Abstract
Bacterial infections at the surgical sites are one of the most prevalent skin infections that impair the healing mechanism. They account for about 20% of all types of infections and lead to approximately 75% of surgical-site infection-associated mortality. Several antibiotics, such as cephalosporins, fluoroquinolones, quinolones, penicillin, sulfonamides, etc., that are used to treat such wound infections not only counter infections but also disrupt the normal flora. Moreover, antibiotics, when used for a prolonged duration, may impair the formation of new blood vessels, delay collagen production, or inhibit the migration of certain cells involved in wound repair, leading to an impaired healing process. Therefore, there is a dire need for alternate therapeutic approaches against such infections. Antimicrobial peptides have gained considerable attention as a promising strategy to counter these pathogens and prevent the spread of infection. Recently, we have reported a designed peptide, DP1, and its broad-spectrum in vitro antimicrobial activity against Gram-positive and Gram-negative bacteria. In the present study, in vivo acute toxicity of DP1 was evaluated and even at a high dose (20 mg/kg body weight) of DP1, a 100% survival of mice was observed. Subsequently, a Staphylococcus aureus-infected murine wound excision model was established to assess the wound healing efficacy of DP1. The study revealed significant wound healing vis-a-vis attenuated S. aureus bioburden at the wound site and also controlled the oxidative stress depicting anti-oxidant activity as well. Healing of the infected wounds was also verified by histopathological examination. Based on the results of this study, it can be concluded that DP1 improves wound resolution despite infections and promotes the healing mechanism. Hence, DP1 holds compelling potential as a novel antimicrobial drug that requires further explorations in clinical platforms.
Graphical Abstract






Similar content being viewed by others
Data Availability
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
References
Smith R, Russo J, Fiegel J et al (2020) Antibiotic delivery strategies to treat skin infections when innate antimicrobial defense fails. Antibiotics 9:56
Punjataewakupt A, Napavichayanun S, Aramwit P (2019) The downside of antimicrobial agents for wound healing. Eur J Clin Microbiol Infect Dis 38:39–54
Bessa LJ, Fazii P, Di Giulio M et al (2015) Bacterial isolates from infected wounds and their antibiotic susceptibility pattern: some remarks about wound infection. Int Wound J 12:47–52
Joshi S, Sharma P, Siddiqui R et al (2020) A review on peptide functionalized graphene derivatives as nanotools for biosensing. Microchim Acta 187:1–15
Stanbro J, Park JM, Bond M et al (2020) Topical delivery of lactobacillus culture supernatant increases survival and wound resolution in traumatic Acinetobacter baumannii infections. Probiotics and antimicrobial proteins 12:809–818
Haque M, Sartelli M, McKimm J et al (2018) Health care-associated infections - an overview. Infect Drug Resist 11:2321–2333
Turner NA, Sharma-Kuinkel BK, Maskarinec SA et al (2019) Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol 17:203–218
Tong SYC, Davis JS, Eichenberger E et al (2015) Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 28:603–661
Hoffmann JP, Friedman JK, Wang Y et al (2020) In situ treatment with novel microbiocide inhibits methicillin resistant Staphylococcus aureus in a murine wound infection model. Front Microbiol 10
Almeida GCM, dos Santos MM, Lima NGM et al (2014) Prevalence and factors associated with wound colonization by Staphylococcus spp. and Staphylococcus aureus in hospitalized patients in inland northeastern Brazil: a cross-sectional study. BMC Infect Dis 14:328
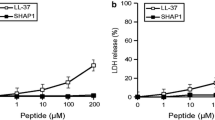
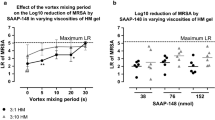
Kim DJ, Lee YW, Park MK et al (2014) Efficacy of the designer antimicrobial peptide SHAP1 in wound healing and wound infection. Amino Acids 46:2333–2343
Prinzi A, Rohde R (2023) The role of bacterial biofilms in antimicrobial resistance. ASM Press
Archer NK, Mazaitis MJ, Costerton JW et al (2011) Staphylococcus aureus biofilms: properties, regulation, and roles in human disease. Virulence 2:445–459
Hughes D, Karlén A (2014) Discovery and preclinical development of new antibiotics. Ups J Med Sci 119:162–169
Sharma S, Barman P, Joshi S et al (2022) Multidrug resistance crisis during COVID-19 pandemic: role of anti-microbial peptides as next-generation therapeutics. Colloids Surf B 211:112303
Joshi S, Sharma S, Verma G et al (2022) Peptide functionalized nanomaterials as microbial sensors. Photophysics and Nanophysics in Therapeutics, Elsevier, 2022, pp 327–48
Barman P, Joshi S, Sharma S et al (2023) Strategic approaches to improvise peptide drugs as next generation therapeutics. Int J Pept Res Ther 29:61
Spencer JJ, Pitts RE, Pearson RA et al (2018) The effects of antimicrobial peptides WAM-1 and LL-37 on multidrug-resistant Acinetobacter baumannii. Pathog Dis 76:fty007
Pfalzgraff A, Brandenburg K, Weindl G (2018) Antimicrobial peptides and their therapeutic potential for bacterial skin infections and wounds. Front Pharmacol 9:281
Joshi S, Siddiqui R, Sharma P et al (2020) Green synthesis of peptide functionalized reduced graphene oxide (rGO) nano bioconjugate with enhanced antibacterial activity. Sci Rep 10:9441
Yang M, Zhang C, Hansen SA et al (2019) Antimicrobial efficacy and toxicity of novel CAMPs against P. aeruginosa infection in a murine skin wound infection model. BMC Microbiol 19:293
Rima M, Rima M, Fajloun Z et al (2021) Antimicrobial peptides: a potent alternative to antibiotics. Antibiotics (Basel) 10
Chen CH, Lu TK (2020) Development and challenges of antimicrobial peptides for therapeutic applications. Antibiotics (Basel) 9
Moretta A, Scieuzo C, Petrone AM et al (2021) Antimicrobial peptides: a new hope in biomedical and pharmaceutical fields. Front Cell Infect Microbiol 453
Sharma P, Sharma S, Joshi S et al (2022) Design, characterization and structure-function analysis of novel antimicrobial peptides based on the N-terminal CATH-2 fragment. Sci Rep 12:12058
Mayank Maan HG, Joshi S, Sharma S, Rishi P, Saini A (2023) Synthetic peptide to combat Staphylococcus aureus-mediated infection: an in vitro and in vivo antimicrobial evaluation study
Diamond G, Beckloff N, Weinberg A et al (2009) The roles of antimicrobial peptides in innate host defense. Curr Pharm Des 15:2377–2392
Martell EM, González-Garcia M, Ständker L et al (2021) Host defense peptides as immunomodulators: the other side of the coin. Peptides 146:170644
Alford MA, Baquir B, Santana FL et al (2020) Cathelicidin host defense peptides and inflammatory signaling: striking a balance. Front Microbiol 11:1902
Wang G, Chen Z, Tian P et al (2022) Wound healing mechanism of antimicrobial peptide cathelicidin-DM. Front Bioeng Biotechnol 10
Li S-A, Lee W-H, Zhang Y (2012) Efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in mouse models. Antimicrob Agents Chemother 56:3309–3317
Locke T, Parsons H, Briffa N et al (2022) A bundle of infection control measures reduces postoperative sternal wound infection due to Staphylococcus aureus but not Gram-negative bacteria: a retrospective analysis of 6903 patient episodes. J Hosp Infect 126:21–28
Roy S, Santra S, Das A et al (2020) Staphylococcus aureus biofilm infection compromises wound healing by causing deficiencies in granulation tissue collagen. Ann Surg 271:1174–1185
NCCLS (2003) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 6th edn. Approved standard M7-A6, National Committee for Clinical Laboratory Standards, Wayne
Andrews JM (2001) Determination of minimum inhibitory concentrations. J Antimicrob Chemother 48:5–16
Schlede E, Genschow E, Spielmann H et al (2005) Oral acute toxic class method: a successful alternative to the oral LD50 test. Regul Toxicol Pharmacol 42:15–23
Tatiya-Aphiradee N, Chatuphonprasert W, Jarukamjorn K (2019) Anti-inflammatory effect of Garcinia mangostana Linn. pericarp extract in methicillin-resistant Staphylococcus aureus-induced superficial skin infection in mice. Biomed Pharmacother 111:705–713
Shang L, Li J, Song C et al (2020) Hybrid antimicrobial peptide targeting Staphylococcus aureus and displaying anti-infective activity in a murine model. Front Microbiol 11:1767
Stoeber B, Ranamukha S, St. Clair R (2018) Intradermal delivery – new technology brings simplicity & scalability to intradermal drug delivery. Drug Deliv Development
Wolf RF, White GL (2012) Chapter 13 - Clinical techniques used for Nonhuman primates. In: Abee CR, Mansfield K, Tardif S et al (eds) Nonhuman Primates in Biomedical Research (Second Edition). Academic Press, Boston, pp 323–337
Moreira CF, Cassini-Vieira P, Canesso MCC et al (2021) Lactobacillus rhamnosus CGMCC 1.3724 (LPR) improves skin wound healing and reduces scar formation in mice. Probiotics Antimicrob Proteins 13:709–719
Huang H-N, Rajanbabu V, Pan C-Y et al (2013) Use of the antimicrobial peptide Epinecidin-1 to protect against MRSA infection in mice with skin injuries. Biomaterials 34:10319–10327
Driver AS, Kodavanti PRS, Mundy WR (2000) Age-related changes in reactive oxygen species production in rat brain homogenates. Neurotoxicol Teratol 22:175–181
Luck H (1974) Methods in enzymatic analysis II (ed.) Bergmeyer.(publ.). Academic Press, New York
Massey V, Williams CH (1965) On the reaction mechanism of yeast glutathione reductase. J Biol Chem 240:4470–4480
Al-Saedi ZHF, Salih ZT, Ahmed KK et al (2022) Formulation and characterization of oleogel as a topical carrier of azithromycin. AAPS PharmSciTech 24:17
Hema-Ouangraoua S, Tranchot-Diallo J, Zongo I et al (2021) Impact of mass administration of azithromycin as a preventive treatment on the prevalence and resistance of nasopharyngeal carriage of Staphylococcus aureus. PLoS ONE 16:e0257190
Hoepelman IM, Schneider MME (1995) Azithromycin: the first of the tissue-selective azalides. Int J Antimicrob Agents 5:145–167
Neu HC (1991) Clinical microbiology of azithromycin. Am J Med 91:S12–S18
Castle SS (2007) Ampicillin. In: Enna SJ, Bylund DB (eds) xPharm: the comprehensive pharmacology reference, Elsevier, New York, pp 1–6
Peechakara BV, Gupta M (2022) Ampicillin/sulbactam. In: StatPearls [Internet]. StatPearls publishing
Teethaisong Y, Autarkool N, Sirichaiwetchakoon K et al (2014) Synergistic activity and mechanism of action of Stephania suberosa Forman extract and ampicillin combination against ampicillin-resistant Staphylococcus aureus. J Biomed Sci 21:90
Watson A, Sauve K, Cassino C et al (2020) Exebacase demonstrates in vitro synergy with a broad range of antibiotics against both methicillin-resistant and methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother. https://doi.org/10.1128/aac.01885-19
Golan Y (2019) Current treatment options for acute skin and skin-structure infections. Clin Infect Dis 68:S206–S212
Dong C-L, Li L-X, Cui Z-H et al (2017) Synergistic effect of pleuromutilins with other antimicrobial agents against Staphylococcus aureus in vitro and in an experimental Galleria mellonella model. Front Pharmacol 8:553
Yameen A, Nasim H, Akhtar N et al (2010) Antibiotic susceptibility profile of methicillin-resistant staphylococci isolated from nasal samples of hospitalized patients. Afr J Microbiol Res 4:204–209
Moses VK, Kandi V, Rao SKD (2020) Minimum inhibitory concentrations of vancomycin and daptomycin against methicillin-resistant Staphylococcus aureus isolated from various clinical specimens: a study from South India. Cureus 12:e6749
Jo A, Ahn J (2016) Phenotypic and genotypic characterisation of multiple antibiotic-resistant Staphylococcus aureus exposed to subinhibitory levels of oxacillin and levofloxacin. BMC Microbiol 16:1–10
Ochoa R (2002) 14 - Pathology issues in the design of toxicology studies. In: Haschek WM, Rousseaux CG, Wallig MA (eds) Handbook of Toxicologic Pathology (Second Edition), Academic Press, San Diego, pp 307–26
Brody T (2018) Chapter 6 - Animal studies. In: Brody T (ed) FDA’s drug review process and the package label, Academic Press, pp 187–254
Agathokleous E, Moore MN, Calabrese EJ (2021) Estimating the no-observed-adverse-effect-level (NOAEL) of hormetic dose-response relationships in meta-data evaluations. MethodsX 8:101568
Strodtbeck F (2001) Physiology of wound healing. Newborn Infant Nurs Rev 1:43–52
Beldon P (2010) Basic science of wound healing. Surg Infect (Larchmt) 28:409–412
Negut I, Grumezescu V, Grumezescu AM (2018) Treatment strategies for infected wounds. Molecules (Basel, Switzerland) 23:2392
Cardona AF, Wilson SE (2015) Skin and soft-tissue infections: a critical review and the role of telavancin in their treatment. Clin Infect Dis 61:S69–S78
Jung C-J, Liao Y-D, Hsu C-C et al (2021) Identification of potential therapeutic antimicrobial peptides against Acinetobacter baumannii in a mouse model of pneumonia. Sci Rep 11:7318
Dijksteel GS (2021) Potential novel antimicrobial therapies for burn wounds: peptides and cold plasma. NARCIS
Gorr S-U, Flory CM, Schumacher RJ (2019) In vivo activity and low toxicity of the second-generation antimicrobial peptide DGL13K. PLoS ONE 14:e0216669-e
Ni Z, Wang B, Ma X et al (2016) Toxicology assessment of a dual-function peptide 5rolGLP-HV in mice. Appl Biochem Biotechnol 180:1276–1285
Cebrián R, Rodríguez-Cabezas ME, Martín-Escolano R et al (2019) Preclinical studies of toxicity and safety of the AS-48 bacteriocin. J Adv Res 20:129–139
El Shazely B, Yu G, Johnston PR et al (2020) Resistance evolution against antimicrobial peptides in Staphylococcus aureus alters pharmacodynamics beyond the MIC. Front Microbiol 11:103
Thomas RK, Melton R, Asbell PA (2019) Antibiotic resistance among ocular pathogens: current trends from the ARMOR surveillance study (2009–2016). Clin Optom (Auckl) 11:15–26
Miklasińska-Majdanik M (2021) Mechanisms of resistance to macrolide antibiotics among Staphylococcus aureus. Antibiotics (Basel) 10
Bojang A, Baines SL, Donovan L et al (2019) Genomic investigation of Staphylococcus aureus recovered from Gambian women and newborns following an oral dose of intra-partum azithromycin. J Antimicrob Chemother 74:3170–3178
Nigatu TA, Afework M, Urga K et al (2017) Toxicological investigation of acute and chronic treatment with Gnidia stenophylla Gilg root extract on some blood parameters and histopathology of spleen, liver and kidney in mice. BMC Res Notes 10:625
Adedapo AA, Abatan MO, Olorunsogo OO (2007) Effects of some plants of the spurge family on haematological and biochemical parameters in rats. Vet Arhiv 77:29–38
Adebayo JO, Yakubu MT, Egwim EC et al (2003) Effect of ethanolic extract of Khaya senegalensis on some biochemical parameters of rat kidney. J Ethnopharmacol 88:69–72
Vaidya VS, Ferguson MA, Bonventre JV (2008) Biomarkers of acute kidney injury. Annu Rev Pharmacol Toxicol 48:463–493
Schneider VAF, Coorens M, Tjeerdsma-van Bokhoven JL et al (2017) Imaging the antistaphylococcal activity of CATH-2: mechanism of attack and regulation of inflammatory response. mSphere 2:e00370-e417
Mangoni ML, McDermott AM, Zasloff M (2016) Antimicrobial peptides and wound healing: biological and therapeutic considerations. Exp Dermatol 25:167–173
Rishi P, Vashist T, Sharma A et al (2018) Efficacy of designer K11 antimicrobial peptide (a hybrid of melittin, cecropin A1 and magainin 2) against Acinetobacter baumannii-infected wounds. Pathog Dis 76:fty072
Polaka S, Katare P, Pawar B et al (2022) Emerging ROS-modulating technologies for augmentation of the wound healing process. ACS Omega 7:30657–30672
Dunnill C, Patton T, Brennan J et al (2017) Reactive oxygen species (ROS) and wound healing: the functional role of ROS and emerging ROS-modulating technologies for augmentation of the healing process. Int Wound J 14:89–96
Andrés CMC, Pérez de la Lastra JM, Juan CA et al (2022) Chemistry of hydrogen peroxide formation and elimination in mammalian cells, and its role in various pathologies. Stresses 2:256–274
Ransy C, Vaz C, Lombès A et al (2020) Use of H(2)O(2) to cause oxidative stress, the catalase issue. Int J Mol Sci 21
Nandi A, Yan LJ, Jana CK et al (2019) Role of catalase in oxidative stress- and age-associated degenerative diseases. Oxid Med Cell Longev 2019:9613090
Mishra S, Imlay J (2012) Why do bacteria use so many enzymes to scavenge hydrogen peroxide? Arch Biochem Biophys 525:145–160
Agarwal P, Singh A, Gaurav K et al (2009) Evaluation of wound healing activity of extracts of plantain banana (Musa sapientum var. paradisiaca) in rats
Rasik AM, Shukla A (2000) Antioxidant status in delayed healing type of wounds. Int J Exp Pathol 81:257–263
Acknowledgements
The author acknowledges the central instrumental facilities provided by SAIF/CIL, Panjab University, Chandigarh, India.
Funding
The study reported here was funded by DRDO, India and DST – FIST sanctioned to Department of Biophysics, Panjab University, India.
Author information
Authors and Affiliations
Contributions
P.B. and C.S. performed the experiments, P.B. compiled the main manuscript, S.J., S.S. and M.M. aided in interpretation of the results. P.R. and N.S. provided valuable inputs during manuscript preparation. A.S. designed the study, supervised all experiments during manuscript preparation, contributed to discussion and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Novel antimicrobial peptide DP1 is a promising alternative treatment to conventional antibiotics.
• DP1 is significantly less toxic as evident by its larger therapeutic window.
• Higher efficacy in healing Staphylococcus aureus infection wounds.
• DP1 reduces the Staphylococcus aureus colonization and bioburden contamination in wound infections.
• Regulates antioxidant levels and restores wound tissue.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barman, P., Sharma, C., Joshi, S. et al. In Vivo Acute Toxicity and Therapeutic Potential of a Synthetic Peptide, DP1 in a Staphylococcus aureus Infected Murine Wound Excision Model. Probiotics & Antimicro. Prot. (2023). https://doi.org/10.1007/s12602-023-10176-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s12602-023-10176-1