Abstract
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic condition associated with substantial clinical and economic burden. As multiple therapeutic options are available, patient preferences on treatment characteristics are key in T2DM therapeutic decision-making. This study aimed to determine the preferences of US patients with T2DM for therapies recommended for first pharmacologic intensification after metformin.
Methods
As part of a discrete choice experiment, an online survey was designed using literature review and qualitative interview findings. Eligibility was met by US patients with T2DM who were aged 18 years or older with an HbA1c ≥ 6.5%. Anonymized therapy profiles were created from six antidiabetic therapies including oral and injectable semaglutide, dulaglutide, empagliflozin, sitagliptin, and thiazolidinediones.
Results
Eligible patients (n = 500) had a mean HbA1c of 7.4%, and a mean BMI of 32.0 kg/m2, the majority of which (72.2%) were injectable-naïve. The treatment characteristic with greatest importance was mode and frequency of administration (35.5%), followed by body weight change (29.2%), cardiovascular event risk (19.1%), hypoglycemic event risk (9.9%), and HbA1c change (6.5%). An oral semaglutide-like profile was preferred by 91.9–70.1% of respondents depending on the comparator agent, and preference was significant in each comparison (p < 0.05); an injectable semaglutide-like profile was preferred by 89.3–55.7% of respondents in each comparison depending on the comparator agent.
Conclusion
Patients with T2DM in the USA are significantly more likely to prefer oral or injectable semaglutide-like profiles over those of key comparators from the glucagon-like peptide 1 receptor agonist, sodium-glucose cotransporter 2 inhibitor, dipeptidyl peptidase 4 inhibitor, and thiazolidinedione classes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Type 2 diabetes mellitus (T2DM) may be treated with a range of oral and injectable therapies. |
All glucagon-like peptide 1 receptor agonist (GLP-1 RA) therapies marketed to date are administered by injection; therefore, it is unknown how an oral formulation of a GLP-1 RA would be perceived by patients. |
This discrete choice experiment explored preferences for (unbranded) oral and injectable therapy profiles (across a variety of therapy classes) among US patients with T2DM. |
An oral semaglutide-like profile was preferred by 91.9–70.1% of respondents when compared to key comparators; mode and frequency of administration was shown to have the highest relative importance among attributes. |
US patients with T2DM appear to prefer oral or injectable semaglutide-like profiles over those of key comparators. |
The treatment attribute with highest relative importance was mode and frequency of administration, followed by weight change. |
Introduction
Type 2 diabetes mellitus (T2DM) is a progressive chronic complex metabolic condition characterized by deficient secretion of insulin along with insulin resistance, and consequent poor glycemic control [1], and is associated with cardiovascular, ophthalmic, and renal complications, which creates a substantial, and growing, clinical and economic burden on often already overloaded healthcare systems [2]. Recently the Centers for Disease Control and Prevention (CDC) reported that, in the USA, 34.2 million people of all ages (10.5% of the population) had diabetes, with T2DM accounting for 90–95% of all cases [3].
The American Diabetes Association (ADA) recommends metformin as the first-line pharmacologic therapy for T2DM, except among patients with compelling comorbid conditions. In patients with established atherosclerotic cardiovascular disease or indicators of high risk, established kidney disease or heart failure, a sodium-glucose cotransporter 2 inhibitor (SGLT2i) or glucagon-like peptide 1 receptor agonist (GLP-1 RA) with demonstrated cardiovascular disease benefit is recommended [4]. Further, if metformin alone cannot adequately control glycemia, treatment should be reassessed and intensified every 3–6 months. Metformin may be intensified with a further oral therapy such as a GLP-1 RA, SGLT2i, dipeptidyl peptidase 4 inhibitor (DPP4i), thiazolidinedione (TZD), or sulfonylurea [4]. Intensification with insulin therapy is also an option for patients requiring additional glycemic control. For most patients, GLP-1 RAs are recommended as the preferred initial injectable therapy. While GLP-1 RAs (a class which includes liraglutide, dulaglutide, exenatide, lixisenatide, and semaglutide) have conventionally been administered by subcutaneous injection, an oral formulation of semaglutide is now approved for use [5].
As T2DM acts via multiple pathophysiologic routes, treatments should therefore attempt to address these multiple pathways. This approach can often lead to polypharmacy unless agents that address multiple pathophysiologic pathways (such as GLP-1 RAs) are used. In addition, therapeutic inertia, defined as the failure to initiate or intensify therapy when therapeutic goals are not reached, has been found to be substantial in T2DM [6]. Possible reasons for therapeutic inertia include time constraints, lack of knowledge, differences in guideline recommendations, non-adherence, and concerns about hypoglycemia and weight gain. This, in turn, may result in delays in assessment and care, and avoidable exposure to chronic hyperglycemia and the complications associated with uncontrolled glycemic states [6]. Therefore, understanding patient perspective and preferences related to their treatment is vital to improve adherence and reduce this clinical inertia.
T2DM is largely self-managed. Working to support patients with T2DM is important to give them the tools and information needed to optimally manage their condition. The ADA recommends that a patient-centered approach should be used to guide the choice of pharmacologic agents as well, where considerations include efficacy, hypoglycemia risk, history of atherosclerotic cardiovascular disease, impact on body weight, potential side effects, renal effects, delivery method (oral versus subcutaneous), cost, and patient preferences [4]. Therefore, patient preferences for characteristics associated with potential treatments are key in therapeutic decision-making.
The aim of this study was to assess preferences of patients with T2DM for treatment choices based on treatment characteristics and outcomes in the USA. Using a discrete choice experiment (DCE), options were offered across the therapies for the management of T2DM typically recommended for first intensification after metformin of T2DM treatment by the ADA [4]. The quantitative DCE was conducted as an online survey, following a qualitative research phase, consisting of a targeted literature review (TLR) and qualitative interviews with physicians who treat patients with T2DM and patients with T2DM. The DCE is an established methodology in research to assess the trade-off patients are willing to make between characteristics through a series of alternative hypothetical scenarios to indirectly determine patient preferences. A number of similar studies have been conducted previously, focusing on injectable and oral GLP-1 RA therapies [7,8,9,10,11,12,13,14]. To align with US treatment patterns and provide insight on a broader range of scenarios, in the current study both injectable-experienced and injectable-naïve patients were surveyed, and the range of tested therapies included DPP4is, SGLT2is, and TZDs.
Methods
Development of Survey
A TLR and qualitative interviews were conducted to identify the most important attributes for use in the DCE survey. The methodology followed for the literature review and interviews is provided in the supplementary materials. This non-interventional study was conducted in accordance with all applicable regulations in the USA. Ethics approval for conducting research with patients with T2D was sought from Salus IRB (Austin, Texas), and the study was deemed to be exempt from requiring ethics review. This exempt status was granted on 30 January 2020. All participants provided informed consent to participant in this study.
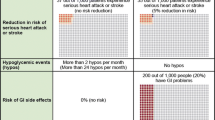
From the TLR and qualitative interviews, the following five treatment attributes were determined to be the most important to patients: mode, frequency, and requirements of administration; change in glycated hemoglobin (HbA1c) level with proposed treatment over 6 months; change in body weight with proposed treatment over 6 months; change in cardiovascular event risk as a result of treatment; risk of hypoglycemic events (defined as blood sugar level falling below what is healthy and causing symptoms such as shakiness, irritability, confusion, rapid heartbeat, and/or hunger) with proposed treatment over 6 months.
Therapy profiles were developed on the basis of these characteristics for the following six non-insulin antidiabetic therapies, which cover representative examples of most of the options recommended by the ADA for first intensification after metformin of T2DM treatment [4]: oral semaglutide (Rybelsus®, an oral GLP-1 RA); injectable semaglutide (Ozempic®, an injectable GLP-1 RA); dulaglutide (Trulicity®, an injectable GLP-1 RA); empagliflozin (Jardiance®, an SGLT2i); sitagliptin (Januvia®, a DPP4i); TZDs (as a class).
Appropriate levels for the efficacy and tolerability outcomes of the treatment attributes of interest were derived from clinical trial data for the four relevant therapy classes, primarily via published meta-analyses [15,16,17,18,19,20,21,22], and from US FDA labels. Clinical data were used to generate realistic minimum and maximum levels, and hypothetical levels were placed in the middle of each range (see Table 1). Attribute levels were then combined into product profiles, which were either presented alone or in choice sets of two profiles where respondents were asked to choose their preferred option, depending on the type of data being collected.
Two types of therapy profiles were developed: “hypothetical” profiles were assembled from the realistic attribute levels presented in Table 1; “real” profiles were developed from the efficacy and safety data for a given therapy from clinical trials [15,16,17,18,19,20,21,22].
For the hypothetical profiles, the “support.CEs” package within R was used to generate the optimal subset of choice sets. As the total number of generated choice sets was too high to be completed by one respondent at one time, sets were assigned to blocks. Specifically, eight unique hypothetical choice sets were assigned to each of two blocks (A and B) (see Supplementary Material Table S1).
Although clinical trial data was used to develop the real therapy profiles in this survey, the respondents were not made aware of this and were instead asked to consider “new treatments”. In cases where respondents were presented with choice sets (each containing two profiles), they were required to select only one profile from each choice set and could not skip any choice sets.
Final Survey
Within the DCE survey, initial questions established the eligibility of each respondent against pre-defined inclusion criteria and collected informed consent. Respondents’ preferences were tested through choice sets of hypothetical profiles, choice sets of real profiles for direct preference comparisons, and willingness to initiate treatment of real profiles. Final questions assessed health literacy and numeracy, collected further demographic data, and collected information on each respondent’s perceived health-related quality of life (HRQoL) assessed using EQ-5D-5L.
Respondents’ preferences were first collected using choice sets including two hypothetical therapy profiles (see Supplementary Material Table S2). Each individual respondent was assigned to one of two blocks of choice sets (A and B). Each block contained eight different unique hypothetical choice sets. Before the main set of hypothetical therapy profiles were presented, an example choice set was shown, in which one profile was clearly inferior. Any respondent who selected the clearly inferior profile (treatment A) was prompted to retry. Respondents could not progress past this choice set without selecting the clearly superior profile (treatment B). After the main series of hypothetical therapy profiles were presented, a further test choice set of hypothetical therapy profiles was shown, with again one clearly inferior profile. Respondents who selected the clearly inferior profile (treatment B) were marked as potentially giving unreliable answers.
Respondents’ preferences were then collected using choice sets each including two (anonymized) real therapy profiles. Choice sets were generated using network meta-analysis or clinical trial data for individual therapies [16,17,18, 21, 23,24,25,26], or head-to-head trial data where available [27, 28]. In cases where multiple doses with differing outcomes are used in clinical practice (e.g., 7 mg and 14 mg oral semaglutide), simple arithmetic means were calculated to illustrate the efficacy and tolerability of an idealized dose. In cases where an outcome could not be determined for an individual named therapy, an estimated class effect was instead used (e.g., the risk of hypoglycemic events with GLP-1 RA therapy, and all outcomes for TZDs, which were examined as a class) [21, 25].
Respondents were then asked on their willingness to initiate six (anonymized) real therapy profiles, presented in Table 2. For each profile, respondents were required to describe their willingness to initiate treatment, by selecting one of the following options, with no option to skip: “very unwilling”, “unwilling”, “neutral”, “willing”, “very willing”.
Survey Respondents
Potential respondents were contacted by e-mail to participate in the survey. As respondents could decline to participate, or be excluded during participation in the survey, respondents were continually recruited until 500 sets of results were captured. Eligible respondents fulfilled each of the following criteria: age of 18 years or older; current residence in the USA; ability to read and understand the English language; diagnosis of T2DM (and no other type of diabetes); currently receiving medication to control blood glucose level, which began at least 6 months prior to the survey;Footnote 1 never received insulin to control blood glucose level; HbA1c level of ≥ 6.5% at the latest time of measuring (within the past year);Footnote 2 no health issues that make it difficult to participate in the survey (e.g., issues with seeing or reading, or issues with understanding or answering questions); not employed at a pharmaceutical company, or in a role with responsibility for directly treating patients with diabetes; willing to participate in the survey, and to provide informed consent. All respondents of the survey confirmed their willingness to participate, and gave explicit informed consent to participate, and for their demographic data and preference data to be captured and stored for research purposes and reported in an anonymized manner.
Data Analysis
The analyses of hypothetical choice set results used a conditional logit regression model to regress stated preferences to determine the crude relative preference for each attribute. Only main effects were estimated, i.e., no interaction terms were examined.
The coefficients on the independent variables from the regression were interpreted as relative preference weights, indicating the relative strength of preference for each attribute level. Larger positive coefficients indicated that respondents preferred that attribute level to levels that have smaller or negative coefficients.
For subgroup analyses, respondents were grouped by injectable-naïve or injectable-experienced status, by gender (male or female), by age (< 65 or ≥ 65 years), by HbA1c level in relation to median or subjective target (HbA1c < 7.2% or ≥ 7.2%; HbA1c within or above personal target), by obesity (BMI < 30 kg/m2 or ≥ 30 kg/m2), by HRQoL (impairment or no impairment by EQ-5D-5L), and by answer to test choice set (correct or incorrect).
Results
Characteristics of Survey Respondents
Of the 4345 patients screened for the DCE survey, 500 met the eligibility criteria. The clinical and demographic characteristics of these patients are presented in Table S1 of the supplementary material. Within the eligible patient group (n = 500), 42.6% were female. The mean age of respondents was 65.5 years, and the majority of respondents (69.6%) were aged between 60 and 80. Most respondents had attained at least a degree-level education (56.8%). The majority of participants were retired (57.8%). The mean BMI within the sample was 32.0 kg/m2, with 56.0% of respondents considered obese (> 30 kg/m2), and 0.8% considered underweight (< 18.5 kg/m2) [29]. Respondents had been diagnosed with T2DM for a mean of 11.4 years prior to the survey, and had been receiving medication to control blood glucose for a mean of 8.9 years. Respondents’ mean reported HbA1c was 7.4%; specifically, 23.0% had tightly controlled HbA1c by ADA standards (defined as ≥ 6.5% to ≤ 6.9%), while 51.4% had loosely controlled HbA1c (≥ 7.0% to ≤ 7.9%) [30]; most respondents (62.4%) reported that their current HbA1c was outside the target set by their physician, and 18.8% reported having experienced complications as a result of T2DM.
Most respondents (93.4%) answered the test question correctly, selecting the clearly superior choice. The remainder (6.6%) therefore potentially provided unreliable results and were subgrouped for further analysis. The proportion of respondents with at least an adequate level of self-reported health literacy was 90.4%, and the proportion with adequate numeracy was 95.0%.
Relative Importance of Attributes and Levels in Hypothetical Profiles
In the full sample of the current study (n = 500), 35.5% of the total variance in respondents’ decision-making between profiles was predicted by mode and frequency of administration, while 29.2% was predicted by change in body weight. Less important attributes were change in cardiovascular event risk (19.1%), risk of hypoglycemic events (9.9%), and change in HbA1c (6.5%). Relative preference weights of attribute levels (relative to the least-preferred level in each attribute) are presented in Fig. 1. All attributes showed a linear upwards trend as expected, with the exception of risk of hypoglycemic events. This may be because the levels presented for this attribute were not sufficiently different to be considered notable by patients.
In the injectable-naïve subgroup (which made up 72.2% of the sample; n = 361), the ordering of attributes by importance matched the full sample with mode and frequency of administration rated as most important, followed by change in body weight, change in cardiovascular event risk, risk of hypoglycemic events, and lastly change in HbA1c (Figs. 2, 3). However, in the injectable-experienced subgroup (n = 139), the ordering of administration and body weight change attributes was reversed, as was the ordering of hypoglycemia risk and HbA1c change attributes.
In four of the five attributes, the relative utility of levels increased linearly according to the expected trend, from “worst” to “best” levels (i.e., from daily injection, to weekly injection, to daily tablet (with restriction) to daily tablet (without restriction); from body weight increase, to no body weight change, to body weight loss (− 5.5 lb), to body weight loss (− 10.5 lb); from no change in cardiovascular risk to greatest improvement in cardiovascular risk; from small HbA1c improvement to large HbA1c improvement). However, the relative utility of hypoglycemia risk levels did not increase linearly from the “worst” to “best” levels (i.e., from greatest to lowest risk).
Attributes were not typically ranked in a different order in subgroups. No subgroup provided attribute preferences that were significantly different to its corresponding subgroup (all comparisons p > 0.05 by t testing).
Relative Preference for (Anonymized) Real Therapy Profiles
Evaluable direct preference results were available from all 500 respondents, and choice sets were answered by 248 to 166 respondents each, as per the block design (see Supplementary Material Table S2). In the full population, the oral semaglutide-like profile was preferred by 91.9–70.1% of respondents in each comparison (Fig. 4a), and preference was significant in each comparison (p < 0.05 by chi-squared testing); the injectable semaglutide-like profile was preferred by 89.3–55.7% of respondents in each comparison (Fig. 4b), and preference was significant in each comparison except with the empagliflozin-like profile (55.7%).
In injectable-experienced respondents, preference for the injectable semaglutide-like profile was increased (94.3–84.6% of respondents depending on comparison), while preference for the oral semaglutide-like profile remained high (92.8–71.8%), and semaglutide was significantly preferred in all comparisons. In injectable-naïve respondents, preference for the injectable semaglutide-like profile was decreased (87.4–42.0%) and was not significant in comparisons with the empagliflozin-like and sitagliptin-like profiles; preference for the oral semaglutide-like profile remained high (91.6–69.5%) and was significant in all comparisons.
Willingness to Initiate Treatment with (Anonymized) Real Therapy Profiles
Evaluable results for willingness to initiate treatment with (anonymized) real therapy profiles were available from all 500 respondents, and questions were answered by 500 or 125 respondents each as per the block design. In the full population, respondents were more often willing (i.e., answered “willing” or “very willing”) to initiate treatment with semaglutide-like profiles, relative to comparators—with the exception of injectable semaglutide (59.2%) versus empagliflozin (85.6%).
Injectable-experienced participants were more willing to initiate treatment with injectable therapies (i.e., semaglutide and dulaglutide; 86.3% and 84.9%, respectively; see Fig. 5); injectable-naïve participants were slightly less willing (48.8% and 43.5%). Willingness to initiate oral semaglutide or empagliflozin remained high in the full population and both subgroups (87.8–84.9%). Willingness to initiate injectable and oral semaglutide, dulaglutide, and empagliflozin was high in the injectable-experienced group (87.8–84.9%).
Discussion
Overall, the results of this DCE survey show that US patients with T2DM prefer oral antidiabetic treatments over injectable treatments. The results also suggest that US patients with T2DM are significantly more likely to prefer oral or injectable semaglutide-like profiles over those of the selected GLP-1 RA, SGLT2i, DPP4i, and TZD comparators presented, with the oral semaglutide-like profile being preferred over any other oral antidiabetic therapy. In comparison to the empaglifozin profile, 69.5% of oral antidiabetic therapy users preferred the oral semaglutide profile, suggesting that improvements in clinical parameters, such as body weight change and blood glucose level, outweigh any disadvantages in the dosing conditions. Additionally, patients are more willing to initiate treatment with oral semaglutide-like profiles compared to all other profiles, even in patients who are injectable-experienced.
Analyses of hypothetical preference results suggest that mode and frequency of administration was the most important attribute considered in patients’ decision-making process (35.5%), followed by change in body weight (29.2%). Cardiovascular event risk was also identified as an important treatment characteristic for US patients with T2DM (19.1%). Risk of hypoglycemic events (9.9%) and change in HbA1c (6.5%) were substantially less important in this context.
The relative importance of HbA1c change within the survey results was low, and this was estimated to be the least important of the five tested attributes in this context. This may be explained by the magnitude of change described in all levels of this attribute, and the HbA1c levels of respondents. For approximately half of respondents (the 51.4% with loosely controlled HbA1c of ≥ 7.0% to ≤ 7.9%), three of the four presented reductions in HbA1c would be sufficient to reach a level of tight control (≤ 6.9%). In addition, many patients may assume that any new therapy will improve HbA1c and that most therapies provide equivalent HbA1c benefit. In subgroup analyses, this attribute remained the least important regardless of HbA1c (above or below median, or within or outside personal target). These findings suggest that, in this patient population, the impact of treatment on HbA1c is not a primary factor when selecting between modern non-insulin therapy options, which generally have high efficacy. This is an area that needs further exploration as further potency and durability of treatment may need to be added to future trials.
In this context, body weight change was estimated to be the second-most important attribute in respondents’ decision-making, in a population where 56.0% were obese according to US criteria (BMI ≥ 30 kg/m2) [29]. This difference may be explained by the inclusion, in the current study, of a wider range of body weight change attribute levels: + 5½ lb to − 10½ lb (+ 2.5 kg, to − 4.8 kg), versus the + 0.3 kg to − 2.4 kg range derived from oral semaglutide clinical trial data for the 2019 Japan DCE [14, 31, 32].
When comparing the results of the current study to those of previous DCEs (comparing different GLP-1 RA-like profiles), it is apparent that the relative importance of different treatment attributes changes substantially depending on the presented levels. For example, in the current study the administration attribute was considered to be the most important, while in another DCE study conducted in the USA by Polster et al. (where administration levels described daily or twice daily injectable therapy), dose frequency was ranked last out of four attributes [13]. In addition, the phrasing used to describe levels may also have an effect on relative importance. For example, the administration level for oral semaglutide was described as “Pill taken once per day, at least 30 min before the first meal or drink of the day and taking other oral medications” in our survey but could equally be described as “Pill taken once per day, requiring fasting for 6 h before and 30 min after dosing”. The attribute levels presented in the current study were based on data for the therapies of interest from network meta-analyses or clinical trials. Estimates from network meta-analyses were used as a default, but direct head-to-head data were used in direct comparison choice sets when available [27, 28].
The current study and four other previous GLP-1 RA-focused DCE studies included questions on direct preference between real GLP-1 RA therapy profiles [7, 11, 12, 14]. Other GLP-1 RA-focused DCE studies did not include a direct comparison of real GLP-1 RA therapy profiles [8,9,10], or instead used a time trade-off (TTO) method to determine direct preference [13]. Across the five studies presenting direct preference data, dulaglutide was consistently preferred to liraglutide, and semaglutide was consistently preferred to both dulaglutide and liraglutide [7, 11, 12, 14]. In addition, oral semaglutide appeared to be particularly highly preferred. Similar results were seen for respondents’ willingness to initiate treatment with real GLP-1 RA therapy profiles, which were also available from the same published studies [7, 11, 12, 14]. Respondents were more willing to initiate treatment with dulaglutide relative to liraglutide, and were more willing to initiate treatment with semaglutide relative to dulaglutide [7, 11, 12, 14].
The sample size of the current study (n = 500) was comparable to those of two GLP-1 RA-focused DCEs conducted in the USA by Hauber et al. and Polster et al. (n = 643 and n = 382, respectively) [10, 13].
While the average age of respondents in the current study (mean 65.5, median 67.0) was higher than that typically seen in similar GLP-1 RA-focused DCE studies [33], this does not appear to have biased responses towards oral or injectable semaglutide: preference for oral and injectable semaglutide remains high among participants younger than the median age (90.4–66.2%, depending on comparison) or aged below 60 (92.3–65.8%).
The average level of glycemic control of survey respondents (mean HbA1c 7.4%; median 7.2%; 66.8% with loosely controlled or uncontrolled disease by ADA target [1]; 62.4% with uncontrolled disease by their personal target), along with their insulin-naïve status, suggests that results may be generalized to US patients with T2DM who require first intensification of treatment. However, caution is advised when drawing conclusions from this study for patients outside of the USA.
Limitations
A few limitations of this study have been noted. Firstly, the reported rates of T2DM-related complications were substantially lower than those seen in other sources such as disease registries: peripheral neuropathy has previously been observed in 42.2% of patients (versus 14.0% in the current study) [34]; vision disability in 11.7% (versus 7.4% in the current study) [35]; kidney disease in 36.5% (versus 3.0% in the current study) [35]; and cardiovascular disease in 32.2% (versus 2.2% in the current study) [36]. This may be because respondents considered these to be separate comorbid diseases rather than T2DM-related complications. Alternatively, the respondents may not have been familiar with the terminology used to describe these complications.
Secondly, findings related to cardiovascular event risk in the current study should be interpreted with caution, as the 21% risk reduction (versus placebo) displayed within oral semaglutide-like profiles in this survey was not statistically significant in the PIONEER 6 cardiovascular outcome trial, possibly because of the limited sample size of that trial [17]. Future data may become available to confirm the true magnitude and level of significance of this risk reduction with oral semaglutide. In the meantime, these results could be considered in the context of pooled data on oral and injectable semaglutide from the PIONEER 6 and SUSTAIN 6 trials, which show a significant risk reduction of 24% versus placebo [37].
In the current study, five treatment attributes were tested, after selection through substantial qualitative research. Guidance from ISPOR suggests that 8–16 is the ideal number of choice tasks in a DCE [38], and the results of the TLR conducted prior to the survey found that the majority of comparable DCE studies used between five and eight attributes. In addition, a recent systematic literature review by Thieu et al. reported that (among six DCE studies in T2DM) six was the median number of attributes used, in testing up to two GLP-1 RA therapies [33]. Therefore, it was extrapolated that approximately five attributes per question would be the ideal in the current study, to allow the intended number of therapies and treatment classes to be covered within the survey. Other GLP-1 RA-focused DCE studies have tested six [11, 12], or even eight attributes [8, 9]. Therefore, the current study focused on increased coverage of therapies and treatment classes, rather than increased coverage of attributes.
In addition, in the current study, respondents completed the DCE survey remotely, with no input from study researchers. Conversely, in two previous GLP-1 RA-focused DCE studies conducted by Gelhorn et al. (to support dulaglutide), choice sets were administered in person to respondents by a trained moderator [11, 12]. However, online self-completion appears to be common in other GLP-1 RA-focused DCE studies [7,8,9,10, 13, 14], and other features were included in the current study to ensure respondents’ understanding (such as example and test choice sets).
Finally, the current study did not include a pilot test survey phase. However, substantial qualitative research was conducted with expert physicians and persons with T2DM in the USA, in order to determine the best presentation methods for use within the final survey. Additionally, elements to allow testing of response quality were incorporated into the survey design.
Conclusion
Injectable-naïve and injectable-experienced US patients with T2DM are significantly more likely to prefer oral or injectable semaglutide-like profiles over those of key comparators from the GLP-1 RA, SGLT2i, DPP4i, and TZD classes. Patients are also more willing to initiate treatment with oral semaglutide-like profiles than with any of these comparator profiles. When such patients compare these therapies, mode and frequency of administration is likely to be the greatest factor in their decision-making, followed by body weight change. While the following treatment attributes were not investigated in this study, research into the importance of treatment cost, side effects such as risk of urinary tract or genital infection, risk of adverse gastrointestinal events, and change in blood pressure would also be useful to further inform patient preference. Future research on patient preference for oral semaglutide could use alternative methods such as TTO or willingness-to-pay analysis, which have occasionally been used to assess preference for GLP-1 RA therapy profiles [13, 39].
Notes
Quotas were initially applied to seek a suitable mix of respondents for analysis: 33% injectable-naïve, ~ 33% with past injectable use, and 33% with current injectable use. However, this was later relaxed to improve feasibility.
To improve feasibility, a limited number of respondents with unknown HbA1c were accepted (n = 51; 10.2%).
References
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S13–27.
Ali SN, Dang-Tan T, Valentine WJ, Hansen BB. Evaluation of the clinical and economic burden of poor glycemic control associated with therapeutic inertia in patients with type 2 diabetes in the United States. Adv Ther. 2020;37(2):869–82.
Centers for Disease Control and Prevenetion. National Diabetes Statistics Report 2020: estimates of diabetes and its burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statisticsreport.pdf. Accessed 5 July 2022.
American Diabetes Association. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S73–85.
Nauck MA, Quast DR, Wefers J, Meier JJ. GLP-1 receptor agonists in the treatment of type 2 diabetes – state-of-the-art. Mol Metab. 2020;46:101102.
Khunti S, Davies MJ, Khunti K. Clinical inertia in the management of type 2 diabetes mellitus: a focused literature review. Br J Diabetes. 2015;15(2):65–9.
Brooks A, Langer J, Tervonen T, Hemmingsen MP, Eguchi K, Bacci ED. Patient preferences for GLP-1 receptor agonist treatment of type 2 diabetes mellitus in Japan: a discrete choice experiment. Diabetes Ther. 2019;10(2):735–49.
Qin L, Chen S, Flood E, et al. Glucagon-like peptide-1 receptor agonist treatment attributes important to injection-experienced patients with type 2 diabetes mellitus: a preference study in Germany and the United Kingdom. Diabetes Ther. 2017;8(2):335–53.
Qin L, Chen S, Flood E, et al. Glucagon-like peptide-1 receptor agonist treatment attributes important to injection-naive patients with type 2 diabetes mellitus: a multinational preference study. Diabetes Ther. 2017;8(2):321–34.
Hauber AB, Nguyen H, Posner J, Kalsekar I, Ruggles J. A discrete-choice experiment to quantify patient preferences for frequency of glucagon-like peptide-1 receptor agonist injections in the treatment of type 2 diabetes. Curr Med Res Opin. 2016;32(2):251–62.
Gelhorn HL, Poon JL, Davies EW, Paczkowski R, Curtis SE, Boye KS. Evaluating preferences for profiles of GLP-1 receptor agonists among injection-naive type 2 diabetes patients in the UK. Patient Prefer Adherence. 2015;9:1611–22.
Gelhorn HL, Bacci ED, Poon JL, Boye KS, Suzuki S, Babineaux SM. Evaluating preferences for profiles of glucagon-like peptide-1 receptor agonists among injection-naive type 2 diabetes patients in Japan. Patient Prefer Adherence. 2016;10:1337–48.
Polster M, Zanutto E, McDonald S, Conner C, Hammer M. A comparison of preferences for two GLP-1 products—liraglutide and exenatide—for the treatment of type 2 diabetes. J Med Econ. 2010;13(4):655–61.
Igarashi A, Hansen BB, Langer J, et al. Preference for oral and injectable GLP-1 RA therapy profiles in Japanese patients with type 2 diabetes: a discrete choice experiment. Adv Ther. 2020;36:1–18.
Scheen AJ. Reduction in HbA1c with SGLT2 inhibitors vs. DPP-4 inhibitors as add-ons to metformin monotherapy according to baseline HbA1c: a systematic review of randomized controlled trials. Diabetes Metab. 2020;46(3):186–96.
Qian D, Zhang T, Zheng P, et al. Comparison of oral antidiabetic drugs as add-on treatments in patients with type 2 diabetes uncontrolled on metformin: a network meta-analysis. Diabetes Ther. 2018;9(5):1945–58.
Pearson S, Kietsiriroje N, Ajjan RA. Oral semaglutide in the management of type 2 diabetes: a report on the evidence to date. Diabetes Metab Syndr Obes Targets Ther. 2019;12:2515.
Nuhoho S, Gupta J, Hansen BB, Fletcher-Louis M, Dang-Tan T, Paine A. Orally administered semaglutide versus GLP-1 RAs in patients with type 2 diabetes previously receiving 1–2 oral antidiabetics: systematic review and network meta-analysis. Diabetes Ther. 2019;10(6):2183–99.
Li Z, Zhang Y, Quan X, et al. Efficacy and acceptability of glycemic control of glucagon-like peptide-1 receptor agonists among type 2 diabetes: a systematic review and network meta-analysis. PLoS One. 2016;11(5): e0154206.
Kanters S, Wilkinson L, Vrazic H, et al. Comparative efficacy of once-weekly semaglutide versus SGLT-2 inhibitors in patients inadequately controlled with one to two oral antidiabetic drugs: a systematic literature review and network meta-analysis. BMJ Open. 2019;9(7): e023458.
Kamalinia S, Josse RG, Donio PJ, Leduc L, Shah BR, Tobe SW. Risk of any hypoglycaemia with newer antihyperglycaemic agents in patients with type 2 diabetes: a systematic review and meta-analysis. Endocrinol Diabetes Metab. 2020;3(1): e00100.
Fei Y, Tsoi M-F, Cheung BMY. Cardiovascular outcomes in trials of new antidiabetic drug classes: a network meta-analysis. Cardiovasc Diabetol. 2019;18(1):1–13.
Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC. The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care. 2010;33(8):1859–64.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Erdmann E, Charbonnel B, Wilcox R. Thiazolidinediones and cardiovascular risk—a question of balance. Curr Cardiol Rev. 2009;5(3):155–65.
Green JB, Bethel MA, Armstrong PW, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–42.
Rosenstock J, Allison D, Birkenfeld AL, et al. Effect of additional oral semaglutide vs sitagliptin on glycated hemoglobin in adults with type 2 diabetes uncontrolled with metformin alone or with sulfonylurea: the PIONEER 3 randomized clinical trial. J Am Med Assoc. 2019;321(15):1466–80.
Rodbard HW, Rosenstock J, Canani LH, et al. Oral semaglutide versus empagliflozin in patients with type 2 diabetes uncontrolled on metformin: the PIONEER 2 trial. Diabetes Care. 2019;42(12):2272–81.
Centers for Disease Control and Prevention. Defining adult overweight and obesity 2020. https://www.cdc.gov/obesity/adult/defining.html. Accessed 17 Sept 2020.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2020. Diabetes Care. 2020;43(Supplement 1):S66–76.
Yabe D, Nakamura J, Kaneto H, et al. Safety and efficacy of oral semaglutide versus dulaglutide in Japanese patients with type 2 diabetes (PIONEER 10): an open-label, randomised, active-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 2020;8(5):P392-406.
Yamada Y, Katagiri H, Hamamoto Y, et al. Dose-response, efficacy, and safety of oral semaglutide monotherapy in Japanese patients with type 2 diabetes (PIONEER 9): a 52-week, phase 2/3a, randomised, controlled trial. Lancet Diabetes Endocrinol. 2020;8(5):P377–91.
Thieu VT, Robinson S, Kennedy-Martin T, Boye KS, Garcia-Perez LE. Patient preferences for glucagon-like peptide 1 receptor-agonist treatment attributes. Patient Prefer Adherence. 2019;13:561–76.
Pfannkuche A, Alhajjar A, Ming A, Walter I, Piehler C, Mertens PR. Prevalence and risk factors of diabetic peripheral neuropathy in a diabetics cohort: Register initiative “diabetes and nerves.” Endocr Metab Sci. 2020;1(1–2): 100053.
Centers for Disease Control and Prevention. Coexisting conditions and complications 2020. https://www.cdc.gov/diabetes/data/statistics-report/coexisting-conditions-complications.html. Accessed 5 July 2022.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):1–19.
Husain M, Bain SC, Jeppesen OK, et al. Semaglutide (SUSTAIN and PIONEER) reduces cardiovascular events in type 2 diabetes across varying cardiovascular risk. Diabetes Obes Metab. 2020;22(3):442–51.
Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
Jendle J, Torffvit O, Ridderstrale M, Lammert M, Ericsson A, Bogelund M. Willingness to pay for health improvements associated with anti-diabetes treatments for people with type 2 diabetes. Curr Med Res Opin. 2010;26(4):917–23.
Acknowledgements
Funding
Adelphi Values PROVE were commissioned by Novo Nordisk to conduct and report this research. Novo Nordisk funded the Rapid Service and Open Access Fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Sarah N. Ali, Barrie Chubb, Kristina DiPietrantonio, Hannah Collings, Robin Wyn and Martina Smith were involved in the concept and planning of the work described; acquisition, analysis and interpretation of the data; drafting and/or critical revision of the manuscript; and approved the final submitted version of the manuscript. Jay H. Shubrook and Michael Radin were involved in the concept and planning of the work described; analysis and interpretation of the data; drafting and/or critical revision of the manuscript; and approved the final submitted version of the manuscript.
Disclosures
Jay H. Shubrook receives consultancy fees from Novo Nordisk Ltd. Other disclosures–Abbott, Bayer, AstraZeneca, Eli Lilly and Nevro Corp. Michael Radin, Sarah N. Ali, and Barrie Chubb are employees of Novo Nordisk Ltd. Kristina DiPietrantonio, Hannah Collings, Robin Wyn, and Martina Smith are employees of Adelphi Values PROVE, or were employees of Adelphi Values PROVE at the time of the conduct and reporting of this research; Adelphi Values PROVE were commissioned by Novo Nordisk to conduct and report this research. Kristina DiPietrantonio is now an employee of Adelphi Research.
Compliance with Ethics Guidelines
This non-interventional study was conducted in accordance with all applicable regulations in the USA. Ethics approval for conducting research with patients with T2D was sought from Salus IRB (Austin, Texas), and the study was granted exempt status on 30 January 2020 under exemption reference 45CFR46.104(d). This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. All subjects provided informed consent to participate in this study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shubrook, J.H., Radin, M., Ali, S.N. et al. Preference for Type 2 Diabetes Therapies in the United States: A Discrete Choice Experiment. Adv Ther 39, 4114–4130 (2022). https://doi.org/10.1007/s12325-022-02181-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02181-7