Abstract
Background
Microcalcifications cannot be identified with the present resolution of CT; however, 18F-sodium fluoride (18F-NaF) positron emission tomography (PET) imaging has been proposed for non-invasive identification of microcalcification. The primary objective of this study was to assess whether 18F-NaF activity can assess the presence and predict the progression of CT detectable vascular calcification.
Methods and Results
The data of two longitudinal studies in which patients received a 18F-NaF PET-CT at baseline and after 6 months or 1-year follow-up were used. The target to background ratio (TBR) was measured on PET at baseline and CT calcification was quantified in the femoral arteries at baseline and follow-up. 128 patients were included. A higher TBR at baseline was associated with higher calcification mass at baseline and calcification progression (β = 1.006 [1.005-1.007] and β = 1.002 [1.002-1.003] in the studies with 6 months and 1-year follow-up, respectively). In areas without calcification at baseline and where calcification developed at follow-up, the TBR was .11–.13 (P < .001) higher compared to areas where no calcification developed.
Conclusion
The activity of 18F-NaF is related to the amount of calcification and calcification progression. In areas where calcification formation occurred, the TBR was slightly but significantly higher.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis is a major cause of disability and death worldwide.1 The amount of arterial calcification is a surrogate imaging marker of the burden of atherosclerotic disease. In an early stage, calcification in the form of microcalcifications can be histologically observed. Microcalcifications are associated with inflammation and unstable high-risk plaques. In a later stage, extensive macrocalcifications develop which are thought to stabilize the plaque.2,3 Computed tomography (CT)-based quantification of calcification is commonly performed for the coronary arteries, where it is an established predictor of cardiovascular disease.4 However, the present resolution of CT allows identification of macrocalcifications, but not of microcalcifications. Therefore, 18F-sodium fluoride (18F-NaF) positron emission tomography (PET) imaging has been proposed for non-invasive identification of areas with microcalcification, to bridge the gap between what can be measured with histology and with CT. However, the availability of data on 18F-NaF PET is limited and validation studies are challenging.
Higher 18F-NaF uptake is associated with cardiovascular risk factors.5,6,7 In bone imaging, 18F-NaF binds to the surface of hydroxyapatite crystals. Subsequently, the hydroxyl ion is exchanged with the 18fluoride ion on the surface of hydroxyapatite to form fluorapatite. Vascular 18F-NaF uptake might therefore be a measure of the calcification surface area and able to visualize smaller calcifications than CT as these microcalcifications have a large surface area relative to the amount of calcium.8 It has also been proposed that 18F-NaF specifically binds areas of microcalcification, and therefore can identify areas of active calcification.9 We performed a longitudinal study to assess whether 18F-NaF activity is associated with incident and progressive vascular calcification on CT in the femoral arteries, which is an arterial bed where motion artifacts do not play a major role.
Methods
For this study, data from two longitudinal medication studies (TEMP and VITACAL trial, trialregister.nl NL4956 and NL5147) in which patients underwent an 18F-NaF PET-CT at baseline and after 1 year (TEMP) or 6 months (VITACAL) follow-up were used. In both studies, TBR on PET and calcium mass on CT were measured at baseline and follow-up.
TEMP
The Treatment of Ectopic Mineralization in Pseudoxanthoma Elasticum Trial (TEMP) was a single center, randomized, double-blind, placebo-controlled trial conducted in the University Medical Center Utrecht in the Netherlands. Patients with a clinical diagnosis of Pseudoxanthoma Elasticum (PXE),10 aged ≥ 18 years and with evidence of arterial calcification on a CT of the lower limbs were included. In total, 74 patients were randomized between 1 year treatment with a bisphosphonate (etidronate) and placebo. At baseline and after 1-year treatment, a full body 18F-NaF PET-CT was performed. The study was previously described in detail.11
VITACAL
The VItamin K and vascular calcification (VITACAL) study was a single center, randomized, double-blind, placebo-controlled trial conducted in the University Medical Center Utrecht in the Netherlands. Patients diagnosed with diabetes mellitus type 2, aged ≥ 40 with presence of arterial disease (Ankle Brachial Index < .9 and/or diagnosed with arterial disease by physician) were included. Patients were randomized between 6 months treatment with 360 microgram vitamin K (menaquinone-7) daily and placebo. At baseline and after 6 months treatment a full body 18F-NaF PET-CT was performed. The study was previously described in detail.12
Data Acquisition
The CT and PET acquisition parameters were described previously.11,12 In all patients, calcifications in both femoral arteries were quantified on CT using dedicated software (iX Viewer, Image Sciences Institute, University Medical Center Utrecht, Utrecht, The Netherlands). A threshold of 130 Hounsfield Units was applied, and the observer manually selected arterial calcifications above this threshold with a single mouse click. Subsequently, the calcification mass score was calculated. The mass equivalent score was computed as the product of the mean attenuation in a lesion and the volume of that lesion. Scoring was started a centimeter below the bifurcation of the communal femoral artery up till the femur condyles.
On PET the standardized uptake value (SUVmax) was determined by manually drawing a circular region of interest (ROI) around the femoral artery on every other slice (slice thickness 5 mm, increment 4 mm). The mean SUVbackground was determined by using the average of three ROIs drawn in the superior vena cava at the level of the aortic arch on consecutive slices. The target to background ratio (TBR) was calculated by dividing the SUVmax by the SUVbackground. The observer was blinded for treatment status and clinical information.
To determine calcification progression in individual image slices, slices at baseline and follow-up were aligned. For each lower limb in each acquisition, calcium mass score profiles along the femoral artery were determined. An example is provided in Figure 1. Because calcification progression in 6 months or 1 year is typically limited, these profiles should correlate for baseline and follow-up. In patients where there was poor alignment, a translation of the follow-up CT scan was applied to create a better fit. The translation was performed by one observer (AH), after which profiles with and without translation were anonymized and scored by two observers (JB, PJ). Each observer chose which plot fitted better and provided a score: (1) perfect overlap, (2) moderate overlap, and (3) poor overlap. All plots in which only one of the observers scored 3 or when the observers had a different plot preference were discussed in a consensus meeting with all three observers. In the consensus meeting, it was decided whether to include the data or not. If both observers scored 3, data were excluded from further analysis. Plots of all patients are provided in Online Appendix 1 (TEMP) and Online Appendix 2 (VITACAL). The result of the matching was one final dataset that included per patient, per lower limb, per slice the calcium mass at baseline and follow-up, the TBR at baseline, and the delta calcium mass. The delta calcium mass was calculated by subtracting the calcium mass at baseline from the calcium mass at follow-up.
Example of alignment. Example of alignment of baseline and follow-up acquisition using the amount of calcification. The continuous line shows calcification at baseline, and the dashed line represents the follow-up acquisition. In the upper figure (before translation), the two lines do not overlap. By moving the dashed follow-up line two slices to the left, a better fit is achieved
Statistical Analysis
Statistical analysis was performed with RStudio version 1.1.414 (RStudio Team, Boston, USA). Data are provided as mean ± standard deviation in case of a normal distribution and as median [interquartiles] if non-normally distributed. Categorical variables are provided as N (percentage).
A multilevel linear model was used since data were clustered per patient and per side. The natural log transformation of the TBR (as measured at baseline) was used as dependent variable, adjusted for age, gender, BMI and renal function (creatinine level). Subsequently, stratified analyses per treatment group were performed. Presented are the results after back transformation.
Subgroup analysis was performed in slices without calcium at baseline. Slices in which calcium progression occurred were compared to slices without calcium at follow-up.
Finally, we investigated whether high TBR values were associated with calcium progression. This was only investigated in the placebo group, since treatment might interfere with calcium progression. From all slices without calcium at baseline, the slice with the highest TBR at baseline was selected in each patient in each lower limb. This was defined as the ‘hottest slice’. If multiple slices had the same highest TBR, they were all marked as the hottest slice. The calcium mass at follow-up on these hottest slices was compared to the remaining slices using the Mann–Whitney-U test.
Results
TEMP
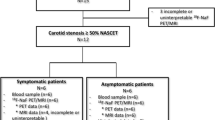
In total 74 patients were included. One patient did not receive the follow-up scan and was therefore excluded. After the consensus meeting seven lower limbs in six different patients (in one patient both limbs, in five patients one limb) were excluded because the baseline and follow-up data could not be matched sufficiently. Ultimately, 72 patients (139 lower limbs) were included with 6,294 slices in total. Forty-one percent (2,603/6,294) of the CT slices showed calcium at baseline. Of those slices, 1,108 slices (43%) showed calcium progression at follow-up. The baseline TBR of those slices was 3.2 compared to 3.1 in slices without calcium progression (P = .67). Baseline characteristics are provided in Table 1. A flowchart is provided in Figure 2. Figure 3 shows the correlation between the TBR and the calcium mass.
Results of univariate analysis are provided in Online Appendix 3. Multivariate analysis (Table 2) showed that a higher TBR was positively associated with both an increase in the delta calcium mass (β = 1.002 [1.002-1.003], P < .001) and the amount of calcium at baseline (β = 1.006 [1.005-1.006], P < .001). Analysis stratified per group (placebo or etidronate) showed the same direction and effect sizes (Online Appendix 4).
There were 3,691 slices without calcium at baseline. In 8% (286 slices) of those slices, calcium developed at follow-up. Figure 4 shows that slices in which calcium developed at follow-up have a higher TBR at baseline. In multivariate analysis, slices without CT calcium at baseline in which calcium developed at follow-up showed a TBR at baseline which was .13 higher compared to slices in which no calcium formation occurred (β = 1.131 [1.105-1.159], P < .001).
18F-NaF activity and calcium progression. Relationship between baseline TBR and calcium progression in the placebo groups in slices without calcium at baseline. Slices in which calcium progression is seen at follow-up have a higher TBR at baseline in both studies (P < .001 in both studies). FU, Follow-Up; TBR, Target to Background Ratio
The hottest slice analysis in slices without calcium at baseline in the placebo group showed that the progression of the calcium mass at follow-up was significantly higher for the hottest slice (slice with the highest TBR at baseline, P < .001). The hottest slice (148 slices) showed a mean calcium mass score at follow-up of 3.204 (SD 8.684) vs 1.064 (SD 4.728) in the 1,525 other slices (P < .001). In 20% (30/148) of the hottest slices and in 8% (129/1,525) of the remaining slices calcium developed at follow-up. Figure 5 shows the mean calcium mass for the hottest slice compared to the other slices.
VITACAL
In total 68 patients were included in the VITACAL study. Eight patients did not receive the follow-up scan and were therefore excluded. After the consensus meeting 18 lower limbs in 14 different patients (in four patient both limbs, in ten patients one limb) were excluded. Therefore 56 patients (101 lower limbs) were included with 4,642 slices in total. Forty-eight percent (2,212/4,642) of the slices showed calcium at baseline. Of those slices, 1,152 slices (25%) showed calcium progression at follow-up. The baseline TBR of those slices was 2.7 compared to 2.6 in slices without calcium progression (P = .01). Baseline characteristics are provided in Table 1. Figure 3 shows the correlation between the TBR and the calcium mass.
Multivariate analysis (Table 2) showed that a higher TBR was associated with both an increase in the delta calcium mass (β = 1.006 [1.005-1.007], P < .001) and the amount of calcium at baseline (β = 1.014 [1.013-1.014], P < .001). Analysis stratified per group (placebo or vitamin K) showed the same direction and effect sizes (supplement 4).
There were 2,430 slices without calcium at baseline. In 13% (322 slices) of those slices, calcium developed at follow-up. Figure 4 shows that slices in which calcium develop at follow-up have a higher TBR at baseline. In multivariate analysis, slices without CT calcium at baseline in which calcium developed at follow-up show a TBR at baseline which is .11 higher compared to slices in which no calcium formation occurred (β = 1.113 [1.084-1.142], P < .001).
The hottest slice analysis in slices without calcium at baseline in the placebo group showed that the progression of the calcium mass at follow-up was not significantly different for the hottest slice (slice with the highest TBR at baseline). The hottest slice (32 slices) showed a mean calcium mass score at follow-up of .304 (SD 1.098) vs .345 (SD 1.097) in the 1,321 other slices (P = .960). In 3/32 (9%) of the hottest slices and in 130/1,321 (10%) of the remaining slices calcium developed at follow-up. Figure 5 shows the mean calcium mass for the hottest slice compared to the other slices.
Discussion
In this longitudinal study, 18F-NaF PET uptake showed a weak positive relation with the amount of CT calcification, CT calcification progression and newly developed CT calcifications. Although a higher TBR in areas without calcium at baseline was related to the occurrence of calcification at follow-up, the difference was small (.11-.13) and therefore the clinical relevance might be limited.
Longitudinal studies which assess the relationship between 18F-NaF activity and disease progression are limited and involve small patient groups. Jenkins et al.13 assessed aortic valve calcification in 99 patients. 18F-NaF activity was strongly correlated to both the amount of calcium at baseline and calcium progression. However, 18F-NaF activity was not able to independently predict clinical outcomes (cardiovascular death and aortic valve replacement). Ishiwata et al.14 retrospectively evaluated 34 patients who underwent a PET-CT because of malignancy or orthopedic diseases. Follow-up was after 1 year (for calcified plaques) or more than 2 years (for 18F-NaF active sites) with a large range in follow-up. The aorta and the common iliac artery were studied. There was no correlation between 18F-NaF activity and baseline calcium; however, the difference in calcium volume and Agatston calcium score were associated with a higher 18F-NaF activity. No correction for potential confounders was performed. De novo calcification occurred in 19/96 (20%) of the hotspots and was related to a longer follow-up interval of on average 5 years, but was not related to a higher TBR at baseline. In the current study de novo calcifications occurred in 20% (TEMP) and 9% (VITACAL) of the hotspots.
It would be very promising if a non-invasive biomarker could distinguish between microcalcifications in high-risk plaques and macrocalcifications in relatively stable plaques. Ex vivo research was performed by Irkle et al.9 in excised carotid endarterectomy specimens. Electron microscopy was compared with immunohistochemical analysis and 18F-NaF adsorption. Tissue fluoride was only found in the presence of calcification and microcalcifications showed greater levels of fluoride compared to macrocalcifications. 18F-NaF did only bind to the surface of the micro- and macrocalcifications. Recently, Creager et al.15 in vitro and ex vivo confirmed that 18F-NaF binds to the surface of both micro- and macrocalcifications. 18F-NaF is a marker of active calcification which is more likely to occur in the early stages of plaque formation, and not a specific marker of microcalcification. This explains the relationship between the amount of calcification and 18F-NaF activity, which was also reported in several earlier studies.5,16
Of special interest are areas without calcification, as measured on CT, but with increased 18F-NaF activity. These might represent areas with microcalcifications, not yet detectable by CT. In both studies we found that the hottest slice at baseline had a higher calcification mass at follow-up. In the literature, several different methods are used to define hotspots. Hotspots can be defined visually, using a fixed cut-off or using a study or patient specific cut-off as was performed in the current study. Since 18F-NaF activity is dependent on many variables such as age, BMI, renal function, injected dose and PET technology,17,18 it is difficult to define a fixed cut-off TBR.
This study has several limitations. First, both studies were clinical trials evaluating a bisphosphonate and vitamin K, respectively. Since the TBR was defined at baseline, it is not possible that this was influenced by treatment. However, the delta calcium can be influenced since the TEMP trial showed that bisphosphonate treatment reduced the amount of arterial calcification.11 Subgroup analysis in the placebo group, however, showed the same results. Second, because the TEMP and the VITACAL concerned very different patient populations and follow-up time the results were not pooled, although pooling of results would have increased the power of the study. Third, the inclusion criteria of both studies resulted in a study population with a high prevalence of femoral artery macrocalcifications, while 18F-NaF activity might allow identification of microcalcifications. Fourth, the coronary arteries, carotid bifurcation and aorta are vascular beds in which atherosclerosis is dominant, but in the femoral artery also medial arterial calcifications occur.19,20 In PXE patients, calcification of elastin fibers in the medial arterial wall occur which is different from atherosclerosis which is characterized by calcification of the intimal layer.21 Therefore, the results in PXE patients might not be generalizable to the atherosclerosis in general. In patients with diabetes, which was an inclusion criterion of the VITACAL study, medial artery calcifications of the lower limb are common.22 This may have influenced the associations between PET and CT in our study as the surface area of medial arterial calcification relative to atherosclerotic microcalcification is uncertain. However, the femoral artery is an arterial bed where motion artifacts do not play a major role. Furthermore, detection of iliofemoral plaques may identify earlier manifestations of atherosclerosis and can be detected in young individuals before the development of coronary calcifications.23 Fifth, the length of follow-up was relatively short, since progression of calcification is a slow process. Finally, we choose to use the calcium mass equivalent score for quantification of calcification in the femoral arteries, instead of the Agatston score which is typically used for calcium quantification in the coronary arteries. This is based on previous studies which show that the calcium mass allows for more robust quantification and shows better reproducibility than the Agatston score.24,25
Conclusions
In conclusion this is the first longitudinal study showing that 18F-NaF activity in the femoral arteries is associated with the amount of CT calcification and CT calcification progression. Areas in which CT calcification occurred at follow-up, showed a slightly higher TBR at baseline, although the differences were small. This supports the concept that PET can detect calcifications below the resolution of CT to some extent, which may be of interest for studies in persons who do not have CT detectable calcifications.
New Knowledge Gained
This study showed that 18F-NaF activity in the femoral arteries is related to the amount of calcification and calcification progression. To some extent, PET-CT can detect calcifications below the resolution of CT, and identify locations where calcifications are likely to develop on CT. This may be of interest for intervention studies in the early phases of the calcification process.
Abbreviations
- 18F-NaF:
-
18F-sodium fluoride
- BMI:
-
Body Mass Index
- CT:
-
Computed Tomography
- PET:
-
Positron Emission Tomography
- PXE:
-
Pseudoxanthoma Elasticum
- ROI:
-
Region Of Interest
- SUV:
-
Standardized Uptake Value
- TBR:
-
Target to Background Ratio
- TEMP:
-
Treatment of Ectopic Mineralization in Pseudoxanthoma Elasticum
References
Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. 2016;118:535–46.
Mori H, Torii S, Kutyna M, Sakamoto A, Finn AV, Virmani R. Coronary artery calcification and its progression: What does it really mean? JACC Cardiovasc Imaging. 2018;11:127–42.
Pugliese G, Iacobini C, Blasetti Fantauzzi C, Menini S. The dark and bright side of atherosclerotic calcification. Atherosclerosis. 2015;238:220–30.
Hoffmann U, Massaro JM, D’Agostino RBS, Kathiresan S, Fox CS, O’Donnell CJ. Cardiovascular event prediction and risk reclassification by coronary, aortic, and valvular calcification in the Framingham Heart Study. J Am Heart Assoc. 2016. https://doi.org/10.1161/jaha.115.003144.
Dweck MR, Chow MW, Joshi NV, Williams MC, Jones C, Fletcher AM, et al. Coronary arterial 18F-sodium fluoride uptake: A novel marker of plaque biology. J Am Coll Cardiol. 2012;59:1539–48.
Li Y, Berenji GR, Shaba WF, Tafti B, Yevdayev E, Dadparvar S. Association of vascular fluoride uptake with vascular calcification and coronary artery disease. Nucl Med Commun. 2012;33:14–20.
Oliveira-Santos M, Castelo-Branco M, Silva R, Gomes A, Chichorro N, Abrunhosa A, et al. Atherosclerotic plaque metabolism in high cardiovascular risk subjects - A subclinical atherosclerosis imaging study with (18)F-NaF PET-CT. Atherosclerosis. 2017;260:41–6.
Nakahara T, Narula J, Strauss HW. NaF uptake in unstable plaque: What does fluoride uptake mean? Eur J Nucl Med Mol Imaging. 2018;45:2250–2.
Irkle A, Vesey AT, Lewis DY, Skepper JN, Bird JL, Dweck MR, et al. Identifying active vascular microcalcification by (18)F-sodium fluoride positron emission tomography. Nat Commun. 2015;6:7495.
Plomp AS, Toonstra J, Bergen AA, van Dijk MR, de Jong PT. Proposal for updating the Pseudoxanthoma Elasticum classification system and a review of the clinical findings. Am J Med Genet A. 2010;152A:1049–58.
Kranenburg G, de Jong PA, Bartstra JW, Lagerweij SJ, Lam MG, Ossewaarde-van Norel J, et al. Etidronate for prevention of ectopic mineralization in patients with Pseudoxanthoma elasticum. J Am Coll Cardiol. 2018;71:1117–26.
Zwakenberg SR, de Jong PA, Bartstra JW, van Asperen R, Westerink J, de Valk H, et al. The effect of menaquinone-7 supplementation on vascular calcification in patients with diabetes: A randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2019;110(4):883–90.
Jenkins WS, Vesey AT, Shah AS, Pawade TA, Chin CW, White AC, et al. Valvular (18)F-fluoride and (18)F-fluorodeoxyglucose uptake predict disease progression and clinical outcome in patients with aortic stenosis. J Am Coll Cardiol. 2015;66:1200–1.
Ishiwata Y, Kaneta T, Nawata S, Hino-Shishikura A, Yoshida K, Inoue T. Quantification of temporal changes in calcium score in active atherosclerotic plaque in major vessels by (18)F-sodium fluoride PET/CT. Eur J Nucl Med Mol Imaging. 2017;44:1529–37.
Creager MD, Hohl T, Hutcheson JD, Moss AJ, Schlotter F, Blaser MC, et al. (18)F-fluoride signal amplification identifies microcalcifications associated with atherosclerotic plaque instability in positron emission Tomography/Computed tomography images. Circ Cardiovasc Imaging. 2019;12:e007835.
Derlin T, Toth Z, Papp L, Wisotzki C, Apostolova I, Habermann CR, et al. Correlation of inflammation assessed by 18F-FDG PET, active mineral deposition assessed by 18F-fluoride PET, and vascular calcification in atherosclerotic plaque: A dual-tracer PET/CT study. J Nucl Med. 2011;52:1020–7.
Blomberg BA, Thomassen A, de Jong PA, Lam MGEH, Hess S, Olsen MH, et al. Reference values for fluorine-18-fluorodeoxyglucose and fluorine-18-sodium fluoride uptake in human arteries: A prospective evaluation of 89 healthy adults. Nucl Med Commun. 2017;38:998–1006.
Blomberg BA, de Jong PA, Thomassen A, Lam MGE, Vach W, Olsen MH, et al. Thoracic aorta calcification but not inflammation is associated with increased cardiovascular disease risk: Results of the CAMONA study. Eur J Nucl Med Mol Imaging. 2017;44:249–58.
Narula N, Dannenberg AJ, Olin JW, Bhatt DL, Johnson KW, Nadkarni G, et al. Pathology of peripheral artery disease in patients with critical limb ischemia. J Am Coll Cardiol. 2018;72:2152–63.
Torii S, Mustapha JA, Narula J, Mori H, Saab F, Jinnouchi H, et al. Histopathologic characterization of peripheral arteries in subjects with abundant risk factors: Correlating imaging with pathology. JACC Cardiovasc Imaging. 2018;12(8 Pt 1):1501–13.
Bartstra JW, de Jong PA, Spiering W. Accelerated peripheral vascular aging in Pseudoxanthoma elasticum - proof of concept for arterial calcification-induced cardiovascular disease. Aging (Albany NY). 2019;11:1062–4.
Niskanen L, Siitonen O, Suhonen M, Uusitupa MI. Medial artery calcification predicts cardiovascular mortality in patients with NIDDM. Diabetes Care. 1994;17:1252–6.
Fernandez-Friera L, Penalvo JL, Fernandez-Ortiz A, Ibanez B, Lopez-Melgar B, Laclaustra M, et al. Prevalence, vascular distribution, and multiterritorial extent of subclinical atherosclerosis in a middle-aged cohort: The PESA (progression of early subclinical atherosclerosis) study. Circulation. 2015;131:2104–13.
Rutten A, Isgum I, Prokop M. Coronary calcification: Effect of small variation of scan starting position on agatston, volume, and mass scores. Radiology. 2008;246:90–8.
Hoffmann U, Siebert U, Bull-Stewart A, Achenbach S, Ferencik M, Moselewski F, et al. Evidence for lower variability of coronary artery calcium mineral mass measurements by multi-detector computed tomography in a community-based cohort–consequences for progression studies. Eur J Radiol. 2006;57:396–402.
Funding
The TEMP study was supported by the Dutch Innovation Fund of Health Insurers (Innovatiefonds Zorgverzekeraars), Dutch Foundation PXE Fund, Dutch Eye Association, and Foundation Friends of University Medical Center Utrecht. The VITACAL study was supported by the Dutch Heart Foundation (2013T120)
Disclosures
Annemarie M. den Harder: none. Jelmer M. Wolterink: none. Jonas W. Bartstra: none. Wilko Spiering/Pim A. de Jong: UNI-PHARMA KLEON TSETIS PHARMACEUTICAL LABORATORIES SA (Greece) provided all etidronate and placebo capsules for free in the TEMP study, as manufacturer of the finished product (OSTOPOR® Hard capsules, 400 mg/cap). UNI-PHARMA SA was not involved in the design, the execution, the analysis, or the reporting of the TEMP trial. There were no other conflicts of interest. Sabine R. Zwakenberg: none. Joline W. Beulens: none. Riemer H.J.A. Slart: none. Gert Luurtsema: none. Willem P. Mali: none.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12350_2020_2031_MOESM1_ESM.pdf
Online Appendix 1: Plots of relationship between TBR at baseline and the calcium mass at baseline and follow-up for the TEMP study (PDF 6962 kb)
12350_2020_2031_MOESM2_ESM.pdf
Online Appendix 2: Plots of relationship between TBR at baseline and the calcium mass at baseline and follow-up for the VITACAL study (PDF 5181 kb)
12350_2020_2031_MOESM4_ESM.docx
Online Appendix 4: Results of multilevel linear regression models stratified per treatment group for both studies (DOCX 20 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
den Harder, A.M., Wolterink, J.M., Bartstra, J.W. et al. Vascular uptake on 18F-sodium fluoride positron emission tomography: precursor of vascular calcification?. J. Nucl. Cardiol. 28, 2244–2254 (2021). https://doi.org/10.1007/s12350-020-02031-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02031-5