.bbrc.2020.07.041.
Soto ME, Pérez-Torres I, Rubio-Ruiz ME, Cano-Martínez A, Manzano-Pech L, Guarner-Lans V. Frailty and the Interactions between Skeletal Muscle, Bone, and Adipose Tissue-Impact on Cardiovascular Disease and Possible Therapeutic Measures. Int J Mol Sci. 2023;24(5):4534. doi:https://doi.org/10.3390/ijms24054534.
Vega-Cabello V, Caballero FF, Lana A, et al. Association of Zinc Intake With Risk of Impaired Physical Function and Frailty Among Older Adults. J Gerontol A Biol Sci Med Sci. 2022;77(10):2015–2022. doi:https://doi.org/10.1093/gerona/glac014.
Kim D, Won CW, Park Y. Association Between Erythrocyte Levels of n-3 Polyunsaturated Fatty Acids and Risk of Frailty in Community-Dwelling Older Adults: The Korean Frailty and Aging Cohort Study. J Gerontol A Biol Sci Med Sci. 2021;76(3):499–504. doi:https://doi.org/10.1093/gerona/glaa042
Siefkas AC, Millar CL, Dufour AB, Kiel DP, Jacques PF, Hannan MT, Sahni S. Dairy Food Intake Is Not Associated With Frailty in Adults From the Framingham Heart Study. J Acad Nutr Diet. 123(5):729–739.e1. doi: https://doi.org/10.1016/j.jand.2022.09.012.
Rahi B, Pellay H, Chuy V, Helmer C, Samieri C, Féart C. Dairy Product Intake and Long-Term Risk for Frailty among French Elderly Community Dwellers. Nutrients. 13(7):2151. doi: https://doi.org/10.3390/nu13072151.
Lana A, Rodriguez-Artalejo F, Lopez-Garcia E. Dairy Consumption and Risk of Frailty in Older Adults: A Prospective Cohort Study. J Am Geriatr Soc. 2015;63(9):1852–1860. doi:https://doi.org/10.1111/jgs.13626.
Laclaustra M, Rodriguez-Artalejo F, Guallar-Castillon P, Banegas JR, Graciani A, Garcia-Esquinas E, Ordovas J, Lopez-Garcia E. Prospective association between added sugars and frailty in older adults. Am J Clin Nutr. 107(5):772–779. doi: https://doi.org/10.1093/ajcn/nqy028.
Yang Y, Zhang D, Yuan G, Wu Y, Huang X. Association between nut consumption and frailty in the elderly: a large sample cross-sectional study. J Hum Nutr Diet. doi: https://doi.org/10.1111/jhn.13208.
Wang R, Hannan MT, Wang M, Schwartz AW, Lopez-Garcia E, Grodstein F. Long-Term Consumption of Nuts (Including Peanuts, Peanut Butter, Walnuts, and Other Nuts) in Relation to Risk of Frailty in Older Women: Evidence from a Cohort Study. J Nutr. 153(3):820–827. doi: https://doi.org/10.1016/j.tjnut.2023.01.003.
Ouyang Y, Wang H, Wang Z, Su C, Zhang J, Du W, Jiang H, Huang F, Jia X, Wang Y, Li L, Zhang B. [Intake of nuts among Chinese elderly residents in 15 provinces, 2015]. Wei Sheng Yan Jiu. 48(4):526–530. Chinese.
Johnson KO, Shannon OM, Matu J, Holliday A, Ispoglou T, Deighton K. Differences in circulating appetite-related hormone concentrations between younger and older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32(7):1233–1244. doi:https://doi.org/10.1007/s40520-019-01292-6.
Ispoglou T, Witard OC, Duckworth LC, Lees MJ. The efficacy of essential amino acid supplementation for augmenting dietary protein intake in older adults: implications for skeletal muscle mass, strength and function. Proc Nutr Soc. 2021;80(2):230–242. doi:https://doi.org/10.1017/S0029665120008010.
Zhao W, Hasegawa K, Chen J. The use of food-frequency questionnaires for various purposes in China. Public Health Nutr. 2002;5(6A):829–833. doi:https://doi.org/10.1079/phn2002374.
Acknowledgments
The authors gratefully acknowledge Dr. Hao Lei for providing valuable suggestions on statistical analysis for this paper.
Funding
Funding Statement: This research was funded by the Key Research and Development Program of Zhejiang Province (grant number 2020C03002), Healthy Zhejiang One Million Cohort (grant number K20230085), and the Leading Innovative and Entrepreneur Team Introduction Program of Zhejiang (grant number 2019R01007).
Author information
Authors and Affiliations
Contributions
Author Contributions: Min Yang and Qiyun Xue contributed to the conception and design of the study. Qiyun Xue and Qiqi Lin contributed to the acquisition of data and data analysis. Qiyun Xue and Menglian Shen wrote the original draft. Xifeng Wu and Min Yang contributed to revising the manuscript. All authors reviewed and edited the draft, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical standards: The study was approved by the Research Ethics Committee of Peking University (IRB00001052-13074). All participants provided informed consent prior to their participation in the study.
Conflicts of Interest: The authors declare no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Xue, Q., Shen, M., Lin, Q. et al. The Association between Dietary Protein Diversity and Protein Patterns with Frailty in Older Chinese Adults: A Population-Based Cohort Study. J Nutr Health Aging 27, 1219–1227 (2023). https://doi.org/10.1007/s12603-023-2043-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-2043-5