Abstract
Introduction
Further insights into real-world management and outcomes of patients with pulmonary arterial hypertension (PAH) are needed. This interim analysis of the ongoing, multicentre, prospective EXPOSURE (EUPAS19085) observational study describes characteristics, treatment patterns and outcomes of patients with PAH initiating a new PAH-specific therapy in Europe/Canada.
Methods and Results
All analyses were descriptive. In total, 1944 patients with follow-up information were included; the majority were female, with World Health Organization functional class II/III symptoms and with idiopathic PAH or connective tissue disease-associated PAH. Most incident patients (N = 1100; diagnosed for ≤ 6 months) initiated treatment as monotherapy (48%) or double therapy (43%). Of those initiating monotherapy, 38% (199/530) escalated to double therapy (median [Q1, Q3] time to escalation 3.4 [1.9, 6.6] months), and of those initiating double therapy, 17% (78/457) escalated to triple therapy (median [Q1, Q3] time to escalation 7.0 [3.4, 12.7] months) during the observation period (median [Q1, Q3]: 17.0 [7.5, 29.9] months). The majority of the 834 prevalent patients (diagnosed > 6 months) entered the study on initiation of combination therapy and most did not change treatment regimen during the observation period (median [Q1, Q3]: 19.6 [10.2, 32.2] months). One-year survival was 88% for incident patients and 90% for prevalent patients.
Conclusions
Results from EXPOSURE suggest a shift towards combination therapy and the alignment of real-world treatment patterns with current guideline recommendations. While survival estimates are encouraging, the extent of monotherapy use at treatment initiation and follow-up highlight an opportunity for further improvements through optimisation of treatment strategies in line with current guidelines.
A graphical abstract is also available with this article.
Trial Registration Number
EUPAS19085.
Plain Language Summary
Pulmonary arterial hypertension (PAH) is a progressive disease. Clinical guidelines recommend that most patients start treatment with a combination of different PAH medications. While there is no cure for PAH, these medications help to control symptoms and slow disease worsening. To understand treatments currently used in clinical practice, we analysed data from EXPOSURE (EUPAS19085), an ongoing study collecting information from patients starting a new PAH medication in Europe and Canada. Most patients in the study were female, with World Health Organization functional class II/III symptoms, and idiopathic (unknown cause) PAH or PAH associated with connective tissue disorders. Among 1100 patients who were ‘recently diagnosed’ (diagnosed with PAH in the past 6 months), 88% were alive after 1 year. We found that 48% started treatment with one PAH medication, and 38% of those patients had a second medication prescribed within a median period of 3 months. Among the 457 ‘recently diagnosed’ patients treated with two PAH medications when they entered the study, 17% had a third medication prescribed within a median period of 7 months. Among 834 patients with ‘established PAH’ (diagnosed more than 6 months ago), 90% were alive after 1 year. Most entered the study when they started a third medication and did not have further changes in treatment. Our findings show that patients with PAH are often treated with one medication in clinical practice as well as a combination of medications. While survival rates are encouraging, the extent to which one PAH medication is used suggests there is room for treatment improvement.
AbstractSection Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pulmonary arterial hypertension (PAH) is a rare progressive disorder that eventually leads to death if left untreated; insights into the current real-world management and characterisation of patients with PAH are needed. |
The EXPOSURE study is an ongoing, prospective, international, observational study enrolling patients with PAH at initiation of a new PAH-specific therapy in clinical practice, with > 2500 patients enrolled to date. |
This interim analysis describes clinical characteristics, treatments patterns and outcomes of newly diagnosed (incident) patients, diagnosed within 6 months of enrolment. |
What was learned from the study? |
Overall, encouraging 1-year survival estimates were observed and the proportion of patients initiating double combination therapy at baseline suggests that treatment patterns are aligning with current guideline recommendations for PAH. |
However, many patients were still initiating monotherapy, suggesting that further improvement and optimisation of treatment of this disease in the real world are still needed. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.24476593.
Introduction
Combination therapy is placed at the core of pulmonary arterial hypertension (PAH) management, with current treatment recommendations advocating for initial oral combination therapy at diagnosis for most patients with PAH [1, 2]. At the first follow-up visit, further treatment escalation with initiation of an additional therapy is recommended for patients who do not manifest features associated with excellent long-term survival, defined as a 1-year mortality risk < 5% [1, 2].
Real-world data suggest that many patients are initiated on monotherapy [3, 4] and therefore treatment regimens do not fully align with the current recommendations [1, 2]. Additionally, recent real-world studies have shown that PAH is becoming more frequently diagnosed in older patients [3,4,5], with a more equal distribution between the sexes, and often accompanied by cardiopulmonary comorbidities, in contrast to what is typically seen in randomised controlled trials (RCTs) [1, 2, 6, 7]. Hence, further insights into the current real-world management and characterisation of patients with PAH are needed.
The EXPloratory Observational Study of Uptravi in Real-lifE (EXPOSURE) is an ongoing, prospective, international, observational study which enrols patients with PAH at initiation of a new PAH-specific therapy in clinical practice. Here, we describe clinical characteristics, treatment patterns and outcomes of newly diagnosed (incident) patients, diagnosed within 6 months of enrolment in EXPOSURE. Complementary data are provided for prevalent patients who were defined as those diagnosed for > 6 months at enrolment.
Methods
Data Sharing Statement
Although these data are not currently publicly available for sharing, requests for sharing can be sent to the Corresponding Author and will be evaluated on an individual basis.
Study Design and Patient Population
EXPOSURE (EUPAS19085) is an ongoing, multicentre, prospective, observational study of patients with PAH initiating a new PAH-specific therapy in Europe or Canada. The study started enrolling in September 2017. Patients ≥ 18 years old with Group 1 pulmonary hypertension (PAH) and initiating a new PAH-specific therapy (excluding calcium channel blockers) within 1 month of enrolment or at enrolment (i.e., at Informed Consent Form signature) were eligible. Data from patients who died < 30 days from initiation of PAH-specific therapy and were not able to provide their consent were collected in the study, where approved by local Ethics Committees. Patients newly initiating a PAH-specific therapy must not have been previously treated with that same drug. Full details of the EXPOSURE study design, patient population and data collection are provided in the Supplementary Methods.
This was an interim analysis of consecutively enrolled patients between 17 September 2017 up to 30 November 2022, with a recorded PAH-specific therapy initiation date and with follow-up information. The observation period for this analysis was defined from the date of the new PAH-specific therapy initiation until date of death, date of study discontinuation or date of last available information prior to data cut-off, whichever came first. Patients were followed and treated by their physician according to local clinical practice, with no visits/investigations mandated. Patients were stratified based on their time from PAH diagnosis: incident (diagnosed ≤ 6 months from enrolment) or prevalent (diagnosed > 6 months from enrolment).
Analyses
All analyses were descriptive, and no formal statistical comparisons were made. For all analyses, baseline was defined as the time of initiation of the new PAH-specific therapy that, per study criteria, should have occurred within a maximum time period of 1 month prior to or at study enrolment. Follow-up corresponds to any visit occurring after the initiation of the new PAH-specific therapy. Patients with year of diagnosis missing were included in the prevalent group. The three-strata risk scores were calculated using the COMPERA method [8] and four-strata risk scores were calculated according to the recommendation in the 2022 European Society of Cardiology/European Respiratory Society (ESC/ERS) Guidelines [1, 2], with further details in the Supplementary Methods.
At baseline and up to 30 days after baseline, each concomitant PAH-specific therapy that overlapped with the new PAH-specific therapy for > 1 day was considered to be taken as part of a combination therapy regimen. Treatment regimen was considered double, triple or other combination therapy if in addition to the new PAH-specific therapy one, two or more other PAH-specific therapies were received simultaneously for > 1 day, respectively. Further information on the definitions of PAH-specific therapy status and the time to treatment escalation analysis is detailed in the Supplementary Methods. Treatment patterns by therapy combination prior to baseline, at baseline and during the study observation period were described using Sankey diagrams. At 6 months and 12 months after baseline, patients who had no observation data due to study discontinuations, were lost to follow-up or had < 6 months follow-up time at data cut-off were considered as “No observation”.
Incidence rates for hospitalisation and all-cause death were calculated based on the number of patients experiencing an event after baseline, divided by the total duration of the observation period, and expressed as 100 person-years, with associated 95% confidence intervals (CI). Calculations were based on a generalised linear model assuming a Poisson distribution and using log (observation time) as an offset. Time to first event for hospitalisation and all-cause death were presented using the Kaplan-Meier (KM) method including estimates of the proportion of event-free patients during the observation period, with associated 95% CIs. Imputations were performed in the case of partially missing dates only (i.e., day or/and month missing, year present) for start/end of hospitalisation, start/discontinuation of PAH therapy, date of death, and date of PAH diagnosis. Imputation rules are further detailed in Table S1.
Monitoring and Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki, the International Society for Pharmacoepidemiology (ISPE) Guidelines for Good Pharmacoepidemiology Practices (GPP) [9] and in accordance with the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Guide on Methodological Standards in Pharmacoepidemiology [10]. The protocol was approved by the Institutional Review Board or Independent Ethics Committee at each study site (and at the national level in Sweden) (Table S2). Written informed consent was obtained from each patient for accessing and processing anonymised patient data and their use in scientific research.
Results
Patient Disposition
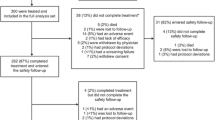
As of 30 November 2022, 2069 patients were enrolled and 1944 patients had follow-up information (Figure S1). Patients were enrolled in sites from 18 countries in Europe and in Canada (Table S3). Of these, 1110 were incident patients and 834 were prevalent patients.
Demographics and Clinical Characteristics at Baseline
Demographics and clinical characteristics at baseline are outlined in Table 1. For patients in the incident group, the median age at baseline was 65 years, 66% were female and the majority in World Health Organization functional class (WHO FC) II/III, with predominantly idiopathic PAH (IPAH) (54%) or PAH associated with connective tissue disease (PAH-CTD) (30%). The median (Q1, Q3) time since diagnosis was 0.9 (0.1, 5.1) weeks, the median 6-min walk distance (6MWD) was 320 m, and the proportion of patients with abnormal N-terminal pro-brain natriuretic peptide (NT-proBNP) (as per physician’s judgement) was 82%; 68% of patients had at least one of the following cardiovascular comorbidities: diabetes, systemic hypertension, body mass index (BMI) > 30 kg/m2 and historical evidence of reported significant coronary artery disease (Table 1 and Fig. 1). When risk of 1-year mortality was assessed using the three-strata method [8], 20%, 63% and 17% of incident patients were in the low, intermediate and high risk categories at baseline, respectively (Table 1).
History of cardiovascular risk factors in incident and prevalent patients at baseline. *Systemic-pulmonary shunts were recorded as cardiac shunts in the case report form, probably owing to their PAH-CHD aetiology. †Defined as cardiovascular comorbidities. BMI: body mass index; PAH-CHD: pulmonary arterial hypertension associated with congenital heart disease
Among prevalent patients, the median age at baseline was 61 years, 72% were female and the majority in WHO FC II/III. Most patients had IPAH (49%) or PAH-CTD (24%), and 17% had PAH associated with congenital heart disease (PAH-CHD). The median (Q1, Q3) time since diagnosis was 40.8 (18.0, 106.8) months, the median 6MWD was 370 m, and the proportion of patients with abnormal NT-proBNP was 77%. Fifty-five per cent of patients had at least one of the cardiovascular comorbidities defined above, and 11% had systemic-pulmonary shunts (Table 1 and Fig. 1). The 1-year mortality risk was assessed using the four-strata method [1, 2]; 16%, 31%, 32% and 21% of prevalent patients were in the low, intermediate-low, intermediate-high and high risk categories, respectively. (Table 1).
Treatment Patterns
At baseline, 48% of incident patients had started a new PAH-specific treatment as monotherapy (predominantly phosphodiesterase 5 inhibitor [PDE5i]), 43% started as double combination therapy (predominantly endothelin receptor antagonist [ERA] + PDE5i) and 8% started as triple combination therapy (predominantly ERA + PDE5i + selexipag) (Fig. 2A). At 6 months after baseline, 111/532 (21%) of incident patients on oral/inhaled monotherapy had escalated to oral/inhaled double combination therapy and the majority remained on this therapy up to 12 months after baseline (Fig. 3A). Most incident patients who had started a new PAH-specific treatment as part of either oral/inhaled double or oral/inhaled triple combination therapy remained on the same treatment regimen at 6 and 12 months after baseline (Fig. 3A).
Treatment patterns at baseline for A incident and B prevalent patients. Calcium channel blockers are not considered as PAH-specific therapy in EXPOSURE. Percentages may not add up to 100 because of rounding. *Includes patients with therapies that have missing start and end dates and those for whom it cannot be determined if some treatments are prior or current. ERA: endothelin receptor antagonist; PDE5i: phosphodiesterase 5 inhibitor; PGI2: prostacyclin and its analogues; sGC: soluble guanylate cyclase
Treatment patterns over time during the observation period for A incident and B prevalent patients. For monotherapy, double therapy and triple therapy, only oral/inhaled PAH-specific therapies were included in the analysis. Calcium channel blockers were not considered as PAH-specific therapy in EXPOSURE. Twenty-five patients were excluded because of missing PAH therapy start date. Some patients were receiving PAH-specific therapy prior to baseline/diagnosis because of the date of right heart catheterisation occurring after patients were enrolled. *Includes patients for whom the PAH-specific treatment combination at initiation was unknown. †Includes patients with < 6 months of observation after baseline in the study. i.v: intravenous; PAH: pulmonary arterial hypertension; s.c.: subcutaneous
Over the median (Q1, Q3) observation period of 17.0 (7.5, 29.9) months, 199/530 (38%) incident patients escalated treatment from oral/inhaled monotherapy to oral/inhaled double combination therapy, and the median (Q1, Q3) time to escalation was 3.4 (1.9, 6.6) months (Table S4). For incident patients initiated on oral/inhaled double combination therapy at baseline, 78/455 (17%) escalated to oral/inhaled triple combination therapy, with a median (Q1, Q3) time to escalation of 7.0 (3.4, 12.7) months (Table S4).
At baseline, 14% of prevalent patients started a new PAH-specific treatment as monotherapy (predominantly PDE5i or ERA), 31% as double combination therapy (predominantly ERA + PDE5i) and 49% as triple combination therapy (predominantly ERA + PDE5i + selexipag) (Fig. 2B). Prevalent patients initiating new PAH-specific therapy as oral/inhaled double combination therapy at baseline generally had escalated from oral/inhaled monotherapy, and those initiating a new PAH-specific therapy as oral/inhaled triple combination therapy generally had escalated from oral/inhaled double combination therapy (Fig. 3B). Over the 12 months prior to baseline, there was little change in treatment regimen among prevalent patients (Fig. 3B). At 6 and 12 months after baseline, the majority of prevalent patients remained on the same treatment regimen received at baseline (albeit with fewer patients with an observation at 12 months) (Fig. 3B).
Hospitalisation
Approximately one third of incident patients were hospitalised and 372/789 (47%) hospitalisations were PAH-related, with an incidence rate of 16.0 (95% CI: 13.9, 18.3) per 100 person-years, indicating that for 100 patients over a period of 1 year, 16 will have at least one PAH-related hospitalisation (Table 2). Among incident patients, 70% and 57% had not experienced a hospitalisation at 12 and 24 months, respectively (Fig. 4).
Time to first all-cause hospitalisation for incident and prevalent patients during the observation period. Kaplan-Meier curves illustrating time to first all-cause hospitalisation for incident and prevalent patients during the observation period. Kaplan-Meier estimates (95% CI) shown at 12 and 24 months. CI: confidence interval
Among prevalent patients, 37% were hospitalised and 352/600 (59%) hospitalisations were PAH-related, with an incidence rate of 15.4 (95% CI; 13.2, 17.9) per 100 person-years (Table 2). Among prevalent patients, 73% and 59% of prevalent patients had not experienced a hospitalisation at 12 and 24 months of follow-up, respectively (Fig. 4). Hospitalisation outcomes for the overall population are outlined in Table S5 and Figure S2A.
Survival
Among incident patients, the median (Q1, Q3) observation period was 17.0 (7.5, 29.9) months (Table 2). There were 207 (19%) patients who died during this time; causes were known for 144 of these and 81 (56%) were deemed to be related to PAH (Table 2). These data correspond to a mortality rate of 11.5 (95% CI: 10.0, 13.2) per 100 person-years, meaning that for 100 patients over a period of 1 year, 11.5 deaths will occur (Table 2). Among incident patients, survival was 88% and 80% at 12 and 24 months, respectively (Fig. 5).
During the observation period for prevalent patients (median [Q1, Q3]: 19.6 [10.2, 32.2] months), there were 161 (19%) prevalent patients who died and 64% of them (84/131) were PAH-related. The mortality rate was 10.8 (95% CI; 9.2, 12.6) per 100 person-years (Table 2). Survival was 90% and 79% at 12 and 24 months, respectively (Fig. 5). The main causes of death, as per physician judgement, for both incident and prevalent patients were disease progression, right heart failure and sudden death/sudden cardiac arrest (Table 2). Disease progression/PAH worsening accounted for 46 (22%) deaths for incident and 41 (25%) deaths for prevalent patients. Survival for the overall population is outlined in Table S5 and Figure S2B.
Discussion
In this analysis of EXPOSURE, we provide contemporary insights on the characteristics, treatment patterns and long-terms outcomes of incident patients with PAH initiating a new PAH-specific therapy. Complementary data are provided for prevalent patients. These prospectively collected, real-world data span 18 European countries and Canada and provide a valuable complement to existing evidence from RCTs and disease registries. The results describe the outcomes of patients with PAH in the context of current treatment practices and offer an opportunity to identify the potential for further improvements in outcomes based on current treatment recommendations (Graphical Abstract).
The characteristics of patients with PAH enrolled in EXPOSURE reflect trends in patient characteristics observed in contemporary disease registries (i.e., trends towards increasing age and presence of comorbidities) although direct comparisons between registries should be made with caution because of differences in study design, eligibility criteria and geographical variabilities in clinical practice. In EXPOSURE, the median age of incident patients (65 years) is consistent with observations in disease registries (53–65 years) [3, 4, 11,12,13,14,15,16] and comparable to the EXPOSURE prevalent population (61 years). Approximately two thirds of incident patients in EXPOSURE had at least one comorbidity, with the proportions of incident patients with obesity and diabetes (32% and 23%, respectively) similar to the COMPERA registry (33% and 27%, respectively) [3]. Such trends in changing age and comorbidities could be attributed to patients with PAH living longer through better access to therapy, or may reflect patients being diagnosed later in life, when comorbid conditions are present but somewhat controlled. These data from EXPOSURE provide insights into the real-word management of such patients who are often excluded from RCTs.
In terms of aetiology, 52% were diagnosed with IPAH, 27% with PAH-CTD and 10% with PAH-CHD. The majority of incident patients in EXPOSURE were diagnosed with IPAH (54%), similar to incident patients in the SPAHR (48%), slightly lower than those in the COMPERA (67%) and higher than those in the French (38%) registries [3,4,5]. While the proportion of patients with IPAH and PAH-CTD was similar across the incident and prevalent groups in EXPOSURE, a larger proportion of PAH-CHD patients, generally associated with a better prognosis [17, 18], was in the prevalent group compared to the incident group. PAH-CHD patients accounted for 5% of patients in the EXPOSURE incident group, compared with 3% in COMPERA [3], 10% in the SPAHR [5], 16% in the REHAP (Spain) [19] and approximately one third of patients in the Polish, Latvian and UK registries [11, 13, 14]. Heritable patients with PAH accounted for 3% of patients in both the incident and prevalent groups; this is slightly lower than that seen in the French registry (5%) [4] but in line with observations in the Polish, REVEAL and PHAR registries (1–3%) [13, 15, 16].
As this was a predominantly European-based study, the 2022 ESC/ERS three and four strata recommended methods for risk assessment [1, 2] were used. Similar to contemporary disease registries [8, 20] using the three-strata risk assessment method (as recommended for incident patients in the current ESC/ERS guidelines) [1, 2], the majority of incident patients in EXPOSURE were in the intermediate risk group. Using the four-strata method [1, 2], at baseline 7%, 23%, 34% and 36% of incident patients were at low, intermediate-low, intermediate-high and high risk of death at 1-year, respectively. These data reflect a trend towards higher risk when compared with contemporary disease registries: 6%, 24%, 55% and 15% in COMPERA, respectively [21], and 12%, 33%, 40% and 15% in the French registry, respectively [4]. Overall, the baseline clinical characteristics of patients in the incident and prevalent groups were similar in EXPOSURE. In particular for prevalent patients, we hypothesise that with current treatment practices, initiation of a new PAH-specific therapy may be in response to evidence of disease progression and may therefore introduce a bias towards higher risk in the prevalent population here compared to the wider prevalent PAH population.
Almost half of incident patients in EXPOSURE were on combination therapy; the proportion was greater than that of disease registries, in which 16–31% were initiated on combination therapy at, or within 3 months of, diagnosis [3, 4, 22]. However, despite current recommendations for combination therapy at treatment initiation [1, 2, 23, 24], the remaining half of newly diagnosed patients in EXPOSURE were treated with monotherapy at baseline, while in other registries between 60 and 80% of patients were either initiated on monotherapy or did not receive PAH-specific therapy at diagnosis [3,4,5]. While certain clinical circumstances warrant monotherapy use, on balance these data suggest that patients may not have been optimally managed in terms of initial treatment strategy, particularly when considering that approximately 70% of patients in EXPOSURE were considered at intermediate-high or high risk of death at 1-year. These results highlight an opportunity for more proactive management of PAH through use of combination therapy at the time of diagnosis. An encouraging finding from EXPOSURE is that more than one third of the patients in the incident cohort who initiated on monotherapy were escalated to double combination therapy within 4 months.
Most prevalent patients enrolled into EXPOSURE upon initiation of either double oral/inhaled combination therapy (predominantly PDE5i + ERA) or triple oral/inhaled combination therapy (predominantly PDE5i, ERA + selexipag), and minimal changes in treatment patterns were observed 6 and 12 months after baseline, with the caveat of fewer observations at 12 months. The limited changes are perhaps to be expected among prevalent patients diagnosed for > 3 years and already receiving combination therapy, thereby having less scope for treatment escalation.
The 1-year survival estimate observed here for incident patients (88%) is similar to that seen for incident patients in disease registries (86%–95%) [3,4,5, 11, 12, 14, 19]. In the past decade, analyses from national registries [15, 25] have shown that populations of incident patients tend to have worse survival than prevalent patients, which could reflect a survival bias among the prevalent patients [26]. Despite the survival bias effect, the survival rates in EXPOSURE were similar between the incident and prevalent groups. The study eligibility criteria required initiation of a new PAH-specific therapy, which might have favoured enrolment of patients with more severe disease, leading to a selection bias. Therefore, the prevalent patients in EXPOSURE may not be representative of prevalent patients with satisfactory disease progress.
Evidence on hospitalisations of patients with PAH in European registries is lacking. Results from claims and hospital discharge databases have respectively shown hospitalisation rates of 80–84% (all-cause) and 71–73% (PAH related) in the UK from 2013 to 2017 [27] and of 47–62% (all-cause) in France from 2012 to 2016 [28]. In our study, the proportion of the overall population hospitalised during the 17.9-month observation period was 36% (all-cause), with 52% of those being deemed related to PAH. However, direct comparisons between EXPOSURE and claims-based data are not possible because of inherent differences in methodology between a clinical and a claim database. As real-world data on hospitalisations in patients with PAH are currently lacking, data from EXPOSURE provide important, real-world insights for patients initiating a new PAH-specific therapy in Europe and Canada.
This interim analysis of EXPOSURE is subject to limitations. Per study design, only patients initiating a new PAH-specific therapy were included. This may have introduced a selection bias towards patients initiating more intensive treatment; therefore, prevalent patients may not be fully representative of those in the wider PAH population. This study provides broad representation of patients with PAH from across Europe and Canada where selexipag is available; however, the generalisability to wider geographical regions is not known.
Conclusions
These real-world data from EXPOSURE provide important insights into the characteristics, treatment patterns and outcomes of patients with PAH initiating a new PAH-specific therapy in Europe and Canada. Treatment patterns are aligning with current guideline recommendations, with the adoption of initial double combination therapy at baseline. The 1-year survival estimates of 89% are encouraging and similar to those observed in European disease registries. However, the high proportion of incident patients initiated on monotherapy and the 21% of prevalent patients at high risk of 1-year mortality at enrolment suggest that further improvement and optimisation of treatment of this disease in the real world are still needed.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43:3618–731. https://doi.org/10.1093/eurheartj/ehac237.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2023;61:2200879. https://doi.org/10.1183/13993003.00879-2022.
Hoeper MM, Pausch C, Grünig E, Staehler G, Huscher D, Pittrow D, et al. Temporal trends in pulmonary arterial hypertension: results from the COMPERA registry. Eur Respir J. 2022;59:2102024. https://doi.org/10.1183/13993003.02024-2021.
Boucly A, Weatherald J, Savale L, de Groote P, Cottin V, Prévot G, et al. External validation of a refined four-stratum risk assessment score from the French pulmonary hypertension registry. Eur Respir J. 2022;59:2102419. https://doi.org/10.1183/13993003.02419-2021.
Swedish Pulmonary arterial hypertension registry (SPAHR). Annual Report 2022. https://www.ucr.uu.se/spahr/arsrapporter/arsrapport-spahr-2022/viewdocument/163. Accessed Mar 2023.
McLaughlin VV, Channick R, Kim NH, Frantz RP, McConnell J, Melendres-Groves L, et al. Safety of macitentan for the treatment of pulmonary hypertension: real-world experience from the OPsumit® USers Registry (OPUS) and OPsumit® Historical USers cohort (OrPHeUS). Pulm Circ. 2022;12: e12150. https://doi.org/10.1002/pul2.12150.
Hoeper MM, Pausch C, Grünig E, Klose H, Staehler G, Huscher D, et al. Idiopathic pulmonary arterial hypertension phenotypes determined by cluster analysis from the COMPERA registry. J Heart Lung Transplant. 2020;39:1435–44. https://doi.org/10.1016/j.healun.2020.09.011.
Hoeper MM, Kramer T, Pan Z, Eichstaedt CA, Spiesshoefer J, Benjamin N, et al. Mortality in pulmonary arterial hypertension: prediction by the 2015 European pulmonary hypertension guidelines risk stratification model. Eur Respir J. 2017;50:1700740. https://doi.org/10.1183/13993003.00740-2017.
International Society for Pharmacoepidemiology. Guidelines for good pharmacoepidemiology practices (GPP). Pharmacoepidemiol Drug Saf. 2008;17:200–8. https://doi.org/10.1002/pds.3891.
The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance. Guide on Methodological Standards in Pharmacoepidemiology (Revision 10). EMA/95098/2010.
Skride A, Sablinskis K, Lejnieks A, Rudzitis A, Lang I. Characteristics and survival data from Latvian pulmonary hypertension registry: comparison of prospective pulmonary hypertension registries in Europe. Pulm Circ. 2018;8:1–9. https://doi.org/10.1177/2045894018780521.
Appenzeller P, Lichtblau M, Berlier C, Aubert J-D, Azzola A, Fellrath J-M, et al. Disease characteristics and clinical outcome over two decades from the Swiss pulmonary hypertension registry. Pulm Circ. 2022;12: e12001. https://doi.org/10.1002/pul2.12001.
Kopeć G, Kurzyna M, Mroczek E, Chrzanowski Ł, Mularek-Kubzdela T, Skoczylas I, et al. Characterization of Patients with Pulmonary Arterial Hypertension: data from the Polish Registry of Pulmonary Hypertension (BNP-PL). J Clin Med. 2020;9:173. https://doi.org/10.3390/jcm9010173.
NHS Digital. National Audit of Pulmonary Hypertension. 13th Annual Report. https://files.digital.nhs.uk/36/B8B717/NAPH%2013AR%20-%20Main%20Report%20v1.0.pdf. Accessed Jul 2023.
Farber HW, Miller DP, Poms AD, Badesch DB, Frost AE, Muros-Le Rouzic E, et al. Five-year outcomes of patients enrolled in the REVEAL Registry. Chest. 2015;148:1043–54. https://doi.org/10.1378/chest.15-0300.
Chang KY, Duval S, Badesch DB, Bull TM, Chakinala MM, de Marco T, et al. Mortality in pulmonary arterial hypertension in the modern era: early insights from the pulmonary hypertension association registry. J Am Heart Assoc. 2022;11: e024969. https://doi.org/10.1161/JAHA.121.024969.
Kaemmerer H, Gorenflo M, Huscher D, Pittrow D, Apitz C, Baumgartner H, et al. Pulmonary hypertension in adults with congenital heart disease: real-world data from the International COMPERA-CHD Registry. J Clin Med. 2020;9:1456. https://doi.org/10.3390/jcm9051456.
Alonso-Gonzalez R, Lopez-Guarch CJ, Subirana-Domenech MT, Ruiz JM, Gonzalez IO, Cubero JS, et al. Pulmonary hypertension and congenital heart disease: an insight from the REHAP National Registry. Int J Cardiol. 2015;184:717–23. https://doi.org/10.1016/j.ijcard.2015.02.031.
Escribano-Subias P, Blanco I, Lopez-Meseguer M, Lopez-Guarch CJ, Roman A, Morales P, et al. Survival in pulmonary hypertension in Spain: insights from the Spanish registry. Eur Respir J. 2012;40:596–603. https://doi.org/10.1183/09031936.00101211.
Kylhammar D, Kjellstrom B, Hjalmarsson C, Jansson K, Nisell M, Soderberg S, et al. A comprehensive risk stratification at early follow-up determines prognosis in pulmonary arterial hypertension. Eur Heart J. 2017;39:4175–81. https://doi.org/10.1093/eurheartj/ehx257.
Hoeper MM, Pausch C, Olsson KM, Huscher D, Pittrow D, Grünig E, et al. COMPERA 2.0: a refined 4-strata risk assessment model for pulmonary arterial hypertension. Eur Respir J. 2022;60:2102311. https://doi.org/10.1183/13993003.02311-2021.
Rådegran G, Kjellström B, Ekmehag B, Larsen F, Rundqvist B, Blomquist SB, et al. Characteristics and survival of adult Swedish PAH and CTEPH patients 2000–2014. Scand Cardiovasc J. 2016;50:243–50. https://doi.org/10.1080/14017431.2016.1185532.
Galiè N, Humbert M, Vachiéry JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37:67–119. https://doi.org/10.1093/eurheartj/ehv317.
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J. 2015;46:903–75. https://doi.org/10.1183/13993003.01032-2015.
Humbert M, Sitbon O, Yaïci A, Montani D, O’Callaghan DS, Jais X, et al. Survival in incident and prevalent cohorts of patients with pulmonary arterial hypertension. Eur Respir J. 2010;36:549–55. https://doi.org/10.1183/09031936.00057010.
Miller DP, Gomberg-Maitland M, Humbert M. Survivor bias and risk assessment. Eur Respir J. 2012;40:530–2. https://doi.org/10.1183/09031936.00094112.
Exposto F, Hermans R, Nordgren Å, Taylor L, Sikander Rehman S, Ogley R, et al. Burden of pulmonary arterial hypertension in England: retrospective HES database analysis. Ther Adv Respir Dis. 2021;15:1753466621995040. https://doi.org/10.1177/1753466621995040.
Exposto F, Petrică N, Davies E, Beaudet A. Identification of a pulmonary arterial hypertension (PAH) patient cohort and study of its burden of illness in Programme de Médicalisation des Systèmes d’information (PMSI). Int J Cardiol. 2020;306:175–80. https://doi.org/10.1016/j.ijcard.2020.02.034.
Acknowledgements
We thank the participants of this study.
Medical Writing, Editorial and Other Assistance.
Medical writing support was provided by Emma Connolly and Laura Corbett of eluSCIdate Ltd (Meggen, Switzerland). For the plain language summary and graphical abstract, medical writing support was provided by Shaun Hall and Lisa Berridge of Ashfield MedComms, an Inizio Company (Macclesfield, UK). Medical writing support was funded by Actelion Pharmaceuticals Ltd, a Janssen Pharmaceutical Company of Johnson & Johnson.
Funding
This study, the journal’s Rapid Service and Open Access fee were funded by Actelion Pharmaceuticals Ltd, a Janssen Pharmaceutical Company of Johnson & Johnson.
Author information
Authors and Affiliations
Contributions
Audrey Muller contributed to the conceptualisation, data curation, formal analysis, methodology, writing–original draft and writing–reviewing and editing of the manuscript. Pilar Escribano-Subias, Catarina C Fernandes, Tobias J Lange, Stefan Söderberg, and Sean Gaine contributed to the conceptualisation, writing–original draft and writing–reviewing and editing. Martina Fontana contributed to the data curation, formal analysis, validation, writing–original draft and writing–reviewing and editing.
Corresponding author
Ethics declarations
Conflict of Interest
Audrey Muller is an employee of Janssen Pharmaceutical Companies of Johnson & Johnson and has Johnson & Johnson shares. Pilar Escribano-Subias has received payment or honoraria for lectures, presentations, speaker’s bureaus, manuscript writing or educational events from Janssen Pharmaceutical Companies of Johnson & Johnson, MSD, Ferrer and AOT, has received support from Janssen Pharmaceutical Companies of Johnson & Johnson and MSD for attending meetings and/or travel and has participated on a Data Safety Monitoring Board or Advisory Board for Janssen Pharmaceutical Companies of Johnson & Johnson, MSD, Ferrer, Gossamer and AOT. Catarina C Fernandes is an employee of Janssen Pharmaceutical Companies of Johnson & Johnson. Martina Fontana is an employee of Janssen Pharmaceutical Companies of Johnson & Johnson. Tobias J Lange has received speaker fees and/or consultancy fees and/or financial and non-financial support for participation in scientific events from Acceleron Pharma, AstraZeneca, Bayer, Böhringer Ingelheim, Ferrer, Gossamer Bio, Janssen Pharmaceutical Companies of Johnson & Johnson, MSD, Orphacare and Pfizer. Stefan Söderberg has received speaker and consultancy fees, and financial support for participation in scientific events from Janssen Pharmaceutical Companies of Johnson & Johnson. Sean Gaine has had relations, such as funding, with the following subjects that have commercial interests in the pharmaceutical and medical field: Aerovate Therapeutics, Acceleron, Altavant, Bayer, Gossamer Bio, Janssen Pharmaceutical Companies of Johnson & Johnson, MSD and United Therapeutics.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki, the International Society for Pharmacoepidemiology (ISPE) Guidelines for Good Pharmacoepidemiology Practices (GPP) and in accordance with the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Guide on Methodological Standards in Pharmacoepidemiology. The protocol was approved by the Institutional Review Board or Independent Ethics Committee at each study site (and at the national level in Sweden). Written informed consent was obtained from each patient for accessing and processing anonymised patient data and their use in scientific research.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Muller, A., Escribano-Subias, P., Fernandes, C.C. et al. Real-World Management of Patients with Pulmonary Arterial Hypertension: Insights from EXPOSURE. Adv Ther 41, 1103–1119 (2024). https://doi.org/10.1007/s12325-023-02730-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02730-8