Abstract
Introduction
Patients with triple-class-exposed relapsed/refractory multiple myeloma (TCE-RRMM) have a poor prognosis and limited treatment options. Teclistamab, a B-cell maturation antigen × CD3 bispecific antibody, was studied in patients with TCE-RRMM in the single-arm MajesTEC-1 study. To assess the relative effectiveness of teclistamab versus real-world physician’s choice of therapy (RWPC), adjusted comparisons were performed using individual patient data from MajesTEC-1 and LocoMMotion, a prospective study of patients with TCE-RRMM.
Methods
An external control arm for MajesTEC-1 was created from patients in LocoMMotion (n = 248; clinical cut-off: November 2, 2021) and compared with treated patients (n = 165) from MajesTEC-1 (teclistamab 1.5 mg/kg weekly; clinical cut-off: March 16, 2022). Inverse probability weighting was used to adjust for imbalances in baseline covariates. For binary endpoints [overall response rate (ORR), very good partial response or better (≥ VGPR) rate, complete response or better (≥ CR)], relative effect of teclistamab versus RWPC was estimated with an odds ratio and relative response rate and 95% confidence interval (CI), derived from weighted logistic regression. Weighted Cox proportional hazards model was used to estimate hazard ratios (HR) and 95% CIs for time-to-event endpoints [duration of response (DOR), progression-free survival (PFS), and overall survival (OS)].
Results
After weighting, baseline characteristics were balanced across cohorts. In adjusted comparisons, teclistamab-treated patients were 2.3-fold, 5.2-fold and 148.3-fold, more likely to reach ORR [response-rate ratio (RR) = 2.31, 95% CI 1.77–2.85, p < 0.0001], ≥ VGPR (RR = 5.19, 95% CI 3.26–7.12, p < 0.0001) and ≥ CR (RR = 148.25, 95% CI 20.63–1065.40, p < 0.0001), respectively, versus patients receiving RWPC. Following adjustment, DOR (HR 0.32, 95% CI 0.19–0.54, p < 0.0001) and PFS (HR 0.48, 95% CI 0.35–0.65, p < 0.0001) were significantly longer with teclistamab versus RWPC. OS was numerically better with teclistamab versus RWPC [HR 0.77 (0.55–1.09), p = 0.1419].
Conclusion
Teclistamab demonstrated improved effectiveness versus RWPC, highlighting its clinical benefit as a novel and effective treatment for patients with TCE-RRMM.
Trial Registration
Majest TEC-1, ClinicalTrials.gov NCT04557098; LocoMMotion, ClinicalTrials.gov NCT04035226.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with relapsed/refractory multiple myeloma (RRMM) have a limited life expectancy, and new, more efficacious treatment options are needed to halt disease progression, extend survival, and improve quality of life. |
The ongoing single-arm MajesTEC-1 (NCT04557098) study is investigating the efficacy and safety of teclistamab, a novel B-cell maturation antigen × CD3 bispecific antibody, in patients with RRMM who are triple-class exposed (TCE; previously received treatment with an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody). |
The objective of this study was to compare outcomes in patients with TCE-RRMM treated with teclistamab in MajesTEC-1 versus patients treated with real-world physician’s choice of therapy from the LocoMMotion study. |
What was learned from the study? |
Patients treated with teclistamab in MajesTEC-1 had most outcomes significantly improved compared with a matched patient cohort treated with real-world physician’s choice of therapy. |
These results indicate that teclistamab provides a highly effective treatment option in this population, filling an important unmet need. |
Introduction
Survival in patients with multiple myeloma (MM) has improved significantly in the last 10 years, with advances in treatment such as immunomodulatory agents (IMiDs), proteasome inhibitors (PIs), and monoclonal antibodies [1,2,3,4,5,6]. However, MM remains incurable, and most patients relapse, requiring multiple rounds of treatment [7,8,9]. Patients with MM who have received IMiDs, PIs, and anti-CD38 monoclonal antibodies [i.e., triple-class exposed (TCE)] have a poor prognosis and limited treatment options, with a low likelihood of response to subsequent therapy [10]. Therefore, there is an urgent requirement for new, more efficacious therapy options to delay progression, prolong survival, and improve quality of life in these patients [10,11,12].
Teclistamab is an off-the-shelf, T-cell-redirecting, B-cell maturation antigen (BCMA) × CD3 bispecific antibody that mediates T-cell activation and subsequent lysis of BCMA-expressing myeloma cells [13, 14]. The safety and efficacy of teclistamab has been investigated in MajesTEC-1, a single-arm, open-label, multicohort, phase 1/2 study in patients with triple-class exposed relapsed/refractory MM (TCE-RRMM) who previously received ≥ 3 lines of therapy (LOTs). Initial results from the cohort with no previous exposure to anti-BCMA therapy demonstrated that weekly teclistamab at the recommended phase 2 dose of 1.5 mg/kg was well tolerated, with an overall response rate of 63% [15]. In the absence of a control arm in MajesTEC-1, indirect adjusted treatment comparisons can be performed to assess the benefits of treatment relative to regimens used in clinical practice [16]. LocoMMotion was the first prospective study of real-world physician’s choice of therapy (RWPC) in patients with TCE-RRMM [17], which created an external real-world control arm for comparison with MajesTEC-1. In the study reported here, individual patient data (IPD) from MajesTEC-1 and LocoMMotion were analyzed to assess the comparative effectiveness of teclistamab versus currently available RWPC in patients with TCE-RRMM.
Methods
Patient Populations
Detailed descriptions regarding data sources, study designs, outcomes, and analysis methods are presented in the Supplementary Materials Appendix S1. IPD from MajesTEC-1 (NCT04557098) and LocoMMotion (NCT04035226) were used to conduct adjusted comparisons between teclistamab and RWPC. IPD from MajesTEC-1 were included from all patients treated with teclistamab 1.5 mg/kg weekly (n = 165; clinical cut-off of March 16, 2022) and compared with data from patients in LocoMMotion (n = 248 enrolled between August 2019 and October 2020; clinical cut-off of November 2, 2021). The index date for both MajesTEC-1 and LocoMMotion was the date of treatment initiation.
For both MajesTEC-1 and LocoMMotion, all patients provided written informed consent, and an independent ethics committee or institutional review board at each study center approved the study protocol (Supplementary Material Tables S1 and S2). MajesTEC-1 was conducted in accordance with the Declaration of Helsinki and International Conference on Harmonisation Guidelines for Good Clinical Practice. The LocoMMotion study was conducted in accordance with the Declaration of Helsinki.
Efficacy Endpoints
Overall response rate (ORR), very good partial response or better (≥ VGPR), complete response or better (≥ CR), duration of response (DOR), progression-free survival (PFS), and overall survival (OS) were compared between teclistamab and RWPC.
Statistical Analyses
The inverse probability of treatment weighting (IPTW) method, using the average treatment effect in the treated (ATT) approach [18], was implemented to balance the RWPC population to the teclistamab cohort, on prognostic baseline characteristics available in both cohorts. The prognostic baseline characteristics to be adjusted for in the statistical analyses were based upon consultations with clinical experts, and included refractory status, International Staging System (ISS) stage, time to progression on previous LOT, extramedullary disease, number of previous LOTs, years since MM diagnosis, average duration of previous LOTs, age, hemoglobin levels, lactate dehydrogenase levels, creatinine clearance, Eastern Cooperative Oncology Group performance status, sex, type of MM, and previous hematopoietic stem cell transplant. Due to a high rate of missingness, cytogenetic risk was not included in the adjusted analyses. In addition, race was also not included in adjusted analyses, as inclusion induced unstable estimates and increased imbalance for other factors. This was caused by the high weights assigned to the small number of non-White patients enrolled in LocoMMotion, in order to balance with the higher proportion of non-White patients in MajesTEC-1. However, sensitivity analyses were run, including these two variables in the ATT-adjustment.
The ATT approach involved two steps. First, propensity scores, estimated using multivariable logistic regression including all baseline factors, were transformed into ATT weights assigned to the RWPC cohort in such a way that baseline factors of the reweighted RWPC cohort became similar to the teclistamab population. The degree of imbalance between groups was assessed using standardized mean differences (SMDs), with values > 0.2 considered to reflect important differences. In a second step, weighted logistic regression was used for response outcomes to estimate odds ratios (OR) with 95% confidence intervals (CIs), converted to response rate ratios (RR) [19]. Weighted Cox proportional hazards regression was used to estimate hazard ratios (HR) with corresponding 95% CIs for time-to-event endpoints. When results indicate the relative treatment effect changed over time, time-dependent HRs were estimated.
Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and R versions 3.6.1 and 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics
The median follow-up was 14.1 months in MajesTEC-1 (data cut-off: March 16, 2022) and 16.13 months in LocoMMotion (data cut-off: November 2, 2021). Baseline characteristics for the MajesTEC-1 and LocoMMotion study populations before and after weighting are shown in Table 1. Before reweighting, substantial (SMD > 0.2) differences were observed for many of the base case variables, with the MajesTEC-1 population having a higher proportion of participants with ISS stage I disease, with immunoglobulin G subtype, who were < 65 years of age, who were penta-drug refractory, who had a previous hematopoietic stem cell transplant, and who had creatinine clearance between 60 and 90 mL/min. In contrast to MajesTEC-1, the RWPC cohort had a greater proportion of participants with ISS stage III disease, who were triple refractory, and who had creatinine clearance < 60 mL/min. After reweighting of the RWPC cohort, baseline characteristics were well balanced between the two cohorts, with all SMD values below 0.10, except for refractory status (SMD = 0.14) (Supplementary Material Fig. S1).
Treatment Regimens Received in Real-World Clinical Practice
Approximately 90 unique regimens were used in LocoMMotion, including PIs, IMiDs, anti-CD38 monoclonal antibodies, alkylating agents, corticosteroids, and combinations thereof (Supplementary Material Table S3). Patients received a median of 4.0 (range, 1–25) cycles of therapy, and 162 (65.3%) patients were treated with a combination of ≥ 3 drugs. The most frequently used PIs, IMiDs, and anti-CD38 monoclonal antibodies were carfilzomib (25.4%), pomalidomide (29.8%), and daratumumab (9.3%), respectively. Only a limited number of patients were initiated at baseline with belantamab mafodotin (n = 6) or selinexor (n = 2), as these agents only became available during the LocoMMotion recruitment period. Idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel) were not approved at end of enrollment in LocoMMotion. At the time of data cut-off, 139 patients received subsequent anti-myeloma therapy, of whom 64 (46.0%) received at least one novel agent, mainly belantamab (n = 42) and selinexor (n = 20), but also bispecific antibodies (n = 10) and CAR-T (n = 1) (both as part of a clinical trial).
Comparative Analysis of Efficacy Outcomes
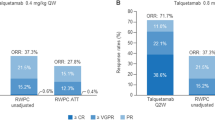
Figure 1 and Table 2 summarize the observed response rates and adjusted treatment comparisons for teclistamab versus RWPC. After IPTW-ATT adjustment, ORR [RR = 2.31, (95% CI 1.77–2.85)], ≥ VGPR [RR = 5.19 (3.26–7.12)] and ≥ CR [RR = 148.25 (20.63–1065.4)] were significantly higher with teclistamab than RWPC (all p < 0.0001). ATT adjusted DOR [HR 0.32 (0.19–0.54), p < 0.0001] was significantly longer for teclistamab (median = 18.43 months) versus RWPC (adjusted median = 5.78 months). Similarly, PFS [HR 0.48 (0.35–0.65), p < 0.0001] was significantly longer for teclistamab (median = 11.30 months) versus RWPC (adjusted median = 4.14 months) (Fig. 2, Table 3). OS was numerically better [HR 0.77 (0.55–1.09), p = 0.142] in MajesTEC-1 (median = 18.27 months) compared to the RWPC cohort (adjusted median = 13.54 months). Figure 2a, b suggests that the relative effect for both PFS and OS for teclistamab increased beyond 3 months when patients start to reach responses, with PFS HR of 0.30 (0.20–0.46, p < 0.001), and HR for OS of 0.60 (95% CI 0.40–0.90, p = 0.014) in patients who were progression free and alive at 3 months. This is also related to the long duration of response in the subgroup of responders.
Discussion
Despite recent advances, outcomes for many patients with TCE-RRMM remain poor, and there is an urgent need for novel therapies in this population. Teclistamab, an off-the-shelf, BCMA × CD3 bispecific antibody, has demonstrated deep and durable clinical responses and a predictable safety profile in MajesTEC-1 in patients with heavily pre-treated RRMM. MajesTEC-1 was performed as a single-arm study, because a randomized controlled trial was not feasible as there was no established standard of care and a lack of clinical equipoise. When direct comparisons are not feasible, indirect treatment comparisons can be performed between different treatment regimens using statistical methods that control for baseline differences in patient characteristics between populations [20]. The adjusted comparisons presented here represent high-quality evidence to inform the comparative effectiveness of teclistamab relative to RWPC.
Data for RWPC were obtained from LocoMMotion, which includes patients from nine European countries and the United States and is therefore representative of RWPC across different settings. A key advantage of LocoMMotion was the availability of a wide range of clinically relevant baseline risk factors and outcomes consistent with those captured in MajesTEC-1, which allowed generation of robust comparative analyses on all relevant endpoints, including response and survival outcomes, with proper adjustment for confounding bias due to imbalance in prognostic baseline characteristics.
Our analyses demonstrated clinically and statistically significant advantages in response and survival outcomes with teclistamab over RWPC in patients with triple-class-exposed RRMM who received ≥ 3 previous LOTs. Patients treated with teclistamab were 2.3-fold, 5.2-fold, and 148.3-fold more likely to achieve a response (ORR), ≥ VGPR, and ≥ CR, respectively, versus RWPC. The superior depth of response is demonstrated by the fact that, within the responding teclistamab patients, nearly all reached ≥ VGPR (94%) and the majority (63%) reached ≥ CR, while the majority (58%) of the RWPC responders only reached PR as best response, and only 1.5% reached ≥ CR. The significantly higher rate of ≥ CR with teclistamab is particularly important, given that ≥ CR rate is a common measure of depth of response and associated with prolonged remission [21]. This is also related to the substantially longer DOR for teclistamab, with a 68% reduction in the risk of progression or death since onset of response compared to the responders in the RWPC-cohort. Patients on teclistamab also had significantly better PFS and numerically better OS compared with RWPC. Additionally, the benefit of teclistamab in improving PFS and OS was observed beyond 3 months of treatment initiation (Fig. 2). The main findings were consistent with those from sensitivity analyses conducted to assess the effect of varying the statistical methods and covariates used.
There are some limitations to our study. As in any non-randomized study, residual confounding cannot be excluded. However, the prospective nature of the LocoMMotion study allowed all patient characteristics as captured in MajesTEC-1 to be collected at baseline, which enabled data analyses to adjust for clinically important prognostic factors. The list of clinically important prognostic factors to be adjusted for was identified a priori based on a review of the literature and consultations with clinical experts, and was further validated by the prognostic strength of these factors in the MajesTEC-1 and RWPC cohorts. Clinical experts were consulted at multiple stages of the analysis to ensure clinical validity of the chosen covariates. Imbalances between cohorts on all these risk factors were minimal after ATT-weighting, strengthening the validity of the adjusted comparisons. Cytogenetic risk was not included in the reported analyses, due to high missingness, which reflects that this is not routinely captured in real-world practice. Also, race was not included, due to low numbers for non-White RWPC patients. However, sensitivity analyses (not reported here) additionally including both factors did not show any major impact on the comparative results.
A further limitation is that there were no restrictions on treatment types used in LocoMMotion, thereby allowing physicians to prescribe based on clinical judgement. Although comparison of teclistamab to individual therapies was not possible due to the highly varied and individualized therapies selected by physicians for their patients, the comparator group was representative of regimens that are widely available to clinicians for use in clinical practice.
Another limitation was the limited availability of newer treatments in the RWCP cohort. Although new therapies for treatment of patients with TCE-RRMM have recently emerged, including selinexor, belantamab mafodotin, ide-cel, and cilta-cel, their use has been largely limited to participants in clinical trials [22,23,24,25]. During recruitment for LocoMMotion, selinexor was only available in the United States, and belantamab mafodotin was approved in the United States and the European Union for 3 months during the LocoMMotion recruitment period, so both agents were received by only a few patients in the study in the treatment line initiated at baseline. No patients initiated CAR-T treatment (ide-cel or cilta-cel), as these were not approved at time of enrollment in LocoMMotion. However, of all the RWPC patients who received subsequent treatment after the treatment line initiated at baseline, 46% were treated with at least one novel agent, indicating that OS observed for RWPC may reflect the benefit of other novel agents.
Conclusions
The comparison of MajesTEC-1 with the prospective LocoMMotion study of RWPC provides robust comparative evidence for a single-arm trial. Results from adjusted treatment comparisons demonstrated clinically and statistically significant improvements with teclistamab compared with RWPC in TCE (PI, IMiD, anti-CD38 antibody)-RRMM and highlight the clinical benefit of teclistamab as a novel and highly effective therapy to address unmet treatment needs in this patient population.
References
Orlowski RZ, Nagler A, Sonneveld P, et al. Randomized phase III study of pegylated liposomal doxorubicin plus bortezomib compared with bortezomib alone in relapsed or refractory multiple myeloma: combination therapy improves time to progression. J Clin Oncol. 2007;25:3892–901.
Dimopoulos MA, Moreau P, Terpos E, et al. EHA Guidelines Committee; multiple myeloma: EHA-ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32:309–22.
Chen C, Baldassarre F, Kanjeekal S, Herst J, Hicks L, Cheung M. Lenalidomide in multiple myeloma—a practice guideline. Curr Oncol. 2013;20:e136–49.
Gay F, Jackson G, Rosiñol L, et al. Maintenance treatment and survival in patients with myeloma: a systematic review and network meta-analysis. JAMA Oncol. 2018;4:1389–97.
Bird SA, Boyd K. Multiple myeloma: an overview of management. Palliat Care Soc Pract. 2019;13:1178224219868235.
Usmani SZ, Weiss BM, Plesner T, et al. Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood. 2016;128:37–44.
Raab MS, Cavo M, Delforge M, et al. Multiple myeloma: practice patterns across Europe. Br J Haematol. 2016;175:66–76.
Lee JH, Kim S-H. Treatment of relapsed and refractory multiple myeloma. Blood Res. 2020;55:S43-53.
Ramasamy K, Gay F, Weisel K, Zweegman S, Mateos MV, Richardson P. Improving outcomes for patients with relapsed multiple myeloma: challenges and considerations of current and emerging treatment options. Blood Rev. 2021;49: 100808.
Gandhi UH, Cornell RF, Lakshman A, et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia. 2019;33:2266–75.
Kumar V, Ailawadhi M, Dutta N, et al. Trends in early mortality from multiple myeloma: a population-based analysis. Clin Lymphoma Myeloma Leuk. 2021;21:e449–55.
Robak P, Drozdz I, Szemraj J, Robak T. Drug resistance in multiple myeloma. Cancer Treat Rev. 2018;70:199–208.
Pillarisetti K, Powers G, Luistro L, et al. Teclistamab is an active T cell-redirecting bispecific antibody against B-cell maturation antigen for multiple myeloma. Blood Adv. 2020;4:4538–49.
Usmani SZ, Garfall AL, van de Donk NWCJ, et al. Teclistamab, a B-cell maturation antigen × CD3 bispecific antibody, in patients with relapsed or refractory multiple myeloma (MajesTEC-1): a multicentre, open-label, single-arm, phase 1 study. Lancet. 2021;398:665–74.
Moreau P, Garfall AL, van de Donk NWCJ, et al. Teclistamab in relapsed or refractory multiple myeloma. N Engl J Med. 2022;387:495–505.
Durie BGM, Kumar SK, Usmani SZ, et al. Daratumumab-lenalidomide-dexamethasone vs standard-of-care regimens: efficacy in transplant-ineligible untreated myeloma. Am J Hematol. 2020;95:1486–94.
Mateos M-V, Weisel K, De Stefano V, et al. LocoMMotion: a prospective, non-interventional, multinational study of real-life current standards of care in patients with relapsed and/or refractory multiple myeloma. Leukemia. 2022;36:1371–6.
Li F, Morgan KL, Zaslavsky AM. Balancing covariates via propensity score weighting. J Am Stat Assoc. 2018;113:390–400.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Kumar S, Durie B, Nahi H, et al. Propensity score matching analysis to evaluate the comparative effectiveness of daratumumab versus real-world standard of care therapies for patients with heavily pretreated and refractory multiple myeloma. Leuk Lymphoma. 2019;60:163–71.
Harousseau J-L, Attal M, Avet-Loiseau H. The role of complete response in multiple myeloma. Blood. 2009;114:3139–46.
Chari A, Vogl DT, Gavriatopoulou M, et al. Oral selinexor-dexamethasone for triple-class refractory multiple myeloma. N Engl J Med. 2019;381:727–38.
Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21:207–21.
Munshi NC, Anderson LD Jr, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384:705–16.
Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398:314–24.
Acknowledgements
We thank all patients who participated in the MajesTEC-1 and LocoMMotion studies and the families and caregivers, physicians, and nurses who cared for the patients and supported the studies. We also thank the staff members at the MajesTEC-1 and LocoMMotion sites involved in data collection, data analysis, and interpretation, and acknowledge the contributions of Nichola Erler-Yates and Jedelyn Cabrieto (Janssen) to the data analyses.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. MajesTEC-1 was funded by Janssen Research & Development, LLC. LocoMMotion was funded by Janssen Research & Development, LLC and Legend Biotech, Inc. Funding for the publication of this study, including the journal’s Rapid Service and Open Access fees were provided by Janssen Global Services, LLC.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by John Bilbruck, PhD, and Linda Wychowski, PhD, of Eloquent Scientific Solutions, and funded by Janssen Global Services, LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Philippe Moreau, Aurore Perrot, Rachel Kobos, Jennifer Smit, and Maria-Victoria Mateos: Conceptualization, Investigation, Visualization, Writing-Reviewing and Editing Niels W. C. J. van de Donk, Michel Delforge, Hermann Einsele, Valerio De Stefano, Britta Besemer, Charlotte Pawlyn, Lionel Karlin, Salomon Manier, Xavier Leleu, Katja Weisel, and Ahmed Elsada: Conceptualization, Investigation, Writing-Reviewing and Editing Francesca Ghilotti: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing original draft, Writing-Reviewing and Editing Joris Diels: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing original draft, Writing-Reviewing and Editing Raul Morano and Mary Slavcev: Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing-Reviewing and Editing Vadim Strulev: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing original draft, Writing-Reviewing and Editing Lixia Pei: Conceptualization, Investigation, Methodology, Writing-Reviewing and Editing.
Prior Presentation
This manuscript is based on work that was previously presented at the 2022 American Society of Clinical Oncology Annual Meeting; June 3–7, 2022; Chicago, IL, USA and online. Niels W.C.J van de Donk, et al. Comparative efficacy of teclistamab (tec) versus current treatments (tx) in real-world clinical practice in the prospective LocoMMotion study in patients (pts) with triple-class exposed (TCE) relapsed/refractory multiple myeloma (RRMM). J Clin Oncol 40, 2022 (suppl 16; abstr 8016).
Disclosures
Philippe Moreau has held a consulting or advisory role for AbbVie, Amgen, Celgene, GlaxoSmithKline, Janssen, Oncopeptides, and Sanofi; and received honoraria from AbbVie, Amgen, Celgene, GlaxoSmithKline, Janssen-Cilag, Oncopeptides, and Sanofi. Niels W. C. J. van de Donk has received honoraria from Celgene; held a consulting or advisory role for Amgen, Bayer, Celgene, Janssen, Novartis, Roche, Servier, and Takeda; and received research funding from Amgen, BMS, Cellectis, and Janssen. Michel Delforge has held a consulting or advisory role for Amgen, Celgene, and Janssen; and received honoraria from Amgen, Celgene, and Janssen. Hermann Einsele has held a consulting or advisory role for Amgen, Bristol Myers Squibb, Celgene, Janssen, Novartis, and Takeda; received travel, accommodations, and/or expenses from Amgen, Bristol Myers Squibb, Celgene, Janssen, and Takeda; received honoraria from Amgen, Bristol Myers Squibb, Celgene, Janssen, Novartis, and Takeda; and received research funding from Amgen, Bristol Myers Squibb, Celgene, and Janssen. Valerio De Stefano has received honoraria from AbbVie, Amgen, Bristol Myers Squibb, Celgene, GlaxoSmithKline, Janssen-Cilag, Sanofi, and Takeda. Aurore Perrot has received honoraria from AbbVie, Amgen, Celgene, Janssen-Cilag, GlaxoSmithKline, Sanofi, and Takeda. Britta Besemer has received travel, accommodations, and/or expenses from Janssen-Cilag; and received honoraria from Janssen-Cilag. Charlotte Pawlyn has received honoraria from Amgen, Celgene/Bristol Myers Squibb, Janssen, Sanofi, and Takeda. Lionel Karlin reports employment (family member) by Aguettant; has received honoraria from AbbVie, Amgen, Celgene/Bristol Myers Squibb, GlaxoSmithKline, Janssen, Sanofi, and Takeda; has held a consulting or advisory role for AbbVie, Amgen, Celgene/Bristol Myers Squibb, GlaxoSmithKline, Janssen, Sanofi, and Takeda; and has received travel, accommodations, and/or expenses from Amgen, Janssen, Sanofi, and Takeda. Salomon Manier has received research funding from AbbVie, Celgene/Bristol Myers Squibb, Janssen, Novartis, and Takeda. Xavier Leleu has held a consulting or advisory role for AbbVie, Amgen, Bristol Myers Squibb, CARsgen Therapeutics, Celgene, Gilead Sciences, GlaxoSmithKline, Janssen-Cilag, Karyopharm Therapeutics, Merck, Novartis, Oncopeptides, Roche, and Takeda; received travel, accommodations, and/or expenses from Takeda; and received honoraria from AbbVie, Amgen, Bristol Myers Squibb, CARsgen Therapeutics, Celgene, GlaxoSmithKline, Janssen-Cilag, Karyopharm Therapeutics, Merck, Novartis, Oncopeptides, Roche, Sanofi, and Takeda. Katja Weisel has held a consulting or advisory role for Adaptive Biotechnologies, Amgen, Bristol Myers Squibb, Celgene, GlaxoSmithKline, Janssen-Cilag, Karyopharm Therapeutics, Oncopeptides, Roche, Sanofi, and Takeda; has received travel, accommodations, and/or expenses from Amgen, Bristol Myers Squibb, Celgene, GlaxoSmithKline, Janssen-Cilag, and Takeda; received honoraria from AbbVie, Adaptive Biotechnologies, Amgen, Bristol Myers Squibb, Celgene, GlaxoSmithKline, Janssen-Cilag, Karyopharm Therapeutics, Novartis, Oncopeptides, Pfizer, Roche/Genentech, Sanofi, and Takeda; and has received research funding from Amgen, Bristol Myers Squibb/Celgene, Celgene, GlaxoSmithKline, Janssen-Cilag, and Sanofi. Francesca Ghilotti is employed by Janssen. Joris Diels is employed by and has stock/other ownership interests in Janssen. Ahmed Elsada was employed by Janssen-Cilag during the conduct of the research and publication development; he is currently an employee of Bristol-Myers Squibb. Raul Morano is employed by Janssen. Vadim Strulev is employed by and has stock/other ownership interests in Janssen. Lixia Pei is employed by and has stock/other ownership interests in Janssen. Rachel Kobos is employed by and has stock/other ownership interests in Janssen. Jennifer Smit is employed by, has stock/other ownership interests in, and has received travel, accommodations, and/or expenses from Johnson & Johnson/Janssen. Mary Slavcev is employed by and has stock/other ownership interests in Janssen. Maria-Victoria Mateos has held a consulting or advisory role for AbbVie, Amgen, Celgene, GlaxoSmithKline, Janssen-Cilag, Pfizer, Regeneron, Roche/Genentech, and Takeda; and received honoraria from AbbVie/Genentech, Amgen, Celgene, GlaxoSmithKline, Janssen-Cilag, Sanofi, and Takeda.
Compliance With Ethics Guidelines
Data analyzed in this study were received from the MajesTEC-1 and LocoMMotion studies. MajesTEC-1 was conducted in accordance with the Declaration of Helsinki and International Conference on Harmonisation Guidelines for Good Clinical Practice. All patients provided written informed consent. An independent ethics committee or institutional review board at each study center approved the study protocol. The LocoMMotion study was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent. An independent ethics committee/institutional review board at each center approved the study protocol.
Data Availability
Data used for this study were based on the MajesTEC-1 and LocoMMotion studies. MajesTEC-1 data sharing is governed by the Janssen Pharmaceutical Companies of Johnson & Johnson data sharing policy that is available online. As noted on policy, requests for access to the study data can be submitted through Yale Open Data.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Moreau, P., van de Donk, N.W.C.J., Delforge, M. et al. Comparative Efficacy of Teclistamab Versus Current Treatments in Real-World Clinical Practice in the Prospective LocoMMotion Study in Patients with Triple-Class-Exposed Relapsed and/or Refractory Multiple Myeloma. Adv Ther 40, 2412–2425 (2023). https://doi.org/10.1007/s12325-023-02480-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02480-7