Abstract
Background
This study aimed to evaluate the feasibility and clinical effect of haploidentical hematopoietic stem cell transplantation (haplo-HSCT) for the treatment of pediatric patients with chronic active Epstein–Barr virus infection (CAEBV).
Methods
Children with CAEBV who did not have matched donors and underwent haplo-HSCT in Beijing Children’s Hospital, Capital Medical University, from October 2016 to June 2020 were analyzed retrospectively. Data relating to the clinical manifestations, engraftment, and prognosis of the children were extracted from medical records.
Results
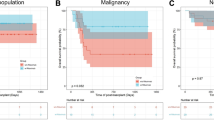
Twenty-five patients, including 16 males and 9 females, with an onset age of 5.0 ± 2.6 years and a transplantation age of 6.9 ± 2.9 years, were enrolled in this study. The mean time from diagnosis to transplantation was 3.8 (2.0–40.2) months. The mean observation time was 19.0 ± 12.0 months. Three patients received the reduced intensity conditioning regimen, and the remaining patients all received the modified myeloablative conditioning regimen. By the end of the follow-up, 23 patients were characterized by disease-free survival (DFS), 22 were characterized by event-free survival (EFS), and two died. One of the patients died of thrombotic microangiopathy (TMA), and another died of graft versus host disease (GVHD); this patient discontinued the treatment for economic reasons. The 3-year overall survival (OS) rate was estimated to be 92.0% ± 5.4%, and the 3-year EFS rate was estimated to be 87.4% ± 6.8%. All active patients survived after HSCT event-free. Acute GVHD degrees 1–3 were observed in ten patients (40.0%), and degree IV was observed in six (24.0%), who were all cured except for one patient. Chronic GVHD was observed in nine (36.0%), and most of these cases were mild. The incidence of TMA and veno-occlusive disease (VOD) was 28.0% and 4.0%.
Conclusions
Haploidentical hematopoietic stem cell transplantation is safe and effective in the treatment of pediatric CAEBV and can be used as an alternative therapy without matched donors or emergency transplantation. Patients with active disease before HSCT also benefited from haplo-HSCT. Haplo-HSCT requires careful monitoring for complications, such as GVHD and TMA. Early detection of TMA and timely treatment can reduce mortality and can improve the survival rate.

Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
References
Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from burkitt’s lymphoma. Lancet. 1964;1:702–3.
Kawa K. Epstein-Barr virus–associated diseases in humans. Int J Hematol. 2000;71:108–17.
Kimura H, Cohen JI. Chronic active epstein-barr virus disease. Front Immunol. 2017;8:1867.
Bollard CM, Cohen JI. How I treat T-cell chronic active Epstein-Barr virus disease. Blood. 2018;131:2899–905.
Sawada A, Inoue M, Kawa K. How we treat chronic active Epstein-Barr virus infection. Int J Hematol. 2017;105:406–18.
Okano M. Recent concise viewpoints of chronic active Epstein-Barr virus infection. Curr Pediatr Rev. 2015;11:5–9.
Okano M, Kawa K, Kimura H, Yachie A, Wakiguchi H, Maeda A, et al. Proposed guidelines for diagnosing chronic active Epstein-Barr virus infection. Am J Hematol. 2005;80:64–9.
Ohshima K, Kimura H, Yoshino T, Kim CW, Ko YH, Lee SS, et al. Proposed categorization of pathological states of EBV-associated T/natural killer-cell lymphoproliferative disorder (LPD) in children and young adults: overlap with chronic active EBV infection and infantile fulminant EBV T-LPD. Pathol Int. 2008;58:209–17.
Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31.
Harris AC, Young R, Devine S, Hogan WJ, Ayuk F, Bunworasate U, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: a report from the mount sinai acute GVHD international consortium. Biol Blood Marrow Transplant. 2016;22:4–10.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389-401.e1.
Cho BS, Yahng SA, Lee SE, Eom KS, Kim YJ, Kim HJ, et al. Validation of recently proposed consensus criteria for thrombotic microangiopathy after allogeneic hematopoietic stem-cell transplantation. Transplantation. 2010;90:918–26.
Bonifazi F, Barbato F, Ravaioli F, Sessa M, Defrancesco I, Arpinati M, et al. Diagnosis and treatment of VOD/SOS After allogeneic hematopoietic stem cell transplantation. Front Immunol. 2020;11:489.
Hamidieh AA, Pourpak Z, Hosseinzadeh M, Fazlollahi MR, Alimoghaddam K, Movahedi M, et al. Reduced-intensity conditioning hematopoietic SCT for pediatric patients with LAD-1: clinical efficacy and importance of chimerism. Bone Marrow Transplant. 2012;47:646–50.
Henter JI, Samuelsson-Horne A, Aricò M, Egeler RM, Elinder G, Filipovich AH, et al. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100:2367–73.
Ma H, Zhang L, Wei A, Jun Y, Dong W, Qing Z, et al. Outcome of L-DEP regimen for treatment of pediatric chronic active Epstein-Barr virus infection. Orphanet J Rare Dis. 2021;16:269.
Mahlaoui N, Ouachée-Chardin M, de Saint BG, Neven B, Picard C, Blanche S, et al. Immunotherapy of familial hemophagocytic lymphohistiocytosis with antithymocyte globulins: a single-center retrospective report of 38 patients. Pediatrics. 2007;120:e622–8.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Jia C, Wang B, Zhu G, Zhang R, Wang K, Yan Y, et al. Haploidentical hematopoietic stem cell transplantation using reduced-intensity conditioning for pediatric patients with familial hemophagocytic lymphohistiocytosis. Pediatr Investig. 2019;2:216–21.
Okamura T, Kishimoto T, Inoue M, Honda M, Yamashita N, Wakiguchi H, et al. Unrelated bone marrow transplantation for Epstein-Barr virus-associated T/NK-cell lymphoproliferative disease. Bone Marrow Transplant. 2003;31:105–11.
Kimura H, Ito Y, Kawabe S, Gotoh K, Takahashi Y, Kojima S, et al. EBV-associated T/NK-cell lymphoproliferative diseases in nonimmunocompromised hosts: prospective analysis of 108 cases. Blood. 2012;119:673–86.
Sato E, Ohga S, Kuroda H, Yoshiba F, Nishimura M, Nagasawa M, et al. Allogeneic hematopoietic stem cell transplantation for Epstein-Barr virus-associated T/natural killer-cell lymphoproliferative disease in Japan. Am J Hematol. 2008;83:721–7.
Arai A. Advances in the study of chronic active Epstein-Barr Virus infection: clinical features under the 2016 WHO classification and mechanisms of development. Front Pediatr. 2019;7:14.
Fujiwara S, Nakamura H. Chronic active Epstein-Barr Virus infection: is it immunodeficiency, malignancy, or both? Cancers (Basel). 2020;12:3202.
Kawa K, Sawada A, Sato M, Okamura T, Sakata N, Kondo O, et al. Excellent outcome of allogeneic hematopoietic SCT with reduced-intensity conditioning for the treatment of chronic active EBV infection. Bone Marrow Transplant. 2011;46:77–83.
Gotoh K, Ito Y, Shibata-Watanabe Y, Kawada J, Takahashi Y, Yagasaki H, et al. Clinical and virological characteristics of 15 patients with chronic active Epstein-Barr virus infection treated with hematopoietic stem cell transplantation. Clin Infect Dis. 2008;46:1525–34.
Yang J, Zhu GH, Wang B, Zhang R, Jia CG, Yan Y, et al. Haploidentical hematopoietic stem cell transplantation for xiap deficiency: a single-center report. J Clin Immunol. 2020;40:893–900.
Leon Rodriguez E, Rivera Franco MM, Perez Alvarez SI. Reduced BUCY 2 and G-CSF-primed bone marrow associates with low graft-versus-host-disease and transplant-related mortality in allogeneic HSCT. Ann Hematol. 2017;96:1525–31.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006;107:3065–73.
Chang YJ, Huang XJ. Haploidentical bone marrow transplantation without T-cell depletion. Semin Oncol. 2012;39:653–63.
George JN, Li X, McMinn JR, Terrell DR, Vesely SK, Selby GB. Thrombotic thrombocytopenic purpura-hemolytic uremic syndrome following allogeneic HPC transplantation: a diagnostic dilemma. Transfusion. 2004;44:294–304.
Epperla N, Li A, Logan B, Fretham C, Chhabra S, Aljurf M, et al. Incidence, risk factors for and outcomes of transplant-associated thrombotic microangiopathy. Br J Haematol. 2020;189:1171–81.
Laskin BL, Goebel J, Davies SM, Jodele S. Small vessels, big trouble in the kidneys and beyond: hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Blood. 2011;118:1452–62.
Xiao H, Hu B, Luo R, Hu H, Zhang J, Kuang W, et al. Chronic active Epstein-Barr virus infection manifesting as coronary artery aneurysm and uveitis. Virol J. 2020;17:166.
Xiao H, Hu B, Luo R, Hu H, Zhang J, Kuang W, et al. Cardiovascular complications associated with chronic active Epstein-Barr virus infection. Pediatr Cardiol. 2009;30:274–81.
Kernan NA, Grupp S, Smith AR, Arai S, Triplett B, Antin JH, et al. Final results from a defibrotide treatment-IND study for patients with hepatic veno-occlusive disease/sinusoidal obstruction syndrome. Br J Haematol. 2018;181:816–27.
Acknowledgements
We thank all of the patients and their families for their kind cooperation. We thank all of the members of clinical team who provided care for patients. This work was supported by Beijing Municipal Science & Technology Commission (No. Z171100001017050) and National Science and Technology Key Projects (No. 2017ZX09304029001).
Funding
No funding.
Author information
Authors and Affiliations
Contributions
YHL, JY and AW contributed equally to this paper. YHL and AW designed and performed the literature search and drafted the manuscript. YHL and AW contributed equally to this work. BW, GHZ, RZ, CGJ, YY, KW, XZ and SDL analyzed the data, and verified and discussed the studies. JY, TYW and MQQ amended the paper, designed the research, proofread the manuscript, supervised and approved the study.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Beijing Children’s Hospital, Capital Medical University ([2021]-A-123-R). Informed consent to participate in the study have been obtained from their parent or legal guardian in the case of children under 16.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, YH., Yang, J., Wei, A. et al. Haploidentical hematopoietic stem cell transplantation for pediatric patients with chronic active Epstein–Barr virus infection: a retrospective analysis of a single center. World J Pediatr 17, 626–636 (2021). https://doi.org/10.1007/s12519-021-00470-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00470-9