Abstract
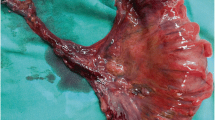
We describe a case of a mucosal prolapse syndrome (MPS)-like inflammatory polyp protruding from the appendiceal orifice, mimicking an appendiceal neoplasm. A 48-year-old man presented with lower abdominal pain and elevated white blood cell count and C-reactive protein level. Computed tomography showed a swollen appendix with multiple small saccular lesions and periappendiceal fat stranding and small saccular lesions in the ascending colon and cecum. Ultrasonography showed a swollen appendix 25 mm in diameter with multiple saccular structures and a periappendiceal high-echoic area, suggesting appendiceal diverticulitis. Colonoscopy revealed an erythematous lesion protruding from the appendiceal orifice. An ileocecal resection was performed based on a preoperative diagnosis of appendiceal diverticulitis and tumor. Histopathological examination of the appendix showed multiple mucosal herniations with infiltration of inflammatory cells, indicating appendiceal diverticulitis. The tumor was characterized by glandular duct hyperplasia and stromal expansion with smooth muscle hyperplasia and was diagnosed as an inflammatory polyp resembling an MPS lesion. Although several studies have shown the macroscopic and endoscopic appearance of MPS-like inflammatory lesions associated with colonic diverticular disease, this case was the first to present an inflammatory polyp associated with appendiceal diverticulitis in which the lesion protruding from the appendiceal orifice was masquerading as an appendiceal neoplasm.





Similar content being viewed by others
References
Kelly JK. Polypoid prolapsing mucosal folds in diverticular disease. Am J Surg Pathol. 1991;15:871–8.
Brian WA. The pathology of diverticulosis: classical concepts and mucosal changes in diverticula. J Clin Gastroent. 2006;40:126–31.
Egashira Y, Akutagawa H, Shimizu S, et al. The pathology of diverticular disease. Stomach Intestine. 2012;47:1072–82 ((In Japanese with English abstract)).
Skaane P. Benign lymphoid polyp (localized lymphoid hyperplasia) at the tip of the cecum associated with lymphoid hyperplasia of the appendix. Hepatogastroenterology. 1980;27:327–9.
Nozoe T, Mori E, Iguchi T, et al. Pedunculated hamartomatous polyp of the appendix: report of a case. Surg Today. 2013;43:191–3.
Yamagiwa Y, Terada N, Hashimoto O, et al. An inflammatory pseudotumor of the appendix. Gan No Rinsho. 1990;36:1059–62 ((in Japanese)).
Chijiiwa Y, Kabemura T, Toyota T, et al. Endoscopic appearance of the intussuscepted appendix and accurate preoperative diagnosis. Am J Gastroenterol. 1988;83:1301–3.
Birkness J, Lam-Himlin D, Byrnes K, et al. The inverted appendix - a potentially problematic diagnosis: clinicopathologic analysis of 21 cases. Histopathology. 2019;74:853–60.
Franzin G, Fratton A, Manfrini C. Polypoid lesions associated with diverticular disease of the sigmoid colon. Gastrointest Endosc. 1985;31:196–9.
Mathus-Vliegen EM, Tytgat GN. Polyp-simulating mucosal prolapse syndrome in (pre-) diverticular disease. Endoscopy. 1986;18:84–6.
Kato S, Hashiguchi K, Yamamoto R, et al. Jumbo biopsy is useful for the diagnosis of colonic prolapsing mucosal polyps with diverticulosis. World J Gastroenterol. 2006;12:1634–6.
Mori H, Tsushimi T, Kobara H, et al. Endoscopic management of a rare granulation polyp in a colonic diverticulum. World J Gastroenterol. 2013;19:9481–4.
Abdullgaffar B. Diverticulosis and diverticulitis of the appendix. Int J Surg Pathol. 2009;17:231–7.
Sugiura K, Miyake H, Nagai H, et al. Chronological changes in appendiceal pathology among patients who underwent appendectomy for suspected acute appendicitis. World J Surg. 2020;44:2965–73.
Fukata K, Takamizawa J, Miyake H, et al. Diagnosis of appendiceal diverticulitis by multidetector computed tomography. Jpn J Radiol. 2020;38:572–8.
Dupre MP, Jadavji I, Matshdes E, et al. Diverticular disease of the vermiform appendix: a diagnostic clue to underlying appendiceal neoplasm. Hum Pathol. 2008;39:1823–6.
Funding
This work is supported by Japanese Red Cross, Nagoya First Hospital Research Grant to SK (NFRCH20-0026). The funder had no role in study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Sumire Kobayashi, Kota Sugiura, Hideo Miyake, Norihiro Yuasa, Kanae Yoshikawa, and Masahiko Fujino. The first draft of the manuscript was written by Sumire Kobayashi, and all authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Sumire Kobayashi, Kota Sugiura, Hideo Miyake, Norihiro Yuasa, Kanae Yoshikawa, and Masahiko Fujino declare that they have no conflict of interest. The authors declare that they have no conflict of interest.
Human/animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5). All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from the patient included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kobayashi, S., Sugiura, K., Miyake, H. et al. Mucosal prolapse syndrome-like inflammatory polyp protruding from the appendiceal orifice masquerading as an appendiceal neoplasm: A rare case report. Clin J Gastroenterol 14, 787–790 (2021). https://doi.org/10.1007/s12328-020-01302-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-020-01302-5