Abstract
In this cross-sectional analysis of 10,071 community dwelling adults aged ≥70 years, we examined factors associated with meal skipping (self-reported) using multivariable logistic regression. Prevalence of meal skipping in this study was 19.5%. The adjusted odds (aOR [95%CI]) of meal skipping were lower in those 85+ years (vs. 70–74.9 years, 0.56 [0.45–0.70]), and in those in regional areas (vs. urban area, 0.81 [0.72–0.92]). Higher odds of meal skipping were observed for those living alone (vs. living with someone, 1.84 [1.64–2.05]), current smokers (vs. non-smokers, 2.07 [1.54–2.80]), consumers of high amounts of alcohol (vs. abstainers 1.93 [1.35–2.75]), those with poor oral health (vs. excellent oral health, 1.71 [1.07–2.73]) diabetes (vs. not 1.26 [1.06–1.50]), or frailty (vs. not, 1.63 [1.09–2.43]). This study identified socio-demographic, social, behavioural and biomedical correlates of meal skipping in later life, which may assist in targeting interventions to address meal skipping.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nutrition-related diseases are major contributors to disability and lowered quality of life in older age (1), and nutrition survey data consistently suggest that people over the age of 65 years do not meet their daily recommended nutritional or energy requirements (2). Nutrient and energy deficiency in later life can increase the risk and the severity of age related chronic disease (3).
It is accepted that there is a relationship between the number of meals consumed per day and overall dietary quality in those over the age of 65 years (4, 5). It is also common for dietary intake to change in quantity and quality in later life, with dietary behaviours such as meal skipping cited as influential in the development of late-life malnutrition (4).
Meal skipping is defined as the omission of one of the traditional daily meals, breakfast, lunch, or dinner (6, 7). A recent systematic review (8) on the prevalence and correlates of meal skipping in community dwelling older adults, reported variability in the proportion of adults who consumed less than 3 meals daily, ranging from 2.1 to 61%. Advancing age, male gender, and social exclusion were reported as significant correlates of meal skipping though the evidence base is limited by non-contemporary and heterogeneous studies (8) Sustaining nutritional status in community dwelling older adults is important to lower the risk of age-related disease, hospitalisation and institutionalisation (9) and to maintain independent living (4). The current evidence base on food behaviours in older adults is predominantly centred on institutionalised people, with limited research on those living independently in the community (9).
Therefore, the aim of this study is to determine the prevalence and socioecological factors associated with meal skipping in a large cohort of community dwelling adults aged 70 years and over.
Methods
Study population
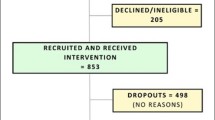
The ASPirin in Reducing Events in the Elderly (ASPREE) study was a multi-centre randomised placebo-controlled trial of low dose aspirin conducted in Australia and the United States (U.S.) between 2010 and 2017. The Australian ASPREE cohort included 16,703 healthy, community dwelling, participants aged 70 years or above who were, at baseline, free from persistent physical disability, dementia, cardiovascular disease or chronic/serious disease that was likely to be fatal within 5 years (10). Details of the inclusion and exclusion criteria and methods have been previously described (10, 11). The ASPREE Longitudinal Study of Older Persons (ALSOP) is a longitudinal cohort study, comprised of 14,892 Australian participants from ASPREE (10). For this study, participants with missing data on exposure (meal skipping) (n=2,466) and independent variables of interest (n=2,355) were removed from the primary analysis dataset. (See Supplementary Figure 1).
Meal skipping
Self-reported dietary intake, including the frequency of meal skipping each week, was ascertained via the year-3 ALSOP medical questionnaire (10). Participants were asked “How often do you miss meals?”, and they were able to choose from the following responses: “never/rarely, once a week or less, several times a week, everyday”. In line with the available evidence (6), and due to small distribution of meal skipping across all categories of the meal skipping variable, we created a variable that assessed whether meal skipping was present or not (yes/no). We classified responses “once a week or less”, “several times a week” or “every day” as “yes”, and “never/rarely” as “no”.
Correlates
The selection of potential correlates was informed by previous research into dietary patterning in older adults (1). These factor correlates were grouped in the following categories: 1) economic and demographic, 2) health behaviours 3) biomedical, 4) social, 5) psychological. The majority of measures were assessed at 3-year ASPREE/ALSOP follow-up interviews, with the exception of years of education, area-level socioeconomic status using the Index of Relative Social Advantage and Disadvantage (IRSAD) (12) and presence of hypertension, polypharmacy, frailty and diabetes which were taken at baseline in the ASPREE trial. The Centre for Epidemiological Studies Depression (CES-D) scale (13) was used to assess level of depressive symptoms and baseline quality of life was assessed using the SF-12 questionnaire, condensed to physical (PCS) and mental component scores (MCS) with higher PCS and MCS scores indicating higher physical and mental quality of life. The mean PCS and MCS were calculated for the study population, and participants were categorised into above or below the average score (14). Behavioural factors were assessed via self-reported questionnaires. In the year-3 ASPREE follow up interviews, participants reported their smoking status, daily consumption and daily alcohol intake. The year-3 ALSOP medical questionnaire asked participants to rate their difficulty performing tasks such as reading labels. Biomedical factors were assessed via combination of clinical and self-reported information at baseline (polypharmacy, hypertension, diabetes and frailty) and at year-3 by the ALSOP medical questionnaire (BMI, oral health status, saliva levels and pain frequency). Living status was assessed by the year-3 ALSOP social questionnaire, participants were asked to report who they lived with. (For additional detail on how correlates were measured please see Supplementary Table 1).
Statistical analysis
Participant characteristics were presented as counts and percentages based on the meal skipping status. Differences in study characteristics between participants who rarely or never skip meals compared to those who skip meals were assessed using Chi-squared tests and two-way T-tests. The association between socio-ecological factors and meal skipping was assessed using multivariable logistic regression where all potential correlates were mutually adjusted. Odds ratios and 95% confidence intervals (CI) were reported. BMI is a recognised correlate of meal skipping in older adults (4, 15, 16) however, substantial missing data were observed for BMI (n=1,194); hence, the variable was removed from the primary analysis. Instead, a multivariable binary logistic regression sensitivity analysis model that included BMI was undertaken (n=8,877). Similarly, depression correlates with appetite loss 17 in older age, however, a considerable amount of data was also missing for the depression variable (n=1,021), and a further sensitivity analysis included all variables in the primary model and the CESD-10 scores (n=9050).
We performed correlation analyses between the hypothesized correlates of meal skipping. The highest correlation coefficient reported was between PCS and pain frequency variables (r=0.33) suggesting no multi-collinearity in the data. All statistical analysis was performed in Stata statistical software version 17.0 (StataCorp LLC, College Station, Texas; www.stata.com) (18).
Results
Participant characteristics
There were 10,071 participants (54% were female) included in this study with mean age of 77.9 years at the time of meal skipping assessment. A majority of participants lived in major metropolitan areas, lived with others, had ≤12 years of education, lived in high socioeconomic areas (29.9%) and were non-smokers (97.9%) (Table 1). Participant characteristics were compared between participants with missing data (n=2,466) and those without (n=10,071) with no substantial differences observed.
Prevalence of meal skipping
Four in five (80.5%) participants reported never or rarely skipping meals, 14.9% reported skipping meals once a week, 3.8% reporting skipping meals several times per week and less than 1% reporting skipping meals daily. The total prevalence of meal skipping in this study population of adults aged 70 years and over was 19.5%.
Compared to people who never or rarely skipped meals, those who reported any meal skipping were younger on average, had more than 12 years of education, reside in inner city locations, and have poorer oral health. People who skipped meals were also more likely to live alone, to consume over 3 alcoholic drinks daily, be current smokers and be diagnosed with diabetes and be classified as frail. (Table 1)
Correlates of Meal Skipping
The odds of meal skipping were lower among adults aged 85 years and over (vs. 70–74.9 years OR [95%CI], 0.56 [0.45–0.70]), in women (vs. men 0.84 [0.75–0.94]), in those living in regional and remote areas (vs. those living in major cities, 0.81 [0.72–0.92]) and in those with above average MCS (vs. those with below average MCS 0.76 [0.69–85]). In contrast, odds of any meal skipping were greater among older adults living alone (vs. with others 1.84 [1.64–2.05]), those who smoked (vs. non-smokers 2.07 [1.54–2.80]), those who consumed more than 4 alcoholic drinks a day (vs. those who abstained 1.93 [1.35–2.75]), and individuals reporting more than 12 years of formal education (vs. those reporting 12 years or less of formal education 1.15 [1.04–1.28]). People diagnosed with diabetes had higher odds of meal skipping (vs. those without diabetes 1.26 [1.06–1.50]). Higher odds of meal skipping were also observed among older adults with frailty (vs. those without 1.63 [1.09–2.43]). (Figure 1 and Supplementary Table 2)
With regard to oral health, older adults who reported good/fair oral health or poor oral health had higher odds of meal skipping (vs. those who reported excellent oral health 1.21 [1.10–1.35]; 1.71 [1.07–2.73], respectively). Odds of meal skipping were also higher among people who reported having difficulty reading food labels (vs. those who did not report difficulty 1.44 [1.12–1.86]). (Figure 1 and Supplementary Table 2)
Forrest Plot: The association of demographic, social, behavioural, biomedical, and psychological factors with meal skipping in adults aged 70 years and over: the results of the multivariable binary logistic regression analyses
OR= odds ratio, CI=confidence interval, IRSAD=Index of Relative Socioeconomic Advantage and Disadvantage 12 *= self-reported; PCS= Physical Component Scores of the SF-12 questionnaire; MCS= Mental Component Score of the SF-12 questionnaire; Hypertension = systolic blood pressure ≥140mmHg and diastolic blood pressure ≥90mmHg or taking blood pressure-lowering medication (11, 29); Diabetes mellitus = self-reported, taking medication for diabetes, or a fasting glucose ≥126mg/dL (11, 29); Frailty ¬is based on modified Fried frailty criteria of low body weight, low grip strength, exhaustion, low physical activity and slow walking speed. 29, 30 Those classified as pre-frail met one or two of the Fried criteria, and those classified as frail met 3 or more criteria. (29, 30); Polypharmacy = self-reported, or confirmed in medical record, of 5 or more prescription medications
Sensitivity analyses
Results were similar after the additional inclusion of BMI in the regression model. No association was observed between meal skipping and BMI. (Supplementary Table 3)
After inclusion of depressive symptoms (CESD-10 overall score) to the primary model, the results indicated that the odds of meal skipping were 26% (1.26 [1.11–1.43]) greater for those who experienced mild depressive symptoms, and 60% (1.6 [1.36–1.90]) greater for those who reported moderate to severe depressive symptoms compared to those who did not report depressive symptoms (Supplementary Table 3). When compared to the primary analysis, the association between female sex and meal skipping did not maintain its significance with meal skipping in this model (0.99 [0.88–1.11], 0.898). The association between smoking and meal skipping was strengthened by the addition of depression to the multivariate model, with greater odds of meal skipping reported for current smokers (compared to non-smokers 2.28 [1.70–3.65]) when compared with the primary model (2.07 (1.54–2.80), <0.001). (Supplementary Table 3)
Discussion
We report a wide-ranging examination on the prevalence and the sociodemographic, behavioural, biomedical, psychological and social factors associated with meal skipping in more than 10,000 community-dwelling individuals aged 70 years and over. Among the strongest correlates, we observed that the oldest age group (85+), women and those with above average mental health component scores, were less likely to skip meals; while those who smoked, consumed more than 4 alcoholic drinks daily, lived alone and reported poor oral health were more likely to skip meals. These results are important, as they point to correlates associated with meal skipping, that if addressed may help reduce nutritional deficiency in later life.
The majority of participants in this cohort rarely or never skipped meals. The observed meal skipping prevalence of 19.5% is consistent with similar research in Korean older adults, which noted that 20.9% of participants indicated some level of meal skipping (5). It is also similar to recent statistics on breakfast skipping in adults, whereby King et al (19) reported that 17.1% of adults skipped breakfast. However, it differs from the prevalence observed in children (10%) (7), adolescents (29.9%) (20) and younger adults (10%) (21) highlighting the need for age specific research on important dietary behaviours, such as meal skipping.
We observed that adults aged 85 years and over were less likely to skip meals compared to those aged 70 to 74.9 years. While demonstrating a similar pattern of consumption across age groups to that reported in the current literature on meal skipping in older adults (5), our findings were more pronounced.
Our results indicate that women were less likely to skip meals compared to men, a result that is consistent with the current evidence (4, 16). Previous research (1) notes that nutritional vulnerabilities are increased for men, especially after the death of a spouse, due to a lack of nutritional knowledge and food preparation skills. Interestingly, the results of our sensitivity analysis demonstrated that further adjustment for depressive symptoms weakened the association between sex and meal skipping. This may be due to the increased likelihood of Australian women to report depressive symptoms compared to men (22); a disparity that is also likely to be exacerbated by generational factors associated with the age of this cohort (22). Previous research on the ASPREE cohort (23) has demonstrated a higher prevalence of women reporting depressive symptoms (CESD-10 overall score 8 or above) compared to men, consistent with findings international cohorts of older adults (24).
In ASPREE participants, the odds of meal skipping were greater among those who smoked and those who consumed higher levels of alcohol compared to those who did not. Smoking is frequently associated with meal skipping in older adults, 5, 15, 16 as well as in younger adults (6, 21). Conversely, findings on the association between alcohol consumption and meal skipping are mixed, with studies in older adults demonstrating both positive (16), negative (5) or no (15) association between alcohol consumption and meal skipping.
This study observed that those who reported living alone had higher odds of meal skipping than people who reported living with others. These results are consistent with the current body of evidence which highlights living alone as a common factor associated with meal skipping among older adults (4, 5, 15).
This study also highlighted the influence of oral health on meal skipping. Changes in dietary intake in later life as a result of poor oral health have been reported in the literature with Gu et al. (25) noting a shift toward a more refined western diet in those over 80 years with difficulty chewing. When considering oral health within the Australian context, it is important to acknowledge that dental care was not, at the time of this study, provided to adults as part of the publicly funded universal healthcare system. This is likely to have increased the influence of the socioeconomic gradient on oral health outcomes (26). The ALSOP cohort is skewed toward a higher socio-economic status (based on area levels of advantage and disadvantage) and education level (higher level of tertiary education 23% vs 2.4%) compared to the general Australian population over the age of 70 years (10). As a result, these participants are likely to have increased access to the financial resources required for suitable dental care compared to their counterparts in the general Australian population. As such, the influence of oral health on meal skipping may be more pronounced within the general community than within this cohort. Food insecurity affects 1 in 50 adults older than 65 years in Australia and can impact food intake (27). Socioeconomic factors have a been shown to have a significant impact on food security status for older Australians (27). Due to the noted differences in socioeconomic status between the ALSOP cohort and the general community, the influence of food insecurity on meal skipping is likely underrepresented in this study.
The results of our sensitivity analysis highlighted a positive association between severity of depressive symptoms and odds of meal skipping. This is consistent with evidence on meal skipping in older adults (5). Depression is often characterised by lowered appetite (24), interestingly, the results of this sensitivity analysis demonstrated that depression strengthened the association between smoking and meal skipping, a behaviour that can also influence appetite and food intake (28). Further research may be required to understand the association between variations in symptoms of depression and meal skipping.
Acknowledging the interrelationship of many of the psychological, social, economic, behavioural and biomedical correlates highlighted in our results is important. It will be essential for future research on meal skipping to further examine the ways in which these factors accumulate across the lifespan, and how their interaction in older age influences health behaviours, and alters the nature and severity of disease risk. The diverse implications of social and psychological factors in older age emphasise the importance of tailored psycho-social services that meet the specific needs of community dwelling older adults. It is likely that many of the protective factors for health and wellbeing in later life are established in younger years, further highlighting the importance of a lifespan focus in health research to identify and manage the socio-ecological factors associated with disease development in later life (8).
The strengths of this research include use of a large, well-characterised sample of older adults, high response rates to questionnaires and strong inclusion and exclusion criteria. 10 There are also several limitations. This is a cross sectional study, so we cannot make any conclusions about the direction of the relationship between the socio-ecological correlates and meal skipping. The use of secondary data also limits the type of information available within the analysis, as such the influence of broader socio-political and environmental correlates on meal skipping could not be assessed. This issue was also noted by Pendergast et al. (21) in their study on the socio-ecological correlates of meal skipping in younger adults, and potentially highlights the need for nutritional research to more consistently consider and explore the influence of the socio-political and environmental context on dietary behaviour. The Year 3 ALSOP medical questionnaire did not define meal in its question on meal skipping, as such no detail on which meal was skipped is provided, and differing cultural and social definitions of meal may increase the risk of misunderstanding and misclassification. We condensed the meal skipping variable from four categories (never/rarely, once a week or less, several times a week, everyday) to two (yes/no) and while this mirrored other research on this topic (6), it may have reduced our ability to discuss differing severities of meal skipping. Future research may benefit from more robust data, allowing for a more granular understanding of the differing frequencies of meal skipping, and the specific meals skipped in older adults. The ASPREE/ALSOP cohort may possibly be a healthier and wealthier subset of the community, as a result of the ASPREE inclusion criteria and their interest in participating in a long-term study of healthy ageing (10, 11). However, it should be noted that by the time the self-reported meal skipping measure was assessed (3 years after enrolment into the study), a number of participants had developed chronic disease (29). This ‘healthy cohort’ effect, compared to the general population, is a factor to consider in the interpretation of the study results, and we advise caution when generalising these findings to population with a lower area level socioeconomic status. A larger body of longitudinal research on meal skipping across the lifespan may be necessary to better determine the influence of age on eating behaviour including meal frequency. Finally, for some variables year 3 data were not available, so baseline derived variables were utilised. This potentially increases the risk of misclassification of participants who may have potentially being diagnosed with hypertension, diabetes, and frailty post baseline.
Conclusion
In this study on more than 10,000 adults aged 70 years and over, we observed that the prevalence of meal skipping was 19.5%. Numerous factors associated with meal skipping were identified, including living circumstance, sex, alcohol intake and smoking status. To better understand the influence of these factors on dietary behaviours such as meal skipping, it will be important for future research to focus on their influence and interaction across the lifespan, and the multiplicity of risk associated with their interaction, and to what extent these factors operate independently or converge on a common mediator such as depression. The results of these analyses, and the identification of key correlates of meal skipping in older adults will be important to inform further investigation on the impact of meal skipping on health outcomes in this cohort.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due data being part of a large ongoing observational cohort study with a rigorous process to access data. The datasets generated and/or analysed during the current study are available in the ASPREE clinical trial data resource repository, https://aspree.org/aus/researchers/. The ASPREE clinical trial data resource is managed in partnership with the US, in the Australian ASPREE National Coordinating Centre. New ASPREE projects with appropriate scientific merit may be proposed by external researchers, and submitted to ASPREE for consideration. Project proposals requesting access to any aspect of data, samples, or analyses from the ASPREE clinical trial and/or sub-studies must gain the support of the ASPREE Principal Investigators. Applications are submitted via a secure web site, the ASPREE Access Management System (AMS). Applicants can obtain information by contacting aspree.ams@monash.edu.
References
Host A, McMahon AT, Walton K, Charlton K. Factors Influencing Food Choice for Independently Living Older People-A Systematic Literature Review. J Nutr Gerontol Geriatr. Apr-Jun 2016;35(2):67–94. doi:https://doi.org/10.1080/21551197.2016.1168760
Whitelock E, Ensaff H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients. 2018;10(4):413. doi:https://doi.org/10.3390/nu10040413
Chang SF. Frailty Is a Major Related Factor for at Risk of Malnutrition in Community-Dwelling Older Adults. J Nurs Scholarsh. Jan 2017;49(1):63–72. doi:https://doi.org/10.1111/jnu.12258
Tani Y, Kondo N, Takagi D, et al. Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: Results of the JAGES. Appetite. December 01 2015;95:1–8.
Kwak Y, Kim Y. Association between mental health and meal patterns among elderly Koreans. Geriatrics and Gerontology International. January 2018;18(1):161–168.
Pendergast FJ, Livingstone KM, Worsley A, McNaughton SA. Correlates of meal skipping in young adults: a systematic review. Int J Behav Nutr Phys Act. Dec 1 2016;13(1):125. doi:https://doi.org/10.1186/s12966-016-0451-1
Dubois L, Girard M, Potvin Kent M, Farmer A, Tatone-Tokuda F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among pre-school children. Public Health Nutr. Jan 2009;12(1):19–28. doi:https://doi.org/10.1017/s1368980008001894
Wild H, Baek, Y, Shah, S, Gasevic, A and Owen, A. The Socioecological Correlates of Meal Skipping in Community Dwelling Older Adults: A Systematic Review Nutrition Reviews. 2022
Low E, Kellett J, Bacon R, Naumovski N. Food Habits of Older Australians Living Alone in the Australian Capital Territory. Geriatrics (Basel). Sep 18 2020;5(3) doi:https://doi.org/10.3390/geriatrics5030055
McNeil JJ, Woods RL, Ward SA, et al. Cohort Profile: The ASPREE Longitudinal Study of Older Persons (ALSOP). Int J Epidemiol. 2019;48(4):1048–1049h. doi:https://doi.org/10.1093/ije/dyy279
McNeil JJ, Woods RL, Nelson MR, et al. Baseline Characteristics of Participants in the ASPREE (ASPirin in Reducing Events in the Elderly) Study. The journals of gerontology Series A, Biological sciences and medical sciences. 2017;72(11):1586–1593. doi:https://doi.org/10.1093/gerona/glw342
Australian Bureau of Statistics. 2033.0.55.001 — Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011 https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2033.0.55.001main+features100042011. 2011
Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977/06/01 1977;1(3):385–401. doi:https://doi.org/10.1177/014662167700100306
Jamali A, Tofangchiha S, Jamali R, et al. Medical students’ health-related quality of life: roles of social and behavioural factors. Medical Education. 2013;47(10):1001–1012. doi:https://doi.org/10.1111/medu.12247
Lee CJ, Templeton S, Wang C. Meal skipping patterns and nutrient intakes of rural southern elderly. Journal of Nutrition for the Elderly. Vol.15(2), 1995, pp. 1–14.; 1995.
Wister A, Cosco T, Mitchell B, Fyffe I. Health behaviors and multimorbidity resilience among older adults using the Canadian Longitudinal Study on Aging. International Psychogeriatrics. 01 Jan 2020;32(1):119–133.
Potter GG, McQuoid DR, Steffens DC. Appetite loss and neurocognitive deficits in late-life depression. International journal of geriatric psychiatry. 2015;30(6):647–654.
StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. 2021
King DE, Xiang J. A Relationship Between Mortality and Eating Breakfast and Fiber. The Journal of the American Board of Family Medicine. 2021;34(4):678–687. doi:https://doi.org/10.3122/jabfm.2021.04.210044
Lee JY, Ban D, Kim H, et al. Sociodemographic and clinical factors associated with breakfast skipping among high school students. Nutr Diet. Sep 2021;78(4):442–448. doi:https://doi.org/10.1111/1747-0080.12642
Pendergast FJ, Livingstone KM, Worsley A, McNaughton SA. Examining the correlates of meal skipping in Australian young adults. Nutrition Journal. 2019/04/03 2019;18(1):24. doi:https://doi.org/10.1186/s12937-019-0451-5
Health AIo, Welfare. Mental health. 2020. https://www.aihw.gov.au/reports/australias-health/mental-health
Agustini B, Lotfaliany M, Woods RL, et al. Patterns of Association between Depressive Symptoms and Chronic Medical Morbidities in Older Adults. Journal of the American Geriatrics Society. 2020;68(8):1834–1841. doi:https://doi.org/10.1111/jgs.16468
Ruskin PE, Blumstein Z, Walter-Ginzburg A, et al. Depressive Symptoms Among Community-Dwelling Oldest-Old Residents in Israel. Am J Geriatr Psychiatry. Summer 1996;4(3):208–217. doi:https://doi.org/10.1097/00019442-199622430-00004
Gu Q, Sable CM, Brooks-Wilson A, Murphy RA. Dietary patterns in the healthy oldest old in the healthy aging study and the Canadian longitudinal study of aging: a cohort study. BMC Geriatrics. 2020/03/16 2020;20(1):106. doi:https://doi.org/10.1186/s12877-020-01507-w
Mejia GC, Elani HW, Harper S, et al. Socioeconomic status, oral health and dental disease in Australia, Canada, New Zealand and the United States. BMC Oral Health. 2018/10/26 2018;18(1):176. doi:https://doi.org/10.1186/s12903-018-0630-3
Quine SaM, S. Food insecurity in community-dwelling older Australians. Public Health Nutrition 2006;9(2):219–224. doi:doi:https://doi.org/10.1079/PHN2005834
Zachari K, Anastasiou CA, Sidiropoulou M, Katsaounou P, Tenta R, Yannakoulia M. Acute effect of smoking and its abstinence on dietary intake and appetite. European Respiratory Journal. 2016;48(suppl 60):OA3499. doi:https://doi.org/10.1183/13993003.congress-2016.OA3499
McNeil JJ, Woods RL, Nelson MR, et al. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. New England Journal of Medicine. 2018;379(16):1499–1508. doi:https://doi.org/10.1056/NEJMoa1800722
Wolfe R, Murray AM, Woods RL, et al. The aspirin in reducing events in the elderly trial: Statistical analysis plan. Int J Stroke. 2018;13(3):335–338. doi:https://doi.org/10.1177/1747493017741383
Acknowledgements
Study concept and design: HW, DG, AO. Data Analysis: HW. Drafting of the manuscript: HW. Critical revision of the manuscript for important intellectual content: All authors.
Funding
The ASPREE study was supported by a grant (UA01AG029824 and U19AG062682) from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health, and by grants (334047 and 1127060) from the Australian National Health and Medical Research Council, by Monash University and the Victorian Cancer Agency. The ALSOP sub-study was supported by Monash University and an unencumbered grant from the Wicking Trust. JR is supported by NHMRC Dementia Research Leader Fellowship (1135727). MB is supported by NHMRC Senior Principal Research Fellowships 1059660 and 1156072. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This secondary analysis of ASPREE and ALSOP data was approved by the Monash University Human Research Ethics Committee (Project ID 25829). The ASPREE trial was approved by multiple Human Research Ethics Committees/Institutional Review Boards.10, 11, 29 The ALSOP study was reviewed and approved by the Monash University Human Research Ethics Committee (project numbers CF11/1100 and CF11/1935). All participants provided signed informed consent.
Additional information
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The ASPREE study was supported by a grant (UA01AG029824 and U19AG062682) from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health, and by grants (334047 and 1127060) from the Australian National Health and Medical Research Council, by Monash University and the Victorian Cancer Agency. The ALSOP sub-study was supported by Monash University and an unencumbered grant from the Wicking Trust. JR is supported by NHMRC Dementia Research Leader Fellowship (1135727). MB is supported by NHMRC Senior Principal Research Fellowships 1059660and 1156072.
Electronic Supplementary Material
Rights and permissions
Open Access : This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Wild, H., Gasevic, D., Woods, R.L. et al. Correlates of Meal Skipping in Community Dwelling Older Adults: A Cross-Sectional Study. J Nutr Health Aging 27, 159–165 (2023). https://doi.org/10.1007/s12603-023-1884-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1884-2