Abstract
Introduction
Therapeutic inertia refers to the failure to initiate or intensify treatment in a timely manner and is widespread in type 2 diabetes (T2D) despite the well-established importance of maintaining good glycemic control. The aim of this analysis was to quantify the clinical and economic burden associated with poor glycemic control due to therapeutic inertia in patients with T2D in the USA.
Methods
The IQVIA CORE Diabetes Model was used to simulate life expectancy, costs associated with diabetes-related complications, and lost workplace productivity in US patients. Baseline glycated hemoglobin (HbA1c) levels were 7.0% (53 mmol/mol), 9.0% (75 mmol/mol), 11.0% (97 mmol/mol) 13.0% (119 mmol/mol), or 15.0% (140 mmol/mol), with targets of 6.5% (48 mmol/mol), 7.0% (53 mmol/mol), 8.0% (64 mmol/mol), or 9.0% (75 mmol/mol) depending on baseline HbA1c, across several delayed intensification scenarios (values above target were defined as poor control). The burden associated with intensification delays of 1, 2, 3, 5, and 7 years was estimated over time horizons of 1–30 years. Future costs and clinical benefits were discounted at 3% annually.
Results
In a population of 13.4 million patients with T2D and baseline HbA1c of 9.0% (75 mmol/mol), delaying intensification of therapy by 1 year was associated with a loss of approximately 13,390 life-years and increased total costs of US dollars (USD) 7.3 billion (1-year time horizon). Longer delays in intensification were associated with a greater economic burden. Delaying intensification by 7 years was projected to cost approximately 3 million life-years and USD 223 billion over a 30-year time horizon.
Conclusion
Therapeutic inertia is common in routine clinical practice and makes a substantial contribution to the burden associated with type 2 diabetes in the USA. Initiatives and interventions aimed at preventing therapeutic inertia are needed to improve clinical outcomes and avoid excess costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Therapeutic inertia, or the failure to initiate or intensify treatment in a timely manner, is common in patients with type 2 diabetes and makes a substantial contribution to the burden associated with the disease in the USA. |
We performed a health economic modeling analysis to quantify the clinical and economic burden associated with poor glycemic control due to therapeutic inertia based on published clinical data and unit costs to estimate complication costs and lost workplace productivity. |
It was estimated that in a population of 13.4 million patients with poor glycemic control (HbA1c 9.0% [75 mmol/mol]), delaying intensification of therapy by 1 year was associated with a loss of approximately 13,390 life-years and increased total costs of USD 7.3 billion (1-year time horizon). |
This modeling analysis provides evidence that initiatives and interventions aimed at preventing therapeutic inertia could play an important role in improving clinical outcomes and avoiding excess costs. |
Introduction
Recently published figures from the Centers for Disease Control and Prevention (CDC) estimate that in the USA there are currently over 30 million people living with diabetes, of whom 90–95% have type 2 diabetes [1]. Moreover, with over 4000 new diabetes cases diagnosed every day [1], by 2030 the number of people living with diabetes is expected to reach approximately 55 million [2]. Type 2 diabetes is a chronic progressive disease associated with cardiovascular, ophthalmic, and renal complications, which places a considerable, and growing, clinical and economic burden on often already overstretched healthcare systems. In the USA, over the period 2012–2017, the total economic burden associated with diabetes increased by 26% to US dollars (USD) 327 billion, of which USD 237 million was attributable to direct medical costs [3]. The economic burden of diabetes is now such that the treatment and management of diabetes and its associated complications account for one in every four healthcare dollars spent in the USA [3]. Any new interventions or initiatives with the potential to mitigate the burden of disease associated with diabetes may have a notable impact on overall healthcare spending in the USA.
A fundamental goal of type 2 diabetes therapy is to delay or ideally prevent long-term diabetes-related complications, which is achieved through an individualized approach to treatment including the maintenance of good glycemic control and management of other risk factors such as systolic blood pressure and serum lipid levels [4]. Despite the elevated risk of diabetes-related complications associated with poor glycemic control, there is often a therapeutic inertia toward the intensification of treatment at all stages of disease. Data from the National Health and Nutrition Examination Survey (NHANES) indicated that, during 2011–2014, over one-third of patients failed to achieve individualized glycated hemoglobin (HbA1c) targets and 15.5% of patients had HbA1c > 9.0% (75 mmol/mol) [5]. A recent study reported that there was frequently a delay in physicians responding to poor glycemic control and that, even among patients with HbA1c ≥ 9.0% (75 mmol/mol), therapy was not intensified in more than 40% of patients during a 6-month follow-up period [6]. Therapeutic inertia specifically around the time of initiation and intensification of insulin is especially pronounced, particularly in primary care [7]. For example, in the USA, a recent real-world data analysis showed that even after eventually initiating basal insulin, at 6 months post-insulin initiation, 81% of patients failed to achieve a target of HbA1c < 7.0% (53 mmol/mol) and at 12 months, only 67% of patients with HbA1c > 9.0% (75 mmol/mol) had intensified treatment [8]. These findings prompted the study authors to describe basal insulin uptitration in this study cohort as “slow and insufficient”.
In light of recent reports highlighting the challenge of therapeutic inertia in the USA [6, 8], the aim of the present analysis was to examine the clinical and economic burden associated with poor glycemic control due to delayed intensification of therapy across a range of glycemic control scenarios and time horizons in the US setting on a patient and population level.
Methods
Modeling Approach
Long-term cost-effectiveness analysis was performed using the IQVIA CORE Diabetes Model (CDM) Version 9.0 (IQVIA, Basel, Switzerland). The CDM is a published and validated, non-product-specific policy analysis tool that can be used to project long-term clinical and economic outcomes in type 1 or type 2 diabetes [9,10,11]. Complications and mortality attributable to diabetes-related complications were captured with the risk for cardiovascular complications predicted using the United Kingdom Prospective Diabetes Study 68 equations and background mortality was included using US-specific life tables published by the World Health Organization [12, 13]. All simulations were performed using a first-order Monte Carlo approach.
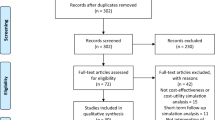
Outcomes were projected over time horizons of 1, 2, 3, 5, 10, and 30 years and scenarios were assessed in which baseline HbA1c was set at 7.0% (53 mmol/mol), 9.0% (75 mmol/mol), 11.0% (97 mmol/mol), 13.0% (119 mmol/mol), and 15.0% (140 mmol/mol) (Table 1) (a range of treatment effects were modeled for each baseline HbA1c value with targets set to 6.5% (48 mmol/mol), 7.0% (53 mmol/mol), 8.0% (64 mmol/mol), or 9.0% (75 mmol/mol) depending on baseline HbA1c). Glycemic control (HbA1c) targets were aligned with previously published guidance from the American Association of Clinical Endocrinologists for 6.5% (48 mmol/mol) and the American Diabetes Association (ADA) for 6.5% (48 mmol/mol), 7.0% (53 mmol/mol), and 8.0% (64 mmol/mol) according to individual patient characteristics [14, 15]. The HbA1c target of 9.0% is aligned with the US Healthcare Effectiveness Data and Information Set threshold for poor glycemic control [16]. For each time horizon and baseline HbA1c, scenarios were performed comparing outcomes with immediate intensification of treatment versus a delay in intensification of 1, 2, 3, 5, and 7 years. In the analysis, simulated patients were assumed to maintain good glycemic control (at the specified target HbA1c level), or to be in poor glycemic control (at the baseline HbA1c level) for a defined period of time before HbA1c was lowered to the target level for the remaining duration of the simulation (or the patient died in the simulation). Only scenarios in which baseline HbA1c was set at 9.0% (75 mmol/mol) or 11.0% (97 mmol/mol) and target HbA1c was set at 7.0% (53 mmol/mol) are presented here; results for all other scenarios and additional information on HbA1c progression are reported in the Supplementary Material. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Cohort Characteristics
Baseline cohort characteristics were primarily sourced from a US-based population of patients newly diagnosed with type 2 diabetes published by Hillier and Pedula [17] (Table 2) supplemented where necessary with data from other published sources (see Supplementary Material) [18,19,20]. The mean (standard deviation) age of the simulated patient cohort was 53.0 (10.6) years and mean duration of disease was assumed to be 0 (0) years as patients were newly diagnosed. For parameters where baseline data were not available, CDM default values were used. Physiological risk factors other than HbA1c (e.g., lipid levels, systolic blood pressure) were assumed to remain constant over time to enable the comparison of different HbA1c targets and baseline levels.
Costs and Other Model Settings
Direct costs for diabetes-related complications were derived from published sources and, where necessary, inflated to 2018 USD using the US consumer price index specific to medical care in US cities (see Supplementary Material for full details of complication costs) [21]. The analysis was performed from the societal perspective (i.e., including both direct and indirect costs), and indirect costs associated with lost productivity were calculated using the human capital approach based on estimates of days off work due to complications published by Sørensen and Ploug [22], combined with median salary estimates published by the Bureau of Labor Statistics [23]. Acquisition costs associated with glucose-lowering therapy were not included in the analysis. Future costs and clinical outcomes were discounted at 3.0% per annum in line with recommendations for the US setting [24].
Population-Level Burden
The burden associated with poor glycemic control was estimated on a national level using a prevalence-based approach. The prevalent population of patients with type 2 diabetes was estimated on the basis of figures published by the CDC (30.3 million cases of diabetes in 2015) [1], together with the assumption that 90% of the overall diabetes population have type 2 diabetes [25]. Results from the NHANES indicate that only about 50% of American adults with diabetes are achieving HbA1c targets < 7.0% (< 53 mmol/mol), with data collected between 2011 and 2014 indicating that 50.9% of patients with type 2 diabetes reached this goal [5, 26]. For the estimation of population burden in all HbA1c scenarios in the present analysis, it was therefore assumed that 49.1% of patients in the overall type 2 diabetes cohort (i.e., 13,389,570 patients) had poor glycemic control (this was defined as HbA1c ≥ 7.0% [53 mmol/mol] in the NHANES analysis) and did not intensify therapy in the first year of treatment.
Results
Population-Level Burden
Modeling projections showed that failure to intensify therapy in a timely manner had a substantial impact on the economic burden associated with type 2 diabetes (Tables 3 and 4). Assuming a mean baseline HbA1c of 9.0% (75 mmol/mol) in the population, a 1-year delay in intensification could cost 13,390 years of life, increase the cost of diabetes-related complications by USD 1.8 billion, and add USD 5.6 billion to lost workplace productivity costs in just 1 year (Table 3). This corresponded to a total economic burden of USD 7.3 billion. Increasing delays in intensification and longer time horizons were associated with increasingly higher estimates of additional clinical and economic burden. This was evidenced in the scenario assuming a 7-year delay in intensification and a time horizon of 30 years: almost 3 million life-years were projected to be lost in the type 2 diabetes population, the cost of diabetes-related complications was increased by approximately USD 82.6 billion, and the additional costs associated with lost workplace productivity were estimated at USD 140.7 billion, resulting in a total cost burden of USD 223.3 billion.
Assuming poorer glycemic control in the population at baseline (mean HbA1c 11.0% [97 mmol/mol]), model projections showed that delayed intensification of therapy was associated with an even greater economic burden (Table 4). With the higher baseline HbA1c, a 1-year delay in intensification was projected to increase the costs associated with diabetes-related complications by USD 4.4 billion and lost productivity costs by USD 14.3 billion, resulting in a total cost of approximately USD 18.7 billion over the course of only 1 year. Modeling scenarios with longer time horizons and longer delays in intensification of therapy were associated with an even greater clinical and economic burden. In a population with a mean baseline HbA1c of 11.0% (97 mmol/mol), a 7-year delay in intensification was associated with a loss of 7,873,067 life-years over a 30-year time horizon. During this period, the time in poor glycemic control increased the cost of complications by approximately USD 209.7 billion and lost productivity costs went up by USD 338.4 billion, leading to a total increase in the economic burden of USD 548.2 billion.
Cost Savings per Patient
Consistent with the population level, patient-level results showed an increasing economic burden as delays in intensification lengthened and the time horizon increased (Tables 5 and 6). For patients with a baseline HbA1c of 9.0% (75 mmol/mol), a 1-year delay in intensification was associated with increased costs due to diabetes-related complications (USD 131) and lost productivity (USD 415), leading to an increase in total costs of USD 546 over a 1-year time horizon (Table 5). Longer delays in intensification led to substantially greater cost increases. For example, assuming a 7-year delay and a 30-year time horizon, poor glycemic control was projected to increase complication costs by USD 6172 and lost productivity costs by USD 10,507, making a total of USD 16,679 per patient. In this scenario, poor glycemic control was associated with a reduction in life expectancy of approximately 0.22 years per patient due to the increased risk of diabetes-related complications.
Patient-level burden was more pronounced in those with baseline HbA1c of 11.0% (97 mmol/mol). Projections showed that a 1-year delay in intensification increased total costs by approximately USD 1396 per patient over a 1-year time horizon, with approximately USD 327 of the total due to complication costs and USD 1070 due to lost productivity costs (Table 6). The greatest increase in patient-level burden was observed with a 7-year delay in intensification and a 30-year time horizon. In this modeling scenario, poor glycemic control increased complication costs by USD 15,663 and lost productivity costs by USD 25,277, resulting in a total of USD 40,940 per patient. As well as substantially increased costs, life expectancy was reduced by 0.59 years per patient due to poor glycemic control in this scenario.
Discussion
Therapeutic inertia has been defined as a failure on the part of healthcare provider to initiate or intensify therapy when needed [27] and has been shown to exist at all stages of the diabetes treatment paradigm, although therapeutic inertia toward the initiation of insulin is particularly pronounced [6, 28,29,30]. This is one of the first analyses to provide US-specific quantitative estimates of the economic implications of delayed treatment intensification due to therapeutic inertia on both an individual patient and population level. Specifically, over a time horizon of just 1 year and assuming a baseline HbA1c of 9.0% (75 mmol/mol), a 1-year delay in treatment intensification was associated with an additional economic burden of USD 7.3 billion, including USD 1.8 billion due to diabetes-related complications. These population estimates are based on reports of the prevalent population of type 2 diabetes patients in 2017. In the USA, the absolute number of people living with type 2 diabetes is projected to almost double by 2030, meaning that the economic burden associated with delayed treatment intensification is likely to increase considerably over the next decade.
Alongside the economic burden, the clinical implications of delayed treatment intensification are also considerable. A 1-year delay in intensification from 9.0% to a target of 7.0% was projected to cost the population 642,699 years of life over a 30-year time horizon. The impact of poor glycemic control projected here is, on an individual patient level, aligned with data reported previously. For example, in a UK-based analysis, Paul et al. [31] reported that for patients with HbA1c ≥ 7.0% (53 mmol/mol) (versus < 7.0%) a 1-year delay in treatment intensification was associated with a 67% increase in the risk of myocardial infarction and a 51% increase in the risk of stroke. Similarly, a 2017 modeling analysis, conducted using the Archimedes model, also reported a higher incidence of complications with delayed intensification [32].
In the present analysis, the consequences of intensification delays ranging from 1 to 7 years were explored, which is in line with those reported in routine clinical practice. In one UK-based analysis, the median time to intensification for patients on one, two, or three oral antidiabetes drugs (OADs) at baseline was 7.1, 6.1, and 6.0 years, respectively, and the mean HbA1c at the time of intensification was 8.7% (72 mmol/mol), 9.1% (76 mol/mol), and 9.7% (83 mmol/mol), respectively [29]. In a second UK-based study, Khunti et al. [30] reported that among insulin-treated patients with poor glycemic control (defined as HbA1c ≥ 7.5% [58 mmol/mol]) who did undergo treatment intensification, the median time to intensification was 3.7 years and mean HbA1c at intensification was > 9.0% (75 mmol/mol). Additionally, it should be noted that the time frame of most clinical studies examining delays in intensification is such that, typically, only a short temporal window in the overall treatment paradigm is included in the analysis. As type 2 diabetes is a progressive disease, therapy has to be routinely intensified multiple times over a patient’s lifetime to maintain good glycemic control and mitigate the risk of diabetes-related complications. There may well be intensification delays at each stage, meaning that the cumulative time spent in poor glycemic control may be longer than that reported in individual studies [33]. The cumulative time spent with poor glycemic control was examined in a US-based analysis by Brown et al. [34], who estimated that even in a well-controlled population, OAD-treated patients spent a mean time of almost 5 years with HbA1c > 8.0% (64 mol/mol) prior to insulin initiation. Notably, this analysis was limited to patients treated with OADs and does not capture potential further cumulative time spent in poor glycemic control associated with any delays in intensification of therapy once patients initiated insulin.
The present analysis uses HbA1c targets that are aligned with previously published recommendations, e.g., the ADA targets of 6.5% (48 mmol/mol), 7.0% (53 mmol/mol), and 8.0% (64 mmol/mol) selected according to individual patient characteristics [15]. In the most recent consensus report by the ADA and the European Association for the Study of Diabetes (EASD), the focus is on individual targets for each patient, stating that a “reasonable HbA1c target for most non-pregnant adults with sufficient life expectancy to see microvascular benefits (generally ~ 10 years) is around 53 mmol/mol (7%) or less”, and noting that targets should be individualized on the basis of patient preferences, treatment goals, and the risk of adverse effects of therapy [4]. While therapy targets are moving away from fixed HbA1c goals at the individual patient level, the use of such threshold values at a population level is still helpful in terms of understanding the benefits of new therapies in a given population, and for quantifying the burden of poor glycemic control. Moreover, the approach of using glycemic control thresholds for a population is aligned with previous publications on therapeutic inertia [26, 27, 34].
Therapeutic inertia may arise at the patient, physician, or healthcare system level, or may be multifactorial emanating at a number of different levels. Barriers to treatment intensification at the patient level include a reluctance to initiate injectable therapies, poor health literacy, increased costs, unwillingness to undertake a more complex regimen, and fear of weight gain with insulin. At the physician level, fears over hypoglycemia have been documented specifically with regard to insulin initiation or intensification. Additionally, therapeutic inertia in relation to the initiation of insulin has been reported to be more common in primary care than for patients treated by secondary care specialists [35]. Moreover, a number of studies have reported similar therapeutic inertia in patients receiving OADs, suggesting that therapeutic inertia can lead to poor glycemic control across the treatment continuum [33]. Concern over increasingly complex regimens negatively influencing adherence has also been reported to contribute to therapeutic inertia at the physician level [36, 37]. The present analysis has shown that treatment delays of even 1 year, and the resultant time spent with poor glycemic control, are associated with substantial clinical and economic consequences. As such, initiatives aimed at overcoming therapeutic inertia both at the patient and physician level are likely to play an important role in combating the increasing burden of disease associated with type 2 diabetes. Initiatives that have been documented as helping overcome therapeutic inertia include patient education programs, simplifying treatment or titration regimens, and the inception of nurse practitioner-led diabetes care, with frequent follow-up allowing for the establishment of good patient–healthcare provider relationships and continuity of care as well as reassurance and assistance with issues such as timing and dosing of new therapies, management of treatment-related adverse events, and titration of insulin [36]. In a recent review, Okemah et al. [38] noted that therapeutic inertia results from healthcare provider-, patient-, and healthcare system-based factors, and represents a serious barrier to optimal treatment escalation and, as a result, glycemic control. The complex nature of inertia means that addressing it requires a combinatorial approach. The authors cited evidence supporting the role of patient education and involvement, personalizing therapy, patient feedback, education of healthcare providers and use of clinical decision support tools to reduce therapeutic inertia and improve outcomes for patients with type 2 diabetes.
The present study is associated with a number of limitations. Only costs associated with long-term diabetes-related complications were considered in the analysis. Costs associated with treatment (OADs and insulin) were not considered. Additionally, the clinical focus of the analysis was limited to HbA1c alone. Although there may be covariance between HbA1c and other physiological risk factors (such as lipid levels and systolic blood pressure) and management of these risk factors is an integral component of diabetes management, HbA1c was the only risk factor captured in the analysis. While this may present an overly simplistic picture of disease management, the rationale for this was that it permitted a focused analysis of HbA1c alone. The costs and quality of life deficits associated with hypoglycemic events were also not included in the current analysis. For patients with problematic hypoglycemic events, individualized HbA1c targets may be above the 7.0% (53 mmol/mol) threshold used here. The omission of hypoglycemic events should be noted when considering findings, particularly on an individual patient level. Allied to this, it should be noted that on an individual patient level, there are other circumstances in which physicians may tolerate poor glycemic control or set HbA1c target levels above 7.0% (53 mmol/mol); these may include instances where the patient has limited life expectancy or cases where multiple serious comorbid conditions are present.
Conclusion
The present health economic analysis has provided evidence that therapeutic inertia resulting in prolonged periods of time spent with poor glycemic control is likely to be associated with a substantial clinical and economic burden. Available clinical evidence has shown that achieving and maintaining good glycemic control is a crucial component of diabetes management in terms of delaying or preventing long-term diabetes-related complications. Initiatives that combat therapeutic inertia at the physician, patient, and health service level may help avert the clinical and economic consequences associated with unnecessary delays in intensification of treatment.
References
United States Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Statistics Report 2017. https://dev.diabetes.org/sites/default/files/2019-06/cdc-statistics-report-2017.pdf Accessed 16 Aug 2019.
Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: insights from yesterday, today, and future trends. Popul Health Manag. 2017;20(1):6–12.
American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care. 2018;41(5):917–28.
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Carls G, Huynh J, Tuttle E, Yee J, Edelman SV. Achievement of glycated hemoglobin goals in the US remains unchanged through 2014. Diabetes Ther. 2017;8(4):863–73.
Pantalone KM, Misra-Hebert AD, Hobbs TM, et al. Clinical inertia in type 2 diabetes management: evidence from a large, real-world data set. Diabetes Care. 2018;41(7):e113–4.
Khunti K, Millar-Jones D. Clinical inertia to insulin initiation and intensification in the UK: a focused literature review. Prim Care Diabetes. 2017;11(1):3–12.
Mocarski M, Yeaw J, Divino V, et al. Slow titration and delayed intensification of basal insulin among patients with type 2 diabetes. J Manag Care Spec Pharm. 2018;24(4):390–400.
Palmer AJ, Roze S, Valentine WJ, et al. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5–26.
Palmer AJ, Roze S, Valentine WJ, et al. Validation of the CORE Diabetes Model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(Suppl 1):S27–40.
McEwan P, Foos V, Palmer JL, Lamotte M, Lloyd A, Grant D. Validation of the IMS CORE Diabetes Model. Value Health. 2014;17(6):714–24.
Clarke PM, Gray AM, Briggs A, et al. UK Prospective Diabetes Study (UKDPS) Group. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia. 2004;47(10):1747–59.
World Health Organization. Global Health Observatory data repository: life tables by country (United Kingdom). 2019. http://apps.who.int/gho/data/view.main.61780?lang=en. Accessed 16 Aug 2019.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2017 executive summary. Endocr Pract. 2017;23(1):207–38.
American Diabetes Association. Glycemic targets. Diabetes Care. 2017;40(Suppl 1):s48–56.
National Committee for Quality Assurance (NCQA). HEDIS measures and technical resources. 2018. https://www.ncqa.org/hedis/measures/. Accessed 21 Nov 2019.
Hillier TA, Pedula KL. Characteristics of an adult population with newly diagnosed type 2 diabetes: the relation of obesity and age of onset. Diabetes Care. 2001;24(9):1522–7.
National Institute for Health and Care Excellence (NICE). NICE guideline [NG28]. Type 2 diabetes in adults: management. Appendix F, Table 20, pages 45/46. 2017. https://www.nice.org.uk/guidance/NG28/documents/type-2-diabetes-appendix-f. Accessed 14 May 2019.
Humes KR, Jones NA, Ramirez RR. Overview and race and Hispanic origin. 2010. https://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed 19 Aug 2019.
Pratley RE, Nauck M, Bailey T, et al. Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet. 2010;375(9724):1447–56 (Erratum in: Lancet. 2010; 76(9737):234).
United States Department of Labor. CPI-All urban consumers. Medical care in US city average, all urban consumers, not seasonally adjusted. https://beta.bls.gov/dataViewer/view/timeseries/CUUR0000SAM. Accessed 19 Aug 2019.
Sørensen J, Ploug UJ. The cost of diabetes-related complications: registry-based analysis of days absent from work. Econ Res Int. 2013; Article ID 618039:1–8.
Bureau of Labor Statistics. News release usual weekly earnings of wage and salary workers second quarter. 2019. https://www.bls.gov/news.release/pdf/wkyeng.pdf. Accessed 19 Aug 2019.
Gold M. Panel on cost-effectiveness in health and medicine. Med Care. 1996;34(12 Suppl):DS197-99.
Diabetes.org.uk. Facts and figures. https://www.diabetes.org.uk/professionals/position-statements-reports/statistics. Accessed 19 Aug 2019.
Edelman SV, Polonsky WH. Type 2 diabetes in the real world: the elusive nature of glycemic control. Diabetes Care. 2017;40(11):1425–32.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Int Med. 2001;135(9):825–34.
Fu AZ, Sheehan JJ. Treatment intensification for patients with type 2 diabetes and poor glycaemic control. Diabetes Obes Metab. 2016;18(9):892–8.
Khunti K, Wolden ML, Thorsted BL, Andersen M, Davies MJ. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care. 2013;36(11):3411–7.
Khunti K, Nikolajsen A, Thorsted BL, Andersen M, Davies MJ, Paul SK. Clinical inertia with regard to intensifying therapy in people with type 2 diabetes treated with basal insulin. Diabetes Obes Metab. 2016;18(4):401–9.
Paul SK, Klein K, Thorsted BL, Wolden ML, Khunti K. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14:100.
Folse HJ, Mukherjee J, Sheehan JJ, et al. Delays in treatment intensification with oral antidiabetic drugs and risk of microvascular and macrovascular events in patients with poor glycaemic control: an individual patient simulation study. Diabetes Obes Metab. 2017;19(7):1006–13.
Khunti S, Davies MJ, Khunti K. Clinical inertia in the management of type 2 diabetes mellitus: a focused literature review. Br J Diabetes Vasc Dis. 2015;15(2):65–9.
Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Diabetes Care. 2004;27(7):1535–40.
Shah BR, Hux JE, Laupacis A, Zinman B, van Walraven C. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Diabetes Care. 2005;28(3):600–6.
Russell-Jones D, Pouwer F, Khunti K. Identification of barriers to insulin therapy and approaches to overcoming them. Diabetes Obes Metab. 2018;20(3):488–96.
Santos Cavaiola T, Kiriakov Y, Reid T. Primary care management of patients with type 2 diabetes: overcoming inertia and advancing therapy with the use of injectables. Clin Ther. 2019;41(2):352–67.
Okemah J, Peng J, Quiñones M. Addressing clinical inertia in type 2 diabetes mellitus: a review. Adv Ther. 2018;35(11):1735–45.
Acknowledgements
The authors are grateful to Laura Rizkallah (Novo Nordisk A/S, Søborg, Denmark) for valuable input regarding the interpretation of results and critical review of the manuscript.
Funding
This study and the journal’s Rapid Service and Open Access Fees were supported by funding from Novo Nordisk A/S, Søborg, Denmark. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sarah Naz Ali is an employee of Novo Nordisk Inc. Tam Dang-Tan is an employee and Shareholder of Novo Nordisk Inc. William J Valentine is an employee of Ossian Health Economics and Communications GmbH, Basel, Switzerland, which has received financial support from Novo Nordisk A/S to conduct the analysis described in this paper. Brian Bekker Hansen is an employee and shareholder of Novo Nordisk A/S.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
All results and key data inputs for the modeling analysis are provided in the Supplementary Material.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11341625.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ali, S.N., Dang-Tan, T., Valentine, W.J. et al. Evaluation of the Clinical and Economic Burden of Poor Glycemic Control Associated with Therapeutic Inertia in Patients with Type 2 Diabetes in the United States. Adv Ther 37, 869–882 (2020). https://doi.org/10.1007/s12325-019-01199-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01199-8