Abstract
Objectives
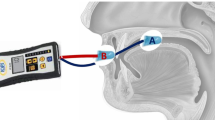
We aimed to investigate the relationship between the ability to press Process Lead (PL) in the oral cavity and the tongue pressure and recommended diet form for elderly individuals in nursing homes, using PL normalized physical properties.
Design
Cross-sectional observation study.
Setting
Geriatric facilities.
Participants
A 100 elderly individuals aged between 67–96 years.
Measurements
PL was pressed between the tongue and palate to evaluate its deformation. The thickness was set at 6, 9, and 18 mm. The tongue pressure was measured with a JMS tongue pressure manometer. The number of chewing cycles until an 18-mm thick PL was first swallowed was measured (PL chewing test). The diet was set to level 4, and the recommended form was evaluated by video endoscopic evaluation of swallowing (VE). The results of the PL pressing test and correlations between PL chewing test, tongue pressure, and diet level were statistically examined.
Results
The tongue pressure was significantly decreased in groups that could not press the PL. The PL pressing test and recommended diet form showed a significant correlation, and the elderly with difficulty in pressing the PL had a lower diet level. In addition, the diet level decreased with decreased PL chewing test performance in those without molar occlusion.
Conclusions
The PL pressing and chewing tests may aid in ascertaining the appropriate diet level. In the future, we would like to verify the usefulness of these tests in determining the diet level of elderly people requiring long-term care at the time of entering the facility.





Similar content being viewed by others
References
Manabe T, Teramoto S, Tamiya N, Okochi J, Hizawa N. Risk factors for aspiration pneumonia in older adults. PloS One 2015;10:e0140060.
Rofes L, Arreola V, Almirall J, Cabre M, Campins L, Garcia-Peris P, Speyer R, Clavé P. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract 2011:818979.
Penman JP, Thomson M. A review of the textured diets developed for the management of dysphagia. J Hum Nutr Diet 1998;11:51–60.
Cichero JA, Steele C, Duivestein J, Clave P, Chen J, Kayashita J, Dantas R, Lecko C, Speyer R, Lam P, Murray J. The need for international terminology and definitions for texture-modified foods and thickened liquids used in dysphagia management: foundations of a global initiative. Curr Phys Med Rehabil Rep 2013;1:280–291.
Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 1991;100:678–681.
Clave P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr 2008;27:806–815.
Nokubi T, Yoshimuta Y, Nokubi F, Yasui S, Kusunoki C, Ono T, Maeda Y, Yokota K. Validity and reliability of a visual scoring method for masticatory ability using test gummy jelly. Gerodontology 2013;30:76–82.
Hayakawa I, Watanabe I, Hirano S, Nagao M, Seki T. A simple method for evaluating masticatory performance using a color-changeable chewing gum. Int J Prosthodont 1998;11:173–176.
Mioche L, Hiiemae KM, Palmer JB. A postero-anterior videofluorographic study of the intra-oral management of food in man. Arch Oral Biol 2002;47:267–280.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am 2008;19:691–707, vii.
Yoshida M, Kikutani T, Tsuga K, Utanohara Y, Hayashi R, Akagawa Y. Decreased tongue pressure reflects symptom of dysphagia. Dysphagia 2006;21:61–65.
Ono T, Kumakura I, Arimoto M, Hori K, Dong J, Iwata H, Nokubi T, Tsuga K, Akagawa Y. Influence of bite force and tongue pressure on oro-pharyngeal residue in the elderly. Gerodontology 2007;24:143–150.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia 2015;30:80–87.
Machida N, Tohara H, Hara K, Kumakura A, Wakasugi Y, Nakane A, Minakuchi S. Effects of aging and sarcopenia on tongue pressure and jaw-opening force. Geriatr Gerontol Int 2017;17:295–301.
Mano T, Katsuno M, Banno H, Suzuki K, Suga N, Hashizume A, Araki A, Watanabe H, Tanaka S, Yamamoto M, Sobue G. Tongue pressure as a novel biomarker of spinal and bulbar muscular atrophy. Neurology 2014;82:255–262.
Nakamori M, Hosomi N, Ishikawa K, Imamura E, Shishido T, Ohshita T, Yoshikawa M, Tsuga K, Wakabayashi S, Maruyama H, Matsumoto1 M. Prediction of pneumonia in acute stroke patients using tongue pressure measurements. PLoS One 2016;11:e0165837.
Tanaka Y, Nakano Y, Yokoo M, Takeda Y, Yamada K, Kayashita J. Examination about the relation of meal form, tongue pressure, grip and walking state in inpatient and elderly residents. The Japanese Journal of Dysphagia Rehabilitation 2015;19:52–62.
Nakagawa K, Matsuo K, Shibata S, Inamoto Y, Ito Y, Abe K, Ishibashi N, Fujii W, Saitoh E. Efficacy of a novel training food based on the process model of feeding for mastication and swallowing - A preliminary study in elderly individuals living at a residential facility-. Japanese Journal of Comprehensive Rehabilitation Science 2014;5:72–78.
Shibata S, Kagaya H, Tanaka S, Fujii W, Nakagawa K, Matsuo K, Abe K, Ishibashi N, Inamoto Y, Saitoh E. Efficacy of a novel training food based on the process model of feeding for mastication and swallowing: A study among dysphagia patients. Japanese Journal of Comprehensive Rehabilitation Science 2017;8:82–87.
Sasao Y, Nohara K, Kotani Y, Sakai T. Videoendoscopic evaluation of the bolus preparation function for dentulous healthy subjects. J J Gerodont. 2008;23:42–49.
Neubauer PD, Rademaker AW, Leder SB. The Yale Pharyngeal Residue Severity Rating Scale: an anatomically defined and image-based tool. Dysphagia 2015;30:521–528.
Martin RE, Murray GM, Kemppainen P, Masuda Y, Sessle BJ. Functional properties of neurons in the primate tongue primary motor cortex during swallowing. J Neurophysiol 1997;78:1516–1530.
Naganuma K, Inoue M, Yamamura K, Hanada K, Yamada Y. Tongue and jaw muscle activities during chewing and swallowing in freely behaving rabbits. Brain Res 2001;915:185–194.
Ono T, Hori K, Nokubi T. Pattern of tongue pressure on hard palate during swallowing. Dysphagia 2004;19:259–264.
Palmer JB, Rudin NJ, Lara G, Crompton AW. Coordination of mastication and swallowing. Dysphagia 1992;7:187–200.
Son YR, Choi KH, Kim TG. Dysphagia in tongue cancer patients. Ann Rehabil Med 2015;39:210–217.
van der Bilt A, Olthoff LW, Bosman F, Oosterhaven SP. The effect of missing postcanine teeth on chewing performance in man. Arch Oral Biol 1993;38:423–429.
Mishellany-Dutour A, Renaud J, Peyron MA, Rimek F, Woda A. Is the goal of mastication reached in young dentates, aged dentates and aged denture wearers? Br J Nutr 2008;99:121–128.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakagawa, K., Matsuo, K. Assessment of Oral Function and Proper Diet Level for Frail Elderly Individuals in Nursing Homes Using Chewing Training Food. J Nutr Health Aging 23, 483–489 (2019). https://doi.org/10.1007/s12603-019-1192-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1192-z