Abstract
Background
Circadian health refers to individuals’ well-being and balance in terms of their circadian rhythm. It is influenced by external cues. In adults, a close relationship between circadian-related alterations and obesity has been described. However, studies in children are scarce, and circadian health and its association with obesity have not been evaluated globally. We aimed to assess whether circadian health differed between children with and without obesity as determined by a global circadian score (GCS) in a school-age population.
Methods
Four hundred and thirty-two children (7–12 years) were recruited in Spain. Non-invasive tools were used to calculate the GCS: (1) 7-day rhythm of wrist temperature (T), activity (A), position (P), an integrative variable that combines T, A, and P (TAP); (2) cortisol; and (3) 7-day food and sleep records. Body mass index, body fat percentage, waist circumference (WC), melatonin concentration, and cardiometabolic marker levels were determined.
Results
Circadian health, as assessed by the GCS, differed among children with obesity, overweight, and normal weight, with poorer circadian health among children with obesity. Children with obesity and abdominal obesity had 3.54 and 2.39 greater odds of having poor circadian health, respectively, than did those with normal weight or low WC. The percentage of rhythmicity, a marker of the robustness of the TAP rhythm, and the amplitude, both components of the GCS, decreased with increasing obesity. Different lifestyle behaviors were involved in the association between circadian health and obesity, particularly protein intake (P = 0.024), physical activity level (P = 0.076) and chronotype (P = 0.029).
Conclusions
The GCS can capture the relationship between circadian health and obesity in school-age children. Protein intake, physical activity level, and chronotype were involved in this association. Early intervention based on improving circadian health may help to prevent childhood obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood obesity is a significant public health concern [1, 2]. Nevertheless, successful treatments for obesity in children are challenging [3], and the underlying causes of overweight at early ages should be investigated to improve the prevention and treatment of obesity in children. Chronobiology is an emerging science that studies the relationship between circadian rhythm alterations, chronodisruption, and pathology [4]. Recent studies link energy regulation to the circadian clock at the behavioral, physiological, and molecular levels [5, 6]. Circadian health refers to the well-being and balance of an individual’s circadian rhythm. It is influenced by external cues, most notably the light–dark cycle of day and night, but other behaviors, such as sleep/wake, eating/fasting, rest/activity, posture changes, and exercise, are also relevant factors [7].
We and others have shown that is more difficult in children with obesity than in those without obesity to maintain healthy biological rhythms (i.e., daily metabolic cycles in humans such as sleep–wake cycles, hormone release, eating habits and digestion, body temperature, and other functions repeated daily) [8]. Circadian-related behaviors such as late bedtimes and late eating have been associated with greater adiposity and obesity in children [9, 10]. However, studies on circadian health in school-age children are still scarce. Its relationship with obesity, including endogenous, behavioral, and environmental markers of circadian health, has not been evaluated globally.
Previously, we developed a global circadian score (GCS) that has been demonstrated to be reliable for assessing circadian health in children [11]. The score includes the following: (1) circadian-related markers such as the amplitude of the rhythm and rhythmicity characteristics of an integrative variable TAP, which combines wrist temperature (T) [12], physical activity (A) [13], and body position (P) [14]; (2) food timing, particularly breakfast and dinner timing [10]; and (3) endogenous circadian-related markers such as cortisol [15].
The hypothesis is that children with poor circadian health are more predisposed to suffer from obesity (and vice versa). Poor circadian health is considered a state in which children’s circadian rhythms are disrupted or not optimally aligned with the natural light–dark cycle [7]. The present study aimed to determine the potential association between circadian health and obesity in school-age children using a global marker of circadian health (GCS). We will also test the independent associations of several circadian-related features involved in the GCS with obesity.
Methods
Subjects
Healthy children (7–12 years; n = 432) from three schools in a Mediterranean area of Spain were recruited between October 2014 and June 2016 (ClinicalTrials.gov ID: NCT02895282), as previously described [11]. Approval for this study was obtained from the University of Murcia Ethics Committee (ID: 1868/2018). All procedures followed the ethical standards of the institutional and national research committees and complied with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The present study is a secondary analysis of the same cohort of children studied in our previous works [10, 11, 16,17,18].
Obesity-related trait measurements
Body weight, body fat percentage, and waist circumference (WC) were measured in the whole population (n = 432) on the first day of the week of the study and at the same time in the morning, as we previously published [11]. Body weight was measured in barefooted children wearing light clothes using a digital scale accurate to the nearest 0.1 kg. Height was determined using a portable stadiometer (rank: 0.14–2.10 m). The children were positioned upright, relaxed, and with their heads in the Frankfort plane. These data were used to calculate body mass index (BMI) according to the formula weight (kg)/height2 (m2). BMI was further transformed to the BMI Z-score according to the World Health Organization growth reference [19]. Total body fat was determined by bioelectrical impedance using TANITA TBF-300 equipment (Tanita Corporation of America, Arlington Heights, IL) [11]. Several cardiometabolic traits, such as glucose, triglyceride, and cholesterol levels, and inflammatory markers such as C-reactive protein, immunoglobulin A, interleukin (IL)-8, IL-1b, tumor necrosis factor-alpha and monocyte chemotactic protein 1 were determined from serum samples obtained from a subset of 79 children in the morning under fasting conditions as previously described [11].
Global circadian score determination
An already developed formula was used to determine the GCS for each child [11] (Supplementary Table 1). The score for each factor was calculated by multiplying each variable by its eigenvalue. Then, each factor score was multiplied by the percentage of the variance in the total information explained by that factor. Factors 1 and 2 explained 28% of the variance and were loaded mainly by TAP characteristics, factor 3 explained about 10% (loaded by cortisol measures), and factors 4 and 5 together explained about 13% of the variance and loaded on the timing of food intake (breakfast and dinner). The five factors together explained 50% of the variance in total information.
Factors and variables included in the GCS
A description of each variable included in the formula is presented in Table 1. Factors 1 and 2 from the GCS included variables derived from TAP. To determine TAP, children wore a wristwatch in their non-dominant hands during the seven days of the study. This wristwatch integrates two sensors: a temperature sensor [20] (Thermochron iButton DS1921H, Dallas, Maxim, Dallas, TX, USA), which is programmed to collect information every 5 minutes; and an accelerometer sensor (G Acceleration Data Logger UA-004–64; Onset Computer, Bourne, MA, USA), which measures physical activity and body position rhythms to record data every 30 seconds [14]. The position was expressed in degrees (°), and activity was expressed as the change in degrees per minute (Δ°/minute). TAP was calculated as previously described [14]. From TAP, different parameters were derived (Table 1) using an integrated package for temporal series analysis (Kronowizard; https://kronowizard.um.es/kronowizard; Chronobiology Laboratory, University of Murcia, Murcia, Spain, 2015). Factor 3 from the GCS comprised salivary cortisol measurements. Saliva samples were collected on the same day at three different times using salivates (Sarstedt, Barcelona, Spain): before breakfast (9:00), before lunch (14:00), and after dinner (23:00). The saliva concentration of cortisol was determined by radioimmunoassay (IZASA, Barcelona, Spain). Factors 4 and 5 from the GCS included dinner start time and finish time and breakfast start time and finish time determined by 7-day dietary records completed by children and parents. Melatonin and lunch timing were not included in the GCS because, in the factor analysis performed for developing the GCS, melatonin and lunch timing did not appear within the first five factors that accounted for about 50% of the variance.
Lifestyle variables
Sleep characteristics, individual chronotype, and related variables
We determined sleep timing, sleep duration, and daytime napping timing and duration using 7-day sleep diaries; children and parents recorded the wake/sleep cycle, which has been demonstrated to be a convenient tool for assessing sleep quality and duration [15, 21]. Individual chronotypes were subjectively determined using an age-appropriate Spanish version of the Munich ChronoType Questionnaire (MCTQ) [22], while melatonin was used as an objective proxy of individual chronotypes. Melatonin concentrations were determined via radioimmunoassay (IBL, Germany) in saliva samples collected at night (01:00) and before lunch (14:00). Social jet lag, which represents different sleep schedule behaviors between free days and schooldays, was measured as the difference between mid-sleep on free days and mid-sleep on schooldays. We considered that children had social jet lag when there was more than a two-hour difference in the midpoint of sleep between free days and school days [23].
Food intake
Energy and macronutrient distributions across meals and the percentage of energy provided by macronutrients were determined by 7-day food diaries adapted for this age group [24], which specify the timing of food intake, type of food and amount/weight/quantity of food eaten [15]. Total energy intake and macronutrient composition were analyzed with a nutritional evaluation software program (Grunumur 2.0 8) [25] based on Spanish food composition tables [26]. Total morning intake was defined as the sum of every intake in the morning, including lunch. Every intake after lunch, including dinner, was considered total evening intake. The timing of meals was determined by averaging every meal timing during the seven days of the dietary records completed by the children and parents.
Physical activity
The average physical activity was determined by an accelerometer (G Acceleration Data Logger UA-004–64; Onset Computer, Bourne, Massachusetts, USA) and was calculated as the average accumulative degree change in three-axis tilt per minute during the most active ten hours during the wake period (i.e., nonsleep time), which correlates with motor activity measured by the wrist-worn Actiwatch [11, 27]. We classified physical activity levels by dividing the average physical activity into tertiles (low, medium and high). The day–night physical activity contrast was determined as the relative amplitude of the activity rhythm.
Light exposure
We evaluated light exposure near the face (eyes) via a pendant luxmeter in the neck (HOBO Pendant Light Data Logger, UA-002–64; Onset Computer, Bourne, Massachusetts, USA). The instrument was programmed to collect light information continuously every 30 seconds for 7 days. We calculated the lux logarithm collected every 30 seconds to assess the light average. We further calculated the amplitude, percentage of rhythmicity (PR), interdaily stability (IS), and circadian function index (CFI) of the light data rhythm. The description and calculation of these variables are included in Table 1. Children were instructed to wear the pendant over their clothing. When sleeping, they had to leave it on the bedside table. Cortisol and melatonin salivary determinations were performed on Sundays after the 7-day recording of temperature, activity, position, and light was completed to avoid these determinations being affected by the melatonin sampling.
Statistical methods
Differences in GCS were analyzed among children stratified into groups according to three categories of obesity (children with normal weight, overweight and obesity) according to the sex- and age-specific BMI cutoff points proposed by the International Obesity Task Force [28] via ANCOVAs. When significant, we explored differences among groups using post hoc analysis (Bonferroni). The median GCS was used as a cutoff point for classifying children according to good or poor circadian health. We fitted multinomial logistic regression models to estimate the odds ratios and 95% confidence intervals of having poorer circadian health (as an outcome) in the presence of obesity/overweight (combination of overweight and obesity categories [28]) or high WC (divided according to the median, considering as "low WC" a WC lower or equal to 64 cm, and "high WC" a WC greater than 64 cm).
We tested for linear regression models of the GCS and its components with BMI, BMI Z-score, and body fat percentage. To understand the impact of lifestyle on the association between GCS and obesity, we explored the significant interactions between the GCS and lifestyle factors (already identified) and BMI. To identify those lifestyle factors, we previously tested linear regression models to determine whether there were significant associations between GCS and lifestyle factors or between the GCS and obesity traits (BMI, BMI Z-score, and body fat percentage). Because no significant interaction effect was found between sex and GCS for BMI, we performed statistical analyses of the total number of children studied without separating by sex. All analyses were performed using SPSS version 25.0 (SPSS, Chicago, Illinois, USA). P < 0.05 was considered to indicate statistical significance and is presented in the tables and figures in bold. The results of borderline statistical significance (considering those with P < 0.1) are presented in italics in all tables and figures.
We adjusted all analyses, including ANCOVA, multinomial logistic regression, linear regression, and interactions according to sex, age, race, and academic year. We chose those variables as a way to control for sociodemographic status.
Results
General characteristics, global circadian score, and obesity traits
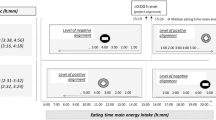
The GCS ranged from 385 to 1555, with higher values corresponding to better circadian health. Descriptive data on the GCS, obesity traits, and related lifestyle factors of the children studied are shown in Table 2. When children were classified into three categories according to their BMI (with obesity, with overweight, and with normal weight), the GCS differed across the three groups toward poorer circadian health among the children with obesity (Fig. 1a). We further classified children into two categories according to their GCS: poor circadian health, with a GCS lower than 1184.61; and good circadian health, with a GCS of 1184.61 or higher. Those children with obesity (determined according to the sex- and age-specific BMI cutoff points proposed by the International Obesity Task Force [28]) and with abdominal obesity (with high WC, if WC > 64 cm, classified according to the median) had 3.54 and 2.39 greater odds of having poor circadian health than those with normal weight [28] or with low WC (WC ≤ 64 cm), respectively (after adjusting for sex, age, race and academic year) (Fig. 1b). Secondary linear regression analyses between the GCS and several obesity-related inflammatory markers showed that the GCS was inversely correlated with C-reactive protein (a trend) (beta = -0.004 ng/mL; P = 0.058), while no significant associations were detected with the other inflammatory markers tested [immunoglobulin A, interleukin (IL)-8, IL-1b, tumor necrosis factor-alpha and monocyte chemotactic protein 1; P > 0.1].
Circadian health and obesity in children. a Differences in the global circadian score among children with normal weight (n = 268), overweight (n = 83), and obesity (n = 39) individuals classified according to International Obesity Task Force body mass index (BMI) cutoff points [28]. ANCOVA was performed, adjusting for sex, age, race, and academic year (P < 0.001). Significant differences were indicated between each pair of groups according to Bonferroni post hoc analyses (P = 0.036, normal weight vs. overweight; P < 0.001, normal weight vs. obesity; P = 0.022, overweight vs. obesity); b odds ratio (OR) and 95% confidence interval (CI) of poor vs. good circadian health with obesity. Obesity, in this case, is a combination of obesity and overweight according to the sex-and-age-specific BMI cutoff points proposed by the International Obesity Task Force [28]; waist circumference (WC) was classified according to the median, considering high WC when WC was greater than 64 cm (and low WC when WC was ≤ 64 cm). All analyses were adjusted for sex, age, race, and academic year. The values in bold are highlighted as statistically significant (P < 0.05)
In addition, several variables included in the GCS were independently associated with BMI and body fat percentage (Table 3). For the integrated TAP variable, the PR, amplitude, IS, CFI, and other circadian-related variables were inversely associated with BMI and BMI Z-score (P < 0.05). Cortisol level at 14:00 was also inversely associated with BMI and body fat percentage. In contrast, dinner start and finish time were directly associated with body fat percentage (toward later timing with greater body fat) (Table 3).
The role of lifestyle behaviors
Lifestyle factors information significantly associated with circadian health and obesity traits is presented in Table 4. Interestingly, earlier bedtime and awake time, longer duration of night sleep, shorter duration of daytime napping, less social jetlag, greater night-melatonin and day–night melatonin contrasts, greater energy intake in the morning, lower protein intake, and higher physical activity level were all factors related to better circadian health (higher GCS). In addition, a better daily pattern of light exposure with higher amplitude, increased PR, a greater IS, and a greater CFI (see Table 1 for definitions) was also associated with better circadian health. To evaluate the potential impact of different lifestyles on the association between circadian health and obesity, we tested for possible interactions between those factors associated with both circadian health and BMI/body fat percentage (i.e., bedtime, night sleep duration, night-melatonin, day–night melatonin contrast, total morning intake, protein intake, average physical activity and day–night activity contrast, and chronotype).
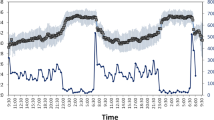
Figure 2 shows the significant results of the lifestyle–GCS interactions for BMI. When the protein intake was categorized into high, medium, and low protein intake groups based on tertiles of the protein percentage of total energy intake (measured in kcal), we identified differential effects across the three groups (interaction P = 0.024). For the low-protein intake group (represented by light gray circles), no significant association was found between circadian health and obesity (P = 0.138). In contrast, in the medium (dark gray squares) and high protein intake groups (black triangles), a higher BMI was associated with poorer circadian health (P < 0.05).
Lifestyle factor and global circadian score (GCS) interaction for body mass index (BMI). Predicted values of BMI according to tertile division of protein percentage of total energy intake (a), physical activity level (Δº/min) (b), and chronotype determined using the Munich chronotype questionnaire (MCTQ) score (c), plotted against the GCS. The predicted values for BMI (kg/m2) were calculated from the regression model after adjustment for age, sex, race, and academic year. Interaction P values indicate the statistical significance of the interaction term in the adjusted regression model (in bold, P < 0.05; in italics, P < 0.1). P values of each tertile indicate the statistical significance of the regression model between GCS and BMI within each tertile group for the protein percentage of total energy intake (a), physical activity level (Δº/min) (b), and chronotype determined using the MCTQ score (c)
Similarly, we identified differential effects across the three groups when children were categorized into high, medium, and low physical activity levels (interaction P = 0.076). For the high physical activity level group, no significant association was found between circadian health and obesity (P = 0.073), while significant associations were found between the medium and low activity level groups and higher BMI in children with poorer circadian health (P < 0.05).
Finally, we also identified significant differential effects across the individual chronotypes categorized into more morning, intermediate, and evening according to tertiles of Munich score (from the MCTQ; interaction P = 0.029). There was a significant association between circadian health and BMI in the morning and intermediate chronotypes (higher BMI with poorer circadian health, P < 0.05), while there was no significant association of circadian health with BMI in evening types (P = 0.181; Fig. 2).
Discussion
Traditionally used techniques for assessing circadian health are self-report questionnaires, which can be biased since they are subjective and depend on good recall and the subject’s ability to complete them correctly and honestly [29]. In recent years, non-invasive, more objective, and thus more accurate methods have been developed to assess circadian-related rhythms in children [13]. The rapid development of wearable devices has provided a more objective approach. Moreover, algorithms that derive metrics to quantify the robustness, phase, and stability of rhythms have been developed to search for new biomarkers of circadian health [30]. Nevertheless, these new tools and algorithms have yet to be used, especially in pediatric populations.
The current study demonstrated that the developed GCS [11], which integrates objective measures such as TAP and cortisol concentrations with meal timing, is easy to use, versatile, and non-invasive [11] and is a valuable tool for preventing and managing obesity through detecting poor circadian health and consequent intervention. Furthermore, this approach follows the recommended methods for identifying circadian-related effects for research or clinical practice [7]. Indeed, our novel GCS captured obesity in this population of school-age children. Those children with obesity and those with abdominal obesity had 3.54 and 2.39 greater odds of having poor circadian health, than did those with a normal weight or with low waist circumference, respectively.
Among all the variables included in the GCS, the variables most strongly associated with obesity were the PR, a marker of the prominence/robustness of the TAP rhythm [31]; amplitude, which shows the difference between day and night TAP values; and IS, which determines the constancy of the 24-hour rhythmic pattern over days. These results are consistent with previous studies showing that PR is inversely correlated with obesity and ghrelin levels [32], the hormone that induces appetite. On the other hand, the amplitude of daily rest–activity patterns is inversely associated with adiposity and cardiometabolic risk in a previous study performed in teenagers [33]. Similarly, in adults, lower values of amplitude at the wrist temperature ultradian peak (from a 12-hour rhythm) have been associated with higher metabolic syndrome risk and ghrelin [32]. In addition, in the current study, a low IS in TAP was related to a higher BMI. A low IS has been previously associated with a worse lipid profile and is considered a relevant cardiometabolic risk factor in adults [34, 35].
In general, in the current population of school-aged children, obesity is related to worse circadian health and a significantly lower GCS. We and others have previously shown that obesity is strongly associated with circadian-related alterations in adults [36,37,38]. Here, we have demonstrated that this is also true for school-age children. Interestingly, children with healthy lifestyle habits were more likely to have better circadian health (measured by the GCS) and less obesity, while the opposite was also true. For example, a higher energy intake in the morning was associated with better circadian health and a lower body fat percentage in our pediatric population. Previous studies have shown that eating breakfast (vs. not eating it) reduces the risk of obesity in children and adolescents [39]. Furthermore, our study revealed that higher protein intake was associated with poorer circadian health and higher BMI. A recent meta-analysis [40] showed that children with higher protein intake (from animal sources) were more likely to have a higher BMI. In addition, we found that protein intake per day interacted with the GCS score for the individual BMI, suggesting the potential influence of protein intake on the association between circadian health and obesity.
Similar interactions were obtained for physical activity. We found a significant association between higher BMI and poorer circadian health in children with low-medium activity levels, while in the higher activity group, this association was not detected; indeed, in the high-level physical activity group, the association between the physical activity average (log) and lower BMI was independent of the circadian health score (beta = – 24.71 kg/m2; P < 0.05), while this was not true for the other two groups (P > 0.05). Physical activity is considered the most modifiable factor of energy expenditure in school-age children, and higher physical activity levels are associated with lower BMI and percentage of body fat [41]. Furthermore, in our study, a greater contrast in day–night physical activity was associated with better circadian health and lower BMI. The day–night physical activity contrast is considered a marker of circadian-related alterations since a lower contrast is related to an impaired circadian system in young adults [42].
We also found a significant association between higher light exposure (average) and better daily patterns of light (higher amplitude, PR, IS, and CFI) and better circadian health (higher GCS). Previous studies have shown that a low amplitude of daily light in children, accompanied by a low day/night contrast in light due to higher light exposure during the evening/night, is associated with an impaired circadian system and melatonin secretion [43], as high light at night prevents the endogenous synthesis of melatonin by the pineal gland and reduces melatonin concentrations [44]. Melatonin is considered to be a sleep hormone because it is produced and secreted at night and is synthesized at a minimal level during the day [44]. In the present study, children with a low day/night contrast in melatonin had poorer circadian health and were more likely to have obesity. We previously reported that melatonin levels at 01:00 were lower in more evening-type children than in more morning-types, which could be related to circadian-related alterations [17] or poor circadian health.
Relatedly, in the current population, a higher Munich chronotype score, corresponding to a more evening type, tended to be associated with poorer circadian health (lower GCS) and a greater body fat percentage (both P < 0.1). We also found that those morning-type or intermediate-type children who had poorer circadian health (lower GCS), were more likely to have a higher BMI. However, those children with more evening chronotypes did not have a greater risk of obesity when they had poor circadian health. Our previous results showed that evening types, objectively determined as a higher value of TAP acrophase, were associated with higher BMI and metabolic alterations [17]. This finding suggested that the evening chronotype per se could be strongly associated with obesity, independent of circadian health.
In the discussion of our results, we need to consider several limitations. The cross-sectional design does not allow us to make inferences about the directionality or causality of the associations. We did not correct for multiple comparisons because all our outcomes are interrelated and the GCS comprises only one test of the relationship between obesity and circadian health. Therefore, future studies are needed to confirm our findings. Furthermore, while this GCS is based on objective and non-invasive measures, it may be challenging to be used in large-scale trials where saliva sampling is unavailable.
In conclusion, this study represents a significant step toward understanding novel aspects of the relationship between circadian health and obesity in school-age children. We demonstrated that the proposed GCS is a non-invasive and objective tool for detecting alterations in circadian health related to obesity (chronobesity). Due to its non-invasive nature, this score could be helpful in pediatric clinical practice. Emphasis should be placed on dietary intake (protein intake), physical activity, and individual chronotype, among other factors, to reduce the risk of obesity and improve overall health in children because these lifestyle factors might be involved in chrono-obesity. However, further intervention studies are needed to evaluate the effectiveness of behavioral interventions in modifying the GCS to reduce obesity.
Data availability
The datasets generated and analyzed during the current study are available in the Figshare repository (https://figshare.com/articles/dataset/Database_of_Global_Circadian_Score_in_Children/23717043).
References
Kostovski M, Tasic V, Laban N, Polenakovic M, Danilovski D, Gucev Z. Obesity in childhood and adolescence, genetic factors. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2017;38:121–33.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17:95–107.
Ryder JR, Fox CK, Kelly AS. Treatment options for severe obesity in the pediatric population: current limitations and future opportunities. Obesity (Silver Spring). 2018;26:951–60.
Laermans J, Depoortere I. Chronobesity: role of the circadian system in the obesity epidemic. Obes Rev. 2016;17:108–25.
Broussard JL, Van Cauter E. Disturbances of sleep and circadian rhythms: novel risk factors for obesity. Curr Opin Endocrinol Diabetes Obes. 2016;23:353–9.
Dibner C, Schibler U, Albrecht U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu Rev Physiol. 2010;72:517–49.
Klerman EB, Brager A, Carskadon MA, Depner CM, Foster R, Goel N, et al. Keeping an eye on circadian time in clinical research and medicine. Clin Transl Med. 2022;12:e1131.
Pereira LR, Moreira FP, Reyes AN, Bach SL, Amaral PLD, Motta JDS, et al. Biological rhythm disruption associated with obesity in school children. Child Obes. 2019;15:200–5.
Zhou M, Lalani C, Banda JA, Robinson TN. Sleep duration, timing, variability and measures of adiposity among 8- to 12-year-old children with obesity. Obes Sci Pract. 2018;4:535–44.
Martinez-Lozano N, Tvarijonaviciute A, Rios R, Baron I, Scheer F, Garaulet M. Late eating is associated with obesity, inflammatory markers and circadian-related disturbances in school-aged children. Nutrients. 2020;12:2881.
Barraco GM, Martinez-Lozano N, Vales-Villamarin C, Del Carmen BM, Rios R, Madrid JA, et al. Circadian health differs between boys and girls as assessed by non-invasive tools in school-aged children. Clin Nutr. 2019;38:774–81.
Krauchi K, Cajochen C, Werth E, Wirz-Justice A. Functional link between distal vasodilation and sleep-onset latency? Am J Physiol Regul Integr Comp Physiol. 2000;278:R741–8.
Martoni M, Carissimi A, Fabbri M, Filardi M, Tonetti L, Natale V. 24-h actigraphic monitoring of motor activity, sleeping and eating behaviors in underweight, normal weight, overweight and obese children. Eat Weight Disord. 2016;21:669–77.
Ortiz-Tudela E, Martinez-Nicolas A, Campos M, Rol MA, Madrid JA. A new integrated variable based on thermometry, actimetry and body position (TAP) to evaluate circadian system status in humans. PLoS Comput Biol. 2010;6:e1000996.
Garaulet M, Madrid JA. Methods for monitoring the functional status of the circadian system in dietary surveys studies: application criteria and interpretation of results. Nutr Hosp. 2015;31(Suppl 3):279–89.
Tvarijonaviciute A, Martinez-Lozano N, Rios R, Marcilla de Teruel MC, Garaulet M, Ceron JJ. Saliva as a non-invasive tool for assessment of metabolic and inflammatory biomarkers in children. Clin Nutr. 2020;39:2471–8.
Martinez-Lozano N, Barraco GM, Rios R, Ruiz MJ, Tvarijonaviciute A, Fardy P, et al. Evening types have social jet lag and metabolic alterations in school-age children. Sci Rep. 2020;10:16747.
Qian J, Martinez-Lozano N, Tvarijonaviciute A, Rios R, Scheer F, Garaulet M. Blunted rest-activity rhythms link to higher body mass index and inflammatory markers in children. Sleep. 2021;44:zsaa256.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Sarabia JA, Rol MA, Mendiola P, Madrid JA. Circadian rhythm of wrist temperature in normal-living subjects A candidate of new index of the circadian system. Physiol Behav. 2008;95:570–80.
Naismith SL, Rogers NL, Mackenzie J, Hickie IB, Lewis SJ. The relationship between actigraphically defined sleep disturbance and REM sleep behaviour disorder in Parkinson’s Disease. Clin Neurol Neurosurg. 2010;112:420–3.
Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11:429–38.
Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. Chronotype and social jetlag: a (self-) critical review. Biology (Basel). 2019;8:54.
Azevedo CSI, Paul K, MacLeish M, Mondejar M, Sarabia J, et al. Teaching chronobiology and sleep habits in school and university. Mind Brain Educ. 2008;2:34–47.
Perez-Llamas F, Garaulet M, Torralba C, Zamora S. Development of a current version of a software application for research and practice in human nutrition (GRUNUMUR 2.0). Nutr Hosp. 2012;27:1576–82 (in Spanish).
Moreiras O, Carvajal A, Cabrera, L. Table of composition of Spanish foods. Madrid, Spain: Pirámide; 1995 (in Spanish).
Bonmati-Carrion MA, Middleton B, Revell VL, Skene DJ, Rol MA, Madrid JA. Validation of an innovative method, based on tilt sensing, for the assessment of activity and body position. Chronobiol Int. 2015;32:701–10.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Martinez-Nicolas A, Martinez-Madrid MJ, Almaida-Pagan PF, Bonmati-Carrion MA, Madrid JA, Rol MA. Assessing chronotypes by ambulatory circadian monitoring. Front Physiol. 2019;10:1396.
Calogiuri G, Weydahl A, Carandente F. Methodological issues for studying the rest-activity cycle and sleep disturbances: a chronobiological approach using actigraphy data. Biol Res Nurs. 2013;15:5–12.
Refinetti R, Lissen GC, Halberg F. Procedures for numerical analysis of circadian rhythms. Biol Rhythm Res. 2007;38:275–325.
Corbalan-Tutau MD, Madrid JA, Ordovas JM, Smith CE, Nicolas F, Garaulet M. Differences in daily rhythms of wrist temperature between obese and normal-weight women: associations with metabolic syndrome features. Chronobiol Int. 2011;28:425–33.
Quante M, Cespedes Feliciano EM, Rifas-Shiman SL, Mariani S, Kaplan ER, Rueschman M, et al. Association of daily rest-activity patterns with adiposity and cardiometabolic risk measures in teens. J Adolesc Health. 2019;65:224–31.
Hoopes EK, Witman MA, D’Agata MN, Berube FR, Brewer B, Malone SK, et al. Rest-activity rhythms in emerging adults: implications for cardiometabolic health. Chronobiol Int. 2021;38:543–56.
Sohail S, Yu L, Bennett DA, Buchman AS, Lim AS. Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int. 2015;32:802–13.
Corbalan-Tutau MD, Gomez-Abellan P, Madrid JA, Canteras M, Ordovas JM, Garaulet M. Toward a chronobiological characterization of obesity and metabolic syndrome in clinical practice. Clin Nutr. 2015;34:477–83.
Garaulet M, Gomez-Abellan P. Chronobiology and obesity. Nutr Hosp. 2013;28(Suppl 5):114–20.
Gomez-Abellan P, Madrid JA, Ordovas JM, Garaulet M. Chronobiological aspects of obesity and metabolic syndrome. Endocrinol Nutr. 2012;59:50–61 (in Spanish).
Szajewska H, Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr. 2010;50:113–9.
Arnesen EK, Thorisdottir B, Lamberg-Allardt C, Barebring L, Nwaru B, Dierkes J, et al. Protein intake in children and growth and risk of overweight or obesity: a systematic review and meta-analysis. Food Nutr Res. 2022;66:8242.
Wyszynska J, Ring-Dimitriou S, Thivel D, Weghuber D, Hadjipanayis A, Grossman Z, et al. Physical activity in the prevention of childhood obesity: the position of the European Childhood Obesity Group and the European Academy of Pediatrics. Front Pediatr. 2020;8:535705.
Martinez-Nicolas A, Madrid JA, Rol MA. Day-night contrast as source of health for the human circadian system. Chronobiol Int. 2014;31:382–93.
Akacem LD, Wright KP Jr, LeBourgeois MK. Bedtime and evening light exposure influence circadian timing in preschool-age children: a field study. Neurobiol Sleep Circadian Rhythms. 2016;1:27–31.
Reiter RJ, Tan DX, Korkmaz A, Ma S. Obesity and metabolic syndrome: association with chronodisruption, sleep deprivation, and melatonin suppression. Ann Med. 2012;44:564–77.
Acknowledgements
We thank all children and their families and the three schools Maristas, San Antonio and San Pablo CEIP in Murcia, Spain, for their help and support: especially to Mari Carmen Blaya, Jose Ignacio Peña and María José Martínez. We thank all the staff of the Biochemistry Laboratory of the Rafael Mendez Hospital for their contribution to the implementation of the study.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was supported by the Spanish Society for the Study of Obesity (SEEDO) with the award of the 1st XLS Medical Scholarship for obesity research and by the Spanish Government of Investigation, Development and Innovation (SAF2017-84135-R) including FEDER co-funding, the Autonomous Community of the Region of Murcia through the Seneca Foundation (20795/PI/18) and NIDDK R01DK105072 granted to Marta Garaulet.
Author information
Authors and Affiliations
Contributions
GM conceptualized and designed the study and drafted the initial manuscript. RMM contributed to data analyses and final manuscript critical review and writing. MLN and TA collected data and samples, contributed to drafting the initial manuscript and critically reviewed the manuscript. MVS, PAG and RR collected data and samples. SD contributed to the formal analysis performing statistical interaction analyses and the revision of the article. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval
Approval for this study was obtained by the University of Murcia Ethics Committee (ID: 1868/2018). All procedures followed the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
No financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file3 (MPG 145035 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodríguez-Martín, M., Martínez-Lozano, N., Santaclara-Maneiro, V. et al. Children with obesity have poorer circadian health as assessed by a global circadian health score. World J Pediatr (2024). https://doi.org/10.1007/s12519-024-00804-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12519-024-00804-3