Abstract
Introduction
This qualitative research study was conducted to develop a novel, comprehensive, patient-reported outcome measure (PRO), the “Symptoms and Impacts of Androgen Deprivation Therapy (ADT) for Prostate Cancer” (SIADT-PC), assessing hormonal therapy-related symptoms and their impacts on men with advanced prostate cancer.
Methods
Concept elicitation (CE) interviews were conducted among adult men with prostate cancer to evaluate their experiences with ADT. Based on key symptom and impact concepts mentioned, an initial PRO measure was developed. The draft measure was further assessed in cognitive debriefing (CD) interviews with men with prostate cancer, in which participants reviewed items, response options, and recall periods. Initial item-based psychometric analyses were conducted using interview data. The draft questionnaire was revised on the basis of participant feedback, quantitative psychometric results, and consultation with clinical experts.
Results
A total of 21 participants were interviewed (CE concept elicitation, n = 12; CD cognitive debriefing, n = 17; n = 8 completed both). Mean participant age (SD) was 59.7 (8.7) years and 76.2% were white. The de novo SIADT-PC measure consists of 27 items: 11 symptoms (e.g., fatigue, hot flashes, and erectile dysfunction), 2 long-term symptoms (e.g., weight gain), 10 impacts (e.g., impacts on physical activities and relationships), and 4 related to mode of administration (i.e., injection-site reactions). Items were assessed with a 5-point verbal rating scale, with answer choices that capture frequency or severity.
Conclusions
Once fully validated, this de novo measure may be used in clinical studies and clinical practice to assess hormone therapy-related symptoms and impacts, enabling physicians to identify timely and appropriate interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Monitoring the symptoms associated with androgen deprivation therapy (ADT) and their impacts on patients with prostate cancer is increasingly recognized as an important part of clinical practice. | |
This study reports on the development of a new patient-reported outcome measure (PRO) measure, the Symptoms and Impacts of ADT for Prostate Cancer (SIADT-PC), designed to capture the relevant symptoms of ADT and their impacts in patients with prostate cancer. | |
It is expected that this PRO measure once fully validated will help physicians recognize how ADT directly impacts patients, enabling physicians to make treatment adjustments to mitigate potential side effects, which will potentially preserve both quality and quantity of life. |
Introduction
In the USA, prostate cancer is the second-most common malignancy, accounting for 14.7% of all new cancer diagnoses in 2023 [1]. Patients with advanced prostate cancer have either high-risk localized disease, recurrent cancer after definitive treatment, or cancer that is metastatic [2, 3]. Since prostate cancer growth and progression are usually androgen-dependent, ADT with gonadotropin-releasing hormone (GnRH) receptor agonists or antagonists (including luteinizing hormone-releasing hormone [LHRH] analogues) is a staple for patients with advanced prostate cancer [4]. While effectively suppressing testosterone, and thereby prostate cancer progression, these drugs are often associated with hormonal symptoms such as hot flashes, loss of libido, and erectile dysfunction, as well as other negative impacts on patients’ daily lives [5, 6].
An assessment of these ADT-related symptoms and their impacts on patients via a validated questionnaire would enable treating physicians to implement adjunctive measures or treatment adjustments [7,8,9]. Although health-related quality of life (HRQoL) instruments are available to evaluate both the impact of the disease and its treatments, these measures may not capture all aspects of the patient experience with ADT [8, 10, 11]. A targeted literature review, conducted prior to this study (Supplemental Fig. 1), identified 26 PRO measures that included at least one question related to symptoms or impacts of ADT therapy. None comprehensively covered patient-relevant ADT-related symptoms and impacts.
The goal of this research was to develop a comprehensive, novel PRO measure, the Symptoms and Impacts of ADT for Prostate Cancer (SIADT-PC), to assess ADT-related symptoms and their impacts in men with advanced prostate cancer.
Methods
Study Design
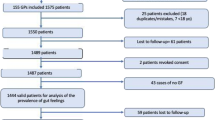
Figure 1 summarizes the study design. Following the targeted literature review, one-on-one CE patient interviews were conducted, during which participants expressed their experiences with ADT, including ADT-related symptoms and impacts on daily life, in their own words. The interview data were analyzed to identify, organize, describe, and report themes found within the dataset. This input was used to develop a draft conceptual model (CM), a graphical representation of the expected relationships between concepts [12] (i.e., ADT-related symptoms and their impacts), and to subsequently develop a draft PRO measure. One-on-one CD interviews were conducted to confirm the content validity of the draft measure; this included the appropriateness, comprehensiveness, and interpretability of content and item wording [13]. Item performance analysis was conducted on the basis of the responses to the draft PRO in the CD interviews. The PRO measure was subsequently revised on the basis of findings from the interviews, item analyses, and expert clinician input. The study methodology applied US Food and Drug Administration (FDA) Patient-Focused Drug Development guidance [14], and all research was conducted in compliance with International Conference on Harmonization Guidelines. Study exempt status was granted from the WCG Independent Review Board® (Puyallup, WA) on August 5, 2021. Participants provided written informed consent prior to enrollment.
Study Participants and Interviewers
Study participants were identified via two recruitment agencies and one large US clinical practice specializing in prostate cancer, and approached via secure email, telephone, or direct messaging through electronic medical record systems. To ensure participants had diverse demographic and clinical characteristics, a purposive sampling approach was applied. Participants were required to be adult male (aged ≥ 18 years), with a prostate cancer diagnosis, and receiving a GnRH receptor agonist (i.e., leuprolide, goserelin, triptorelin, histrelin) or antagonist (degarelix), either as monotherapy or as monotherapy for ≥ 6 months before another treatment was added (no more than 3 months prior). This was required to ensure that participants could attribute and recall symptoms specific to ADT use. See Supplemental Table 1 for detailed participant inclusion and exclusion criteria.
Sample size was determined by saturation (the point where all relevant concepts were identified); the a priori target was 10 and 15 participants for the CE and CD interviews, respectively; up to 10 participants taking a part in the CE interviews were allowed to participate in the CD interviews. Recruitment targets for the CE and CD interviews were established to ensure a diverse group in terms of age, race, educational level, comorbidities, and treatment history. Participants provided written informed consent prior to enrollment and received an honorarium after completing a CE or CD interview.
The majority of CE and CD interviews were conducted by two (of three) trained interviewers (authors KB and JC, and an additional male interviewer). All were staff researchers at Clinical Outcomes Solutions (COS; Chicago, IL), with several years of prior experience in conducting research interviews. There was no established relationship between the interviewers and participants prior to conducting the interviews; the interviewers did not report biases, assumptions, or any personal interest in the research topic. Interviews were conducted in English via telephone or videoconference software, required 60–90 min to complete, and were audio-recorded and transcribed verbatim (transcripts were not returned to participants for comment/correction). Field notes were written during the conduct of the interviews.
Qualitative Interviews
Semi-structured CE and CD interview guides were developed, pilot-tested among COS interviewers, but not with participants, to assess the flow of the guides, the length of the interviews, and the wording of questions. After pilot testing, edits were made to both interview guides.
The CE interview guide featured open-ended questions and a list of specific symptoms and impacts, identified from the literature and clinical input, to probe for if these concepts were not spontaneously mentioned. Participants were asked which symptoms and impacts were most important to them, whether they attributed the symptoms to ADT, and to indicate their preferred response options (e.g., frequency, severity) and recall periods (e.g., 7 days, 4 weeks). Attribution to ADT was not assessed for impact concepts; instead, impact concepts were categorized as proximal to ADT (i.e., resulting from or closely related to ADT symptoms) or distal to ADT (i.e., not solely attributable to ADT symptoms). CE interviews were conducted to the point of saturation [15].
CE interview data were analyzed to identify relevant concepts (symptoms and impacts) to include in the draft CM, taking into account their frequency of mention and participant-attributed importance and relationship to ADT.
The PRO items were drafted on the basis of the draft CM. Whenever possible, participants’ words, terminology, or phrasing were applied, and response options and recall periods were derived from participant preferences. For concepts with differing participant descriptions, multiple items were developed and debriefed in the CD interviews. CD interviews were conducted to confirm the content validity of the draft measure; this included the appropriateness, comprehensiveness, and interpretability of content and item wording. Specifically, participants were asked about their understanding of instructions and items, the relevance of items to their experience, and the appropriateness of recall periods and response options. For concepts with several items, participants were asked which item resonated most, and whether items measured the same or different symptoms and/or impacts. Further, participants commented on whether any symptoms or impacts were missing, and if they had suggestions for change.
Item Performance Analyses
The performance of each item in the draft PRO measure, obtained from CD interviews, was assessed in initial descriptive analyses, including ceiling and floor effects (defined as the proportion of participants who rated an item with the highest and lowest response options). A Rasch rating scale model was applied to assess the initial item parameters of the de novo measure [16, 17]. Rasch methodology applies underlying assumptions of local independence and uni-dimensionality. It also takes into consideration reliability statistics, principal components analysis, item fit, and residual correlations to ensure that PRO measure items are conditionally independent, meaning that each item is specific to a unique symptom or trait.
Data Evaluation
Participant demographic and clinical characteristics were summarized with descriptive statistics using SAS v9.4 analytic software (Cary, NC); any missing data were excluded. Analyses of transcribed interview data were conducted with NVivo 1.6.1 (QSR International, Burlington, MA). Two coders analyzed both the CE and CD interview transcripts. CE interviews were coded systematically via a thematic approach and codebook (Supplemental Table 2) that were based on the interview guide. Themes were derived from the interview transcripts. CD interview data were analyzed via a structured, deductive approach that systematically compared participant responses to determine whether the participant’s description was confirmatory of the measure’s content validity.
The final item set for the de novo PRO measure was determined in a harmonization meeting that accounted for the accumulated evidence from CE, CD, and preliminary item performance analyses. Decisions on whether to retain, delete, or change an item were based primarily on participant input, supported by clinical input from the study investigators and results from the Rasch and descriptive item quantitative analyses.
Results
Participant Characteristics
A total of 21 unique participants were interviewed; 8 completed both interviews, 4 completed only the CE interviews, and 9 completed only the CD interviews (CE sample n = 12; CD sample n = 17). No participants refused to participate or dropped out, and no interviews had to be repeated. Demographic characteristics for the overall sample are shown in Table 1. Mean participant age (SD) was 59.7 (8.7) years; 66.7% were ≤ 65 years of age, 76.2% were white, and the mean (SD) time since prostate cancer diagnosis was 21.2 (13.0) months. Approximately one-half of all participants had comorbid hypertension (52.4%), and 28.6% had diabetes. The majority (81%) had localized prostate cancer, and all participants were being treated with leuprolide as their current LHRH/GnRH receptor agonist, for a mean (SD) of 18.4 (14.4) months.
Recruitment targets were met, with the exception of non-hypertensive participants for CE (target 8, actual 6) and CD (target 12, actual 10) interviews, and age > 65 years (target 5, actual 3) and Black/African American (target 4, actual 2) for CD interviews.
Concept Elicitation and Cognitive Debriefing Results
Across the 12 CE interviews, 21 unique symptoms were identified (Table 2; see Supplemental Table 3 for key participant quotes). Most commonly reported symptoms were fatigue (n = 11), pain at the injection site (n = 10), and reduced sexual interest or desire (n = 10). When asked about the most important symptoms, participants frequently mentioned reduced sexual activity/interest (n = 6), fatigue or lack of energy (n = 5), and headache (n = 4). Among the 35 unique impacts reported (Supplemental Table 4), the most commonly mentioned were being less sexually active (n = 10); less physically active (n = 9); less socially engaged (n = 9); feeling depressed, sad, or hopeless (n = 9); anxiety, stress, or worry (n = 9); and reduced intimacy with partner (n = 9).
Supplemental Fig. 2 shows the draft CM, illustrating key ADT-related symptoms and their impacts on participants’ lives. Headaches and urinary symptoms, while reported often (n = 8 and n = 6, respectively), were generally experienced before starting ADT, and were not included in the CM. One concept, pain in the stomach or abdomen, was included in the CM based on clinician feedback, despite not being mentioned during participant interviews. This symptom could be possibly related to oral ADT, which no study participants received.
Based on the CM, the draft PRO was developed, which comprised 36 items, assessed with a 5-point verbal rating scale, with answer choices that captured frequency or severity. A total of 14 items covered seven symptom concepts, with a 7-day recall period. The two symptoms of weight gain and muscle loss were placed into a separate “long-term symptom” section, with a 4-week recall period. An additional 14 items covered six impact concepts, with a 4-week recall period. Finally, one item assessed whether participants received injectable ADT (yes/no), and an additional six items covered mode of administration (i.e., injection-site) reactions such as pain, tenderness, redness, firmness, and swelling. For these items, the recall period was “after your most recent injection.”
A total of 17 CD interviews were completed. Participant comprehension of the draft PRO measure was generally high (Supplemental Table 5: summary of CD findings per item).
Rasch Rating Scale Results
The initial review of the Rasch model (Table 3) suggested that the items included represented the hierarchy of ADT symptoms and that the measure was multidimensional; 32.4% of overall variance was explained by the model. Two items contributed to misfit: “difficulty maintaining an erection” and “intimacy impact.”
Item Harmonization and PRO Measure Development
In item harmonization meetings, which considered the CE and CD findings, and the initial item performance analyses, the final number of PRO items was reduced from 36 to 27: 11 symptom items, 10 impact items, 2 long-term symptom items, 1 injection-site item, and 3 site reaction items. Figure 2 shows the final CM, and Supplemental Table 6 the changes made to each item, along with respective rationales. The two items contributing to misfit in the Rasch model were retained as a result of participant relevance, noted in the CD interviews. The recall period for the impact items (originally 4 weeks) was changed to 7 days on the basis of clinical expert input, and in alignment with FDA guidance that patients may have difficulty accurately recalling beyond 7 days [14].
Discussion
ADT has been a treatment standard for advanced prostate cancer for many years, but can be associated with cardiovascular, cognitive, metabolic, musculoskeletal, psychological, and sexual side effects [18, 19]. Currently, there is no PRO measure to adequately assess the ADT-related symptoms and impacts of men undergoing androgen deprivation. This study describes a novel, fit-for-purpose SIADT-PC measure developed on the basis of current regulatory guidance [14] via a mixed-methods approach that comprised qualitative interviews and initial item performance analyses. CE interviews provided rich data regarding participants’ experiences of the symptoms and impacts of ADT. Subsequently, CD interviews confirmed the measure’s content validity, affirming that its instructions and items were relevant and understood as intended by participants.
Assessing HRQoL in patients with prostate cancer is increasingly recognized as an essential component of clinical practice [9]. While existing PRO instruments can measure general HRQoL changes associated with prostate cancer [10, 11], the de novo SIADT-PC provides a single instrument that focuses on and captures all patient-relevant symptoms and impacts related to hormonal-based treatment. This new measure, when fully validated, may help physicians recognize how ADT impacts patients, enabling them to intervene in treatment to mitigate side effects, potentially preserving both quality and quantity of life of patients with prostate cancer on ADT [18,19,20,21,22,23]. For example, patients with treatment-related musculoskeletal adverse effects, psychological distress, or reduced sexual activity may benefit from an exercise protocol [18, 21, 22]. Other patients experiencing ADT-related symptoms may be referred to a psychologist, nutritionist, or other specialist for adjunctive medication or diet/lifestyle education, including physical exercise, to improve bone health, erectile dysfunction, depression, hot flashes, fatigue, and/or metabolic syndrome [18, 19, 24,25,26,27,28]. Symptom assessment may also be beneficial to patients following ADT discontinuation. Multiple ADTs are currently available for the treatment of prostate cancer, and the mode of administration and half-life of these therapies vary, as do their kinetics and mechanisms of action, [29,30,31]. For example, testosterone recovery after relugolix is both more rapid and complete than with leuprolide [30, 31]. Understanding the post-treatment resolution of ADT-related symptoms and impacts could enable clinicians to more accurately identify appropriate therapeutics.
Limitations
Study limitations included the age distribution of participants, with few men aged > 65 years interviewed (men aged > 65 years have the highest prostate cancer incidence) [32]. This study population may comprise younger patients because men receiving ADT without other prostate cancer medications are younger and healthier [33]. No participants with metastatic cancer were recruited, as they were likely to be treated with combination therapies in accordance with current clinical guidelines [4]. Additionally, few Black men were interviewed. The validity of the SIADT-PC in older and African-American men, as well as those with metastatic disease, should be confirmed in future studies. In addition, the psychometric properties of the SIADT-PC measure will have to be assessed in a larger study.
Conclusions
The de novo SIADT-PC PRO measure developed in this study assesses ADT symptoms and their impacts in patients with advanced prostate cancer, with the goal of facilitating improved management. As a next step, it is expected that this measure will be included in a larger observational or clinical study to further assess its reliability, validity, sensitivity to change, and interpretability, and to confirm the factor structure and tool scoring. Once fully validated, it is anticipated that this new tool can be incorporated in real-world clinical practice and as part of clinical trial programs.
Data Availability
Anonymized transcripts of interviews generated and analyzed during the current study are available from Sumitomo Pharma Switzerland GmbH on reasonable request.
References
National Cancer Institute. Cancer stat facts: prostate cancer. https://seer.cancer.gov/statfacts/html/prost.html. Accessed March 12, 2023.
American Cancer Society. Prostate cancer early detection, diagnosis, and staging. Updated August 1, 2019. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging.html. Accessed December 30, 2022.
Swami U, McFarland TR, Nussenzveig R, Agarwal N. Advanced prostate cancer: treatment advances and future directions. Trends Cancer. 2020;6(8):702–15. https://doi.org/10.1016/j.trecan.2020.04.010.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Prostate Cancer. Version 1.2023; 2022.
Choi S, Lee AK. Efficacy and safety of gonadotropin-releasing hormone agonists used in the treatment of prostate cancer. Drug Healthc Patient Saf. 2011;3:107–19. https://doi.org/10.2147/DHPS.S24106.
Perlmutter MA, Lepor H. Androgen deprivation therapy in the treatment of advanced prostate cancer. Rev Urol. 2007;9(Suppl 1):S3-8.
Mooney K, Berry DL, Whisenant M, Sjoberg D. Improving cancer care through the patient experience: how to use patient-reported outcomes in clinical practice. Am Soc Clin Oncol Educ Book. 2017;37:695–704. https://doi.org/10.1200/EDBK_175418.
Vij A, Kowalkowski MA, Hart T, et al. Symptom management strategies for men with early-stage prostate cancer: results from the Prostate Cancer Patient Education Program (PC PEP). J Cancer Educ. 2013;28(4):755–61. https://doi.org/10.1007/s13187-013-0538-1.
Singhal U, Skolarus TA, Gore JL, et al. Implementation of patient-reported outcome measures into health care for men with localized prostate cancer. Nat Rev Urol. 2022;19(5):263–79. https://doi.org/10.1038/s41585-022-00575-4.
Chu D, Popovic M, Chow E, et al. Development, characteristics and validity of the EORTC QLQ-PR25 and the FACT-P for assessment of quality of life in prostate cancer patients. J Comp Eff Res. 2014;3(5):523–31. https://doi.org/10.2217/cer.14.41.
Gamper EM, Musoro JZ, Coens C, et al. Minimally important differences for the EORTC QLQ-C30 in prostate cancer clinical trials. BMC Cancer. 2021;21(1):1083. https://doi.org/10.1186/s12885-021-08609-7.
Ravitch SM, Carl NM. Conceptual frameworks in research. In: Qualitative Research: Bridging the Conceptual, Theoretical, and Methodological. 2nd ed. Sage. 2021.
Cheng KKF, Clark AM. Qualitative methods and patient-reported outcomes: measures development and adaptation. Int J Qual Methods. 2017;16:1–3. https://doi.org/10.1177/1609406917702983.
Food and Drug Administration. Guidance for Industry. Patient-reported outcome measures: use in medical product development to support labeling claims. https://www.fda.gov/media/77832/download. Accessed February 14, 2023.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. https://doi.org/10.1007/s11135-017-0574-8.
Petrillo J, Cano SJ, McLeod LD, Coon CD. Using classical test theory, item response theory, and Rasch measurement theory to evaluate patient-reported outcome measures: a comparison of worked examples. Value Health. 2015;18(1):25–34. https://doi.org/10.1016/j.jval.2014.10.005.
Nunnally J. Psychometric theory. 2nd ed. New York: McGraw Hill; 1978.
Donovan KA, Walker LM, Wassersug RJ, Thompson LM, Robinson JW. Psychological effects of androgen-deprivation therapy on men with prostate cancer and their partners. Cancer. 2015;121(24):4286–99. https://doi.org/10.1002/cncr.29672.
Nguyen PL, Alibhai SM, Basaria S, et al. Adverse effects of androgen deprivation therapy and strategies to mitigate them. Eur Urol. 2015;67(5):825–36. https://doi.org/10.1016/j.eururo.2014.07.010.
Efficace F, Collins GS, Cottone F, et al. Patient-reported outcomes as independent prognostic factors for survival in oncology: systematic review and meta-analysis. Value Health. 2021;24(2):250–67. https://doi.org/10.1016/j.jval.2020.10.017.
Galvao DA, Newton RU, Chambers SK, et al. Psychological distress in men with prostate cancer undertaking androgen deprivation therapy: modifying effects of exercise from a year-long randomized controlled trial. Prostate Cancer Prostatic Dis. 2021;24(3):758–66. https://doi.org/10.1038/s41391-021-00327-2.
Taaffe DR, Galvao DA, Spry N, et al. Immediate versus delayed exercise in men initiating androgen deprivation: effects on bone density and soft tissue composition. BJU Int. 2019;123(2):261–9. https://doi.org/10.1111/bju.14505.
Perera M, Roberts MJ, Klotz L, et al. Intermittent versus continuous androgen deprivation therapy for advanced prostate cancer. Nat Rev Urol. 2020;17(8):469–81. https://doi.org/10.1038/s41585-020-0335-7.
Baguley BJ, Skinner TL, Leveritt MD, Wright ORL. Nutrition therapy with high intensity interval training to improve prostate cancer-related fatigue in men on androgen deprivation therapy: a study protocol. BMC Cancer. 2017;17:1. https://doi.org/10.1186/s12885-016-3022-6.
Baguley BJ, Skinner TL, Jenkins DG, Wright ORL. Mediterranean-style dietary pattern improves cancer-related fatigue and quality of life in men with prostate cancer treated with androgen deprivation therapy: a pilot randomised control trial. Clin Nutr. 2021;40:245–54. https://doi.org/10.3390/ijerph19095709.
Baguley B, Smith-Gillis C, Porter J, Kiss N, Ugalde A. Nutrition services during prostate cancer androgen deprivation therapy. BMJ Support Palliat Care. 2023. https://doi.org/10.1136/spcare-2023-004304.
Newton RU, Jeffery E, Galvão DA, et al. Body composition, fatigue and exercise in patients with prostate cancer undergoing androgen-deprivation therapy. BJU Int. 2018;122:986–93. https://doi.org/10.1111/bju.14384.
Cormie P, Zopf EM. Exercise medicine for the management of androgen deprivation therapy-related side effects in prostate cancer. Urol Oncol. 2020;38:62–70. https://doi.org/10.1016/j.urolonc.2018.10.008.
Choi E, Buie J, Camacho J, Sharma P, de Riese WTW. Evolution of androgen deprivation therapy (ADT) and its new emerging modalities in prostate cancer: an update for practicing urologists, clinicians and medical providers. Res Rep Urol. 2022;14:87–108. https://doi.org/10.2147/RRU.S303215.
Ranjan SK. HERO trial: a rescue from injectable androgen deprivation therapy. Indian J Urol. 2021;37(2):193–4. https://doi.org/10.4103/iju.IJU_497_20.
Shore ND, George DJ, Saad F, et al. HERO phase III trial: results comparing relugolix, an oral GnRH receptor antagonist, versus leuprolide acetate for advanced prostate cancer. J Clin Oncol. 2020;38(15_suppl):5602–5602. https://doi.org/10.1200/JCO.2020.38.15_suppl.5602.
Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019;10(2):63–89. https://doi.org/10.14740/wjon1191.
Siegel DA, O'Neil ME, Richards TB, Dowling NF, Weir HK. Prostate cancer incidence and survival, by stage and race/ethnicity—USA, 2001–2017. MMWR Morb Mortal Wkly Rep. 2020;69(41):1473–1480. https://doi.org/10.15585/mmwr.mm6941a1.
Hudgens S, Dineen K, Webster K, Lai J, Cella D. Assessing statistically and clinically meaningful construct deficiency/saturation: recommended criteria for content coverage and item writing. Rasch Meas Trans. 2004;17:954–5.
Acknowledgements
The authors thank the study participants for their involvement in the study.
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial support were provided by Caitlin Rothermel and Donna Simcoe (Simcoe Consultants) and funded by Sumitomo Pharma Switzerland GmBH and Pfizer Inc. Editorial support was provided by Juscilene Menezes, a Sumitomo Pharma America Inc. employee.
Funding
This study (including the journal’s Rapid Service and Open Access fees) was funded by Sumitomo Pharma Switzerland GmbH & Pfizer, Inc.
Author information
Authors and Affiliations
Contributions
Conception and/or design of the work: Ashley Ross, Kelsie Brewer, Stacie Hudgens, Bruce Brown, Mark Fallick, Simon dePaauw-Holt, Bhakti Arondekar, Elke Hunsche. Data acquisition: Ashley Ross, Kelsie Brewer, Stacie Hudgens, Jennifer Clegg. Data analysis and/or interpretation: Ashley Ross, Kelsie Brewer, Stacie Hudgens, Bruce Brown, Mark Fallick, Simon dePaauw-Holt, Bhakti Arondekar, Jennifer Clegg, Elke Hunsche. Drafting the manuscript: Ashley Ross, Mark Fallick, Elke Hunsche. Critical review: Ashley Ross, Kelsie Brewer, Stacie Hudgens, Bruce Brown, Mark Fallick, Simon dePaauw-Holt, Bhakti Arondekar, Jennifer Clegg, Elke Hunsche. Supervision: Ashley Ross, Stacie Hudgens, Simon dePaauw-Holt, Bhakti Arondekar, Jennifer Clegg, Elke Hunsche. Note: All authors read and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
Bryan Selby (Senior VP, Product Development, was an employee of Myovant Sciences Inc, Employee, Brisbane, CA); Michael Chladek and Ruby Gogana (were employees of Clinical Outcomes Solutions, COS, Chicago, IL, US; COS was supported by Sumitomo Pharma Switzerland GmbH). Ashley E. Ross is a consultant for Veracyte Inc., Astellas Pharma Inc., Bayer, Blue Earth Inc., Janssen, Lantheus, and Tempus. Kelsie Brewer was an employee of Clinical Outcomes Solutions at the time this study was done. Stacie Hudgens is an employee of Clinical Outcomes Solutions. Bruce Brown was an employee of Myovant Sciences Inc. at the time this study was done. Mark Fallick was an employee of Myovant Sciences Inc. at the time this study was done. Simon dePaauw-Holt is an employee of Sumitomo Pharma Switzerland GmbH. Bhakti Arondekar is an employee of and owns stock in Pfizer, Inc. Jennifer Clegg is an employee of Clinical Outcomes Solutions. Elke Hunsche is an employee of Sumitomo Pharma Switzerland GmbH.
Ethical Approval
All research was conducted in compliance with International Conference on Harmonization Guidelines. Study exempt status was granted from the WCG Independent Review Board® (Puyallup, WA) on August 5, 2021. Participants provided written informed consent prior to enrollment.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ross, A., Brewer, K., Hudgens, S. et al. Development of a Novel Patient-Reported Outcome Measure to Assess Symptoms and Impacts of Androgen Deprivation Therapy for Advanced Prostate Cancer. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02888-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02888-9