Abstract
Introduction
MET exon 14 skipping in patients with advanced non-small cell lung cancer (aNSCLC), can be targeted with MET inhibitors including tepotinib, capmatinib, savolitinib, and crizotinib. Matching-adjusted indirect comparison (MAIC) methodology was used to compare outcomes data between agents and to address bias from differences in baseline characteristics.
Methods
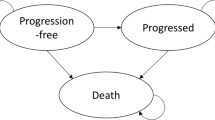
Patient-level data from the VISION study (tepotinib) were weighted for comparison with aggregate data from the GEOMETRY mono-1 (capmatinib), NCT02897479 (savolitinib) and PROFILE 1001 (crizotinib) studies in patients with aNSCLC, using baseline characteristics prognostic for overall survival (OS) in VISION. Overall response rate (ORR), OS, progression-free survival (PFS), and duration of response (DOR) were compared. Patients were stratified by line of therapy: overall (all lines), previously treated, and treatment-naïve.
Results
Improvements in ORR and all time-to-event endpoints were predicted for tepotinib compared with crizotinib and savolitinib in the different populations, although comparisons with savolitinib were hindered by considerable differences in baseline patient populations. Tepotinib appeared to be associated with prolonged PFS and OS compared with capmatinib in previously treated patients (PFS HR 0.54; 95% CI 0.36–0.83; OS HR 0.66; 95% CI 0.42–1.06) and the overall populations (PFS HR 0.60; 95% CI 0.43–0.86; OS HR 0.72; 95% CI 0.49–1.05), with smaller improvements in DOR. The ORR comparisons between tepotinib and capmatinib identified a swing of up to ± 6 percentage points in the weighted tepotinib ORR depending on the population studied (treatment-naïve vs. previously treated patients).
Conclusions
The MAIC identified potential differences in efficacy endpoints with the different MET inhibitors, and predicted prolonged PFS and OS with tepotinib compared with capmatinib and crizotinib. Although MAIC cannot balance for unobserved factors, it remains an informative method to contextualize single-arm studies, where head-to-head trials are unlikely to be feasible.
Similar content being viewed by others
Why carry out this study? |
There are several MET-targeted tyrosine kinase inhibitors clinically available for the treatment of METex14 skipping non-small cell lung cancer (NSCLC), but no head-to-head comparative studies have been conducted |
What was learned from the study? |
This Matching-adjusted indirect comparison (MAIC) provides a sound scientific basis for indirect comparisons of available MET inhibitors based on the tepotinib VISION study, in contrast to naïve side-by-side comparisons of study data |
ORR estimates for tepotinib varied by up to ± 6 percentage points when adjusted for baseline characteristics of the capmatinib GEOMETRY mono-1 study population, illustrating the impact of the investigated study population in single-arm studies |
The indirect comparisons confirmed the benefits of tepotinib compared with other MET inhibitors in previously treated patients, and showed comparability of effects with capmatinib in treatment-naïve patients |
Introduction
MET exon 14 skipping (METex14) is an oncogenic driver occurring in 3–4% of patients with non-small cell lung cancer (NSCLC), which has been successfully targeted using the selective MET inhibitors tepotinib, capmatinib, and savolitinib in the phase 2, single-arm VISION (NCT02864992) [1], GEOMETRY mono-1 (NCT02414139) [2], and 2016-504-00CH1 (NCT02897479) [3] studies, respectively. Both tepotinib [4] and capmatinib [5] received accelerated approval from the US Food and Drug Administration (FDA) for the treatment of METex14 metastatic NSCLC, based on data from these studies. Savolitinib was approved in China for patients with METex14 NSCLC following progression on (or inability to tolerate) platinum-based chemotherapy [6, 7]. Crizotinib is a multikinase inhibitor which is approved for ALK- and ROS1-altered NSCLC, but also has clinical results in METex14 NSCLC (PROFILE 1001; NCT00585195), and is referred to in international guidelines [8, 9]. These agents are currently the only MET TKIs recommended or licensed for the treatment of METex14 skipping NSCLC [10].
The majority of evidence for the utility of therapies in METex14 NSCLC is from single-arm phase 1 and 2 trials. However, side-by-side comparison of data from different studies is prone to bias, resulting from differences in patient populations from different studies. To allow meaningful comparative insights, a method is needed to provide a robust comparison of data from these studies, which is capable of addressing the potential biases resulting from these differences. Matching-adjusted indirect comparison (MAIC) [11] is a pairwise indirect comparison method intended to provide a more accurate comparison of trial data by compensating for between-trial differences in patient characteristics [12]; patient-level data for one trial are weighted to make them more comparable with the population of a second trial. Endpoint data are then recalculated for the weighted study population and compared with the second trial to give a more balanced comparison than simply comparing data from different trials side-by-side. MAIC is an established comparative method that has been applied to conduct comparisons between immunotherapy-based anticancer therapies and ROS1-related targeted treatments for NSCLC [13,14,15].
Here, we compare efficacy data for all of the available MET inhibitors for the treatment of METex14 advanced NSCLC, via MAICs of data for tepotinib from the VISION study, weighted for comparison with capmatinib (GEOMETRY mono-1 study), savolitinib (NCT02897479), and crizotinib (PROFILE 1001 study).
Methods
Study Data
The VISION, GEOMETRY mono-1, NCT02897479, and PROFILE 1001 trials were used for indirect treatment comparison of tepotinib versus capmatinib, savolitinib, and crizotinib, respectively. Population-level data were available for patients with METex14 NSCLC from GEOMETRY mono-1, NCT02897479, and PROFILE 1001. Patient-level data were only available for the VISION study, provided by the study sponsor. To align with the eligibility criteria of the other trials by tissue biopsy only, the VISION population was limited to patients with METex14 NSCLC identified by tissue biopsy, as the VISION study permitted patient enrollment by either tissue or liquid biopsy. In GEOMETRY mono-1, liquid biopsy was included as a retrospective procedure in patients already enrolled to the study [2], and as a complementary detection method in PROFILE 1001 and NCT02897479 [16, 17].
VISION is a phase 2 single-arm study which included three patient cohorts: A (METex14 skipping NSCLC; primary analysis cohort), B (NSCLC with MET amplification) and C (confirmatory cohort for Cohort A). Data from VISION included 174 patients with METex14 NSCLC identified by tissue biopsy with ≥ 3 months’ follow-up, who received tepotinib 500 mg (450 mg active moiety) once daily, with a cut-off date of February 2021 [18, 19]. Patient populations for analysis were: (1) previously treated patients only (at least one prior systemic therapy for advanced or metastatic disease), (2) line-agnostic patients (any number of prior systemic therapies for advanced or metastatic disease, including no prior therapy), and (3) treatment-naïve patients (no prior therapies for advanced or metastatic disease).
Data for the comparator trials were taken from the most recent publications of aggregate data for which baseline characteristics data were available. For the analysis of time-to-event endpoints, Kaplan–Meier (KM) curves were mapped back to the original data using the algorithm of Guyot et al. [20], and reconstructed for comparison with naïve (unweighted) and weighted VISION patient-level data; the reconstructed comparator KM curves were compared with the original comparator KM curves, as an indicator of the validity of the reconstructed KM data. Where KM data were not available, a MAIC was performed using median outcome point estimates. Odds ratios were calculated for objective response rate (ORR) comparisons. Statistical analyses were performed using RStudio (2020) R 4.1.0.
GEOMETRY mono-1 is a multiple-cohort phase 2 study, which recruited patients with stage IIIb or IV NSCLC: Cohorts 1–3 (previously treated patients with various levels of MET amplification), Cohort 4 (previously treated patients with METex14 skipping), Cohort 5a (untreated patients with MET amplification), Cohort 5b (untreated patients with METex14 skipping), Cohort 6 (expansion cohort for previously treated patients with MET amplification or METex 14 skipping), and Cohort 7 (expansion cohort for untreated patients with METex14 skipping). GEOMETRY mono-1 data (capmatinib) were taken from publications for the various patient cohorts and data cuts from this study due to the availability of KM data, and different endpoints reported for different cohorts at different times (Table 1). For the treatment-naïve patients only comparison, the data cut-off of September 18, 2020 was used for overall survival (OS), duration of response (DOR), and ORR comparisons, with the January 6, 2020 data cut used for progression-free survival (PFS). For the previously treated patients only comparison, the September 18, 2020 data cut-off was used for OS and ORR, with the January 6, 2020 data cut-off for PFS and the April 15, 2019 data cut-off used for DOR [21]. Patients in the GEOMETRY mono-1 study received capmatinib 400 mg twice daily [2, 22]. As there were data reported for the original GEOMETRY mono-1 cohorts, and data combining the original cohort with an expansion cohort for both previously treated and treatment-naïve patients, we ran comparisons with both the larger expansion + original patient cohorts [‘Base case’ analyses; Cohorts 4 + 6 for previously treated patients (n = 100) and Cohorts 5b + 7 for treatment-naïve patients (n = 60)], and the original patient cohorts only [‘Sensitivity’ analyses; Cohort 4 for previously treated patients (n = 69) and Cohort 5b for treatment-naïve patients (n = 28)]. There was only one cohort used for the line-agnostic analysis (Cohorts 4 + 5b; n = 97).
Savolitinib data were taken from the 2021 publication of the NCT02897479 study, a single-arm phase 2 study, in which patients received savolitinib 600 mg (bodyweight ≥ 50 kg) or 400 mg (bodyweight < 50 kg) once daily, with a median follow-up of 17.6 months (data cut-off: August 3, 2020) [3]. More than 35% of patients enrolled in the NCT02897479 study had pulmonary sarcomatoid carcinoma (PSC), a rare histologic subtype that was less prevalent (< 10%) in the other studies, where adenocarcinoma was the predominant histology. PSC usually accounts for < 0.5% of all lung cancers, and is associated with different patient characteristics compared with other types of NSCLC [23, 24]. Therefore, to produce a meaningful comparison between the NCT02897479 and VISION studies, efficacy data reported for ‘other histologies’ in NCT02897479 was used, limiting the analysis to PFS, DOR, and ORR (Table 1).
Data for crizotinib were taken from the phase 1 PROFILE 1001 study, in which an expansion cohort of patients with advanced NSCLC harboring METex14 alterations received crizotinib 250 mg twice daily (Table 1) [16]. At the data cut-off date of January 31, 2018, this cohort included 69 patients with predominantly adenocarcinoma tumor histology (84%), but also a small proportion (9%) of patients with PSC histology.
Statistical Methods, Matching Variables and Outcomes Comparisons
Study data were compared using both unweighted naïve comparisons [where study data were modeled without weighting, with regression coefficients providing hazard ratio (HR) estimates with a two-sided 95% confidence interval (CI)] and as a MAIC, where the VISION population was weighted to match the relevant comparison study populations [11, 25]. A propensity score-type logistic regression equation was used to estimate weights to balance studies with respect to patient characteristics; this equation predicts whether a given type of patient originates from the index trial (VISION) or the comparator study as a function of baseline characteristics. The propensity score weights were constructed to match the VISION trial to the comparator trial based on proportions for categorical baseline characteristics and median for continuous baseline characteristics (e.g., age). A Cox regression analysis was performed to identify baseline variables that were prognostic of OS from the VISION study at the 5% significance level, to inform the weighting process.
OS, PFS, and DOR outcomes were compared between tepotinib and capmatinib for previously treated and treatment-naïve patients, and between tepotinib and all other MET inhibitors (capmatinib, savolitinib, and crizotinib) for treatment line-agnostic patients.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Variables for Baseline Characteristics Matching
The matching variables selected to weight data from VISION patients for the MAIC were those identified by the Cox regression analysis to have a significant association with OS (Table 2): age (median), race, Eastern Cooperative Oncology Group performance status (ECOG PS), histology, and smoking history (only the comparison between former vs. regular smokers was statistically significant). These variables were used where comparator data were available.
Table 3 shows the major areas of similarity and difference between VISION and the comparator studies, and Tables 4, 5 and 6 show the results of baseline population characteristic weighting for each of the outcome comparisons by line of treatment. In each case, the VISION population was successfully weighted to match the comparison population.
For the savolitinib comparison in line-agnostic patients (Table 5), only Asian patients in VISION were selected for weighting (all patients in the NCT02897479 study were enrolled from China), to minimize race as a weighting factor. Smoking history was not included as a factor because it was reported only as smoker versus non-smoker in NCT02897479, and only the former smoker versus regular smoker status had a significant prognostic impact in VISION (Table 2).
Previously Treated Patients Only
The odds ratio for the MAIC ORR comparison between tepotinib and capmatinib in previously treated patients only was in favor of capmatinib in the Base case analysis, and tepotinib in the Sensitivity analysis. These odds ratios were accompanied by wide, overlapping 95% CIs of 0.59–1.95 and 0.45–1.69, respectively (Table 7), indicating that, overall, neither agent was likely to be superior to the other.
Point-estimate comparisons of median PFS for tepotinib with capmatinib (Base case analysis) in previously treated patients only suggested a marked increase in median PFS with tepotinib (11.0 months and 5.5 months, respectively), without overlap of 95% CIs for the estimates. However, the estimates of median DOR were similar (9.7 and 11.1 months for capmatinib and tepotinib, respectively) (Table 8).
Naïve and MAIC KM comparisons of PFS and OS data from previously treated patients only who received tepotinib and capmatinib (sensitivity analysis) are shown in Fig. 1. The KM curves for the naïve and MAIC tepotinib populations showed a large degree of overlap, and notable separation from the capmatinib KM curve in favor of tepotinib, up to around 24 months (PFS) and 21 months (OS).
Line-Agnostic Patients
The odds ratio for ORR for the comparison of tepotinib with capmatinib was close to 1 for both the naïve and MAIC comparisons, indicating no difference between agents. The ORR for tepotinib was considerably higher than savolitinib and crizotinib in the MAICs (56.9% vs. 44.4% for tepotinib and savolitinib, respectively, and 52.7% vs. 32.3% for tepotinib and crizotinib, respectively), with similar trends in the naïve comparisons (Table 7). Accordingly, the odds ratios for these comparisons both favored tepotinib. Although the 95% CI of the odds ratio for the savolitinib comparison included 1, there were difficulties with weighting for this analysis (see below), which may have resulted in wide confidence intervals. Overall, these data indicate a probable improvement in ORR for tepotinib compared with either savolitinib or crizotinib.
PFS, OS, and DOR KM comparisons between tepotinib and capmatinib (Base case analysis; Fig. 2) for line-agnostic patients showed a similar pattern to that for previously treated patients only, with overlapping curves for the tepotinib naïve and MAIC analyses, and marked separation from the capmatinib survival curves. There was a higher degree of separation between the capmatinib and tepotinib curves for PFS and OS than for DOR, with 95% CIs for both the naïve and MAIC analyses being < 1 for PFS [naïve HR 0.57 (95% CI 0.41–0.79); MAIC HR 0.60 (95% CI 0.43–0.86)]. These predicted trends indicate prolonged survival with tepotinib compared with capmatinib across all lines of treatment.
Time-to-event endpoint comparisons for line-agnostic patients: tepotinib versus capmatinib (Cohort 4 and 5b). A PFS (IRC-assessed data), B OS, and C DOR (IRC-assessed data). Footnote for Weighted tepotinib VISION: unscaled weights. DOR duration of response, HR hazard ratio, IRC independent review committee, MAIC matching-adjusted indirect comparison, PFS progression-free survival, OS overall survival
Reconstruction of the KM curve for PFS with savolitinib was unsuccessful, and therefore all time-to-event comparisons relied on point estimates (Table 8). In the comparisons for PFS and DOR, estimated median values for both endpoints were slightly higher for tepotinib than for savolitinib in the MAIC, although full 95% CI could not be calculated; median point estimates were not evaluable for tepotinib in the naïve comparison.
The PFS KM curve comparison between tepotinib and crizotinib again showed considerable overlap between the naïve and MAIC analyses for tepotinib, and separation of both from the curve for crizotinib, with longer PFS suggested for tepotinib [HR 0.50 (95% CI 0.32–0.76); Fig. 3]. In the point-estimate OS and DOR comparisons of tepotinib with crizotinib (Table 8), predicted median OS was slightly longer with tepotinib than crizotinib (median 22.3 months vs. median 20.5 months, respectively) but predicted median DOR was considerably longer with tepotinib (median 15.4 months vs. 9.1 months, respectively).
Treatment-Naïve Patients
In both the Base case and Sensitivity analyses for treatment-naïve patients, ORR with capmatinib was considerably higher than those calculated for tepotinib (66.7–67.9% vs. 54.7–60.7%, respectively; Table 7). Notably, the MAIC ORR values for tepotinib in treatment-naïve patients considerably increased compared with the unweighted naïve ORRs, with a difference of 6 percentage points in the Base case analysis. This increase was higher than for any of the other analyses, and indicates that weighting the treatment-naïve tepotinib population to match the treatment-naïve capmatinib population selected for patients more likely to respond to treatment. Furthermore, the odds ratios for the treatment-naïve ORR comparisons were not significant, based on wide 95% CIs.
The KM curves for PFS and OS for treatment-naïve patients with tepotinib and capmatinib (Sensitivity analysis; Fig. 4) overlapped for both endpoints and did not suggest differences between them. However, the point estimate of DOR showed a considerable difference between tepotinib (median 32.7 months) and capmatinib (median 12.6 months) in the Base case analysis, which was repeated in the Sensitivity analysis (Table 8), although the full 95% CI ranges were not estimable.
Time-to-event endpoint comparisons for treatment-naïve patients: tepotinib versus capmatinib (Cohort 5b). A PFS (IRC-assessed data) and B OS. Footnote for Weighted tepotinib VISION: unscaled weights. HR hazard ratio, IRC independent review committee, MAIC matching-adjusted indirect comparison, PFS progression-free survival, OS overall survival
Discussion
Comparing outcomes between discrete single-arm trials is not a straightforward task, but it is necessary in the setting of uncommon cancers, such as METex14 skipping NSCLC, for which such trials are the only available data source. Straightforward side-by-side outcomes data have been published [26,27,28], but are prone to bias, resulting from differences in outcome measure definitions, study designs, assessment time, and patient characteristics of the study populations. Consequently, any conclusions drawn from direct side-by-side presentations of raw study data are limited, and may be inappropriate. Hence, the utility of the MAIC method, which is capable of mitigating patient population bias by weighting data from one trial to more closely resemble another, provides a more balanced comparison of outcomes.
Weighting in our MAIC analyses was performed using baseline characteristics identified as prognostic for OS in the VISION study. In general, there was a high degree of consistency between the unweighted naïve comparison and MAIC time-to-event endpoints for tepotinib across the comparisons with other agents. However, for the ORR comparisons with capmatinib, weighting of the tepotinib data to resemble the capmatinib population for the MAIC increased the tepotinib ORR by 6 percentage points (Base case analysis) in treatment-naïve patients, and decreased the tepotinib ORR by 5.3 percentage points (Base case analysis) in the previously treated patients only population. This considerable swing in effect on the tepotinib ORR between first- and later-line patients suggests either that the treatment-naïve population in GEOMETRY mono-1 experienced an exceptionally good response to treatment, or that the selected weighting characteristics did not include some clinically significant factor that was better represented in treatment-naïve patients in GEOMETRY mono-1 than in previously treated patients, or patients in the VISION study. Table 6 shows that, compared with the treatment-naïve population in GEOMETRY mono-1, the treatment-naïve population in VISION contained more Asian patients, more former smokers and fewer never-smokers, fewer patients with adenocarcinoma histology and more patients with ‘other’ histologies, and more patients with ECOG PS 0. In the line-agnostic and previously treated patients only populations (Tables 4, 5), differences in race and smoking history are still visible, but differences in ECOG PS and histology are much less prominent. Hence, there were differences in baseline characteristics for the treatment-naïve populations between VISION and GEOMETRY mono-1 that were more evenly distributed across the overall study populations.
The comparisons for previously treated patients only were limited to capmatinib, and suggested an improvement in PFS (HR 0.54; 95% CI 0.36–0.83) and OS (HR 0.66; 95% CI 0.42–1.06) in favor of tepotinib, with no consistent difference in ORR identified between the two agents.
Data for line-agnostic patients were available for comparisons between tepotinib and all three of the other MET inhibitors. ORR was predicted to be higher with tepotinib than savolitinib or crizotinib in the MAICs, but there were no major differences between tepotinib and capmatinib. However, the MAICs with capmatinib suggested improved PFS with tepotinib (HR 0.6; 95% CI 0.43–0.86).
The comparisons with savolitinib were complicated by a failure to accurately re-map the published KM curve, leading to a reliance on point-estimate comparisons, where a small increase in median PFS with tepotinib was suggested (9.6 vs. 6.9 months). This difficulty reflects the problems encountered with making a robust comparison between the savolitinib and tepotinib datasets. Fundamental differences in the histology and ethnic composition of the patient populations reduced the number of patients available for comparison, and hence the likelihood of finding meaningful differences. Further evidence of the fundamental differences between the savolitinib dataset and data for the other agents can be seen in the tepotinib ORR calculated for the naïve comparisons; for comparison with capmatinib and crizotinib, the ORR calculated for tepotinib was 51.1% in both cases, but was considerably higher for the comparison with savolitinib (57.9%). The comparisons with crizotinib predicted improvements with tepotinib for ORR (odds ratio 0.43; 95% CI 0.23–0.79) and PFS (HR 0.50; 95% CI 0.32–0.76).
Time-to-event comparisons in treatment-naïve patients were limited to capmatinib, and did not suggest meaningful differences for any of the time-to-event endpoints. Although ORR estimates appeared to favor capmatinib, ORR for both were ≥ 60%. The MAIC estimate for median DOR with tepotinib was more than twice that with capmatinib, where median DOR could be estimated [32.7 (95% CI 10.8–ne) vs. 12.6 (95% CI 5.6–ne) months], although this difference may decrease with further data maturity.
The major limitations of the MAIC process relate to the availability of data and fundamental comparability of patient populations. Ideally, patient-level data from all of the included studies would be used for the MAIC. However, the only patient-level data available to us was from the VISION study, and our MAIC was restricted to retrospective data in the public domain. Population weighting can only accommodate basic differences in population datasets to a certain extent. For example, the savolitinib comparisons were highly restricted by patient populations in terms of race and histology, which could not be completely addressed via population weighting. Hence, these comparisons could be considered less robust than those for the other agents. The general limitations of indirect comparisons are also relevant, including potential bias resulting from different assessment times between studies and comparability of endpoints used. In addition to the small sample sizes, certain confounding factors could not be corrected for, such as the effect of post-study treatment on OS, differences in follow-up times for the different data cuts used (which was dependent on the various available publications), and the influence of unobserved factors (which could not be mitigated outside of a randomized trial). The included studies had comparable inclusion and exclusion criteria for recruitment and were performed during similar time periods (which may otherwise have affected METex14 detection methods), and for VISION, patient selection was restricted to identification by tissue biopsy only for consistency with comparator studies. However, as these considerations could not mitigate all residual confounding factors, our results must be interpreted cautiously. Regarding the agents studied, it is important to note that crizotinib is a type 1a MET inhibitor, whereas the other agents are type 1b inhibitors. While both types are ATP-competitive, they have different binding characteristics which may affect their pharmacologic activity [29].
Further data with greater maturity are anticipated for all the investigated studies. As more single-arm datasets become available, the use of comparison methods such as MAIC will become increasingly important to provide indirect cross-trial comparisons to help to inform clinicians and patients.
MAIC is becoming established as an accepted and reliable method for cross-trial comparison where head-to-head trials are not available; in recent years, MAICs have been used to support clinical benefit across various endpoints in oncology [13,14,15]. For example, a MAIC was performed to compare data from the KEYNOTE-021 and KEYNOTE-189 studies, which both included patients with non-squamous NSCLC who received first-line pembrolizumab + pemetrexed + platinum chemotherapy, with patients who received atezolizumab + carboplatin + (nab-)paclitaxel ± bevacizumab in the IMpower 130 and IMpower 150 trials. By weighting patient-level data from the KEYNOTE studies for comparison with aggregate data from the IMpower studies, significant OS (HR 0.80; 95% CI 0.67–0.95) and PFS (HR 0.79; 95% CI 0.67–0.93) benefits were demonstrated for the pembrolizumab-based regimens with the atezolizumab-based regimens [13]. Similar methodology was used in a separate MAIC between patients with metastatic NSCLC who received pembrolizumab + chemotherapy in the KEYNOTE-021G, KEYNOTE-189, and KEYNOTE-407 studies, and patients who received nivolumab + ipilimumab in the CheckMate 227 Part 1A study. Here, the MAIC suggested greater clinical benefit in terms of OS (HR 0.80; 95% CI 0.59–1.09), ORR (25.5% risk reduction), and PFS (HR 0.53; 95% CI 0.41–0.68) for pembrolizumab + chemotherapy than with nivolumab + ipilimumab in patients with programmed death-ligand 1 ≥ 1% [15]. Lastly, MAIC methodology was used to identify better responses to entrectinib versus crizotinib in patients with ROS1 fusion-positive NSCLC, using data collected via a systematic literature review. The MAIC suggested significantly better ORR with entrectinib versus crizotinib across a range of scenarios for proportion of patients with central nervous system metastases (odds ratio 2.43–2.74), increased OS (HR 0.47–0.61), and lower levels of adverse event-related treatment discontinuation (odds ratio 0.79–0.90) [14].
Overall, this MAIC identifies potential differences in the efficacy profiles of tepotinib, capmatinib, savolitinib, and crizotinib. In particular, there is tendency towards probability of superiority for PFS in favor of tepotinib compared with capmatinib and crizotinib. Further investigation will be required to confirm and identify specific patient or disease characteristics that might be used to select between these agents.
Change history
20 July 2022
The article is updated due to correct link of reference 21.
References
Paik PK, Felip E, Veillon R, et al. Tepotinib in non-small-cell lung cancer with MET exon 14 skipping mutations. N Engl J Med. 2020;383(10):931–43.
Wolf J, Seto T, Han JY, et al. Capmatinib in MET exon 14-mutated or MET-amplified non-small-cell lung cancer. N Engl J Med. 2020;383(10):944–57.
Lu S, Fang J, Li X, et al. Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations: a multicentre, single-arm, open-label, phase 2 study. Lancet Respir Med. 2021;9(10):1154–64.
US Food and Drug Administration. TEPMETKO (tepotinib) Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214096s000lbl.pdf. Accessed Feb 2022.
US Food and Drug Administration. TABRECTA (capmatinib) Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213591s000lbl.pdf. Accessed Feb 2022.
Paik P. MA11.05—Tepotinib in patients with MET exon14 (METex14) skipping advanced NSCLC: updated efficacy results from VISION Cohort A. Presented at IASLC 2021. https://library.iaslc.org/conference-program?product_id=20&author=&category=&date=&session_type=&session=&presentation=MA11.05&keyword=&cme=undefined&. Accessed Feb 2022.
Markham A. Savolitinib: first approval. Drugs. 2021;81(14):1665–70.
NCCN. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Guideline Non-Small Cell Lung Cancer V1.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed Jan 2022. To view the most recent and complete version of the guideline, go online to NCCN.org.
Planchard D, Popat S, Kerr K, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;29iv:192–237.
Dong Y, Xu J, Sun B, Wang J, Wang Z. MET-targeted therapies and clinical outcomes: a systematic literature review. Mol Diagn Ther. 2022;26(0123456789):203–27.
Signorovitch JE, Sikirica V, Erder MH, et al. Matching-adjusted indirect comparisons: a new tool for timely comparative effectiveness research. Value Health. 2012;15(6):940–7.
Phillippo DM, Ades AE, Dias S, Palmer S, Abrams KR, Welton NJ. Methods for population-adjusted indirect comparisons in health technology appraisal. Med Decis Mak. 2018;38(2):200–11.
Halmos B, Burke T, Kalyvas C, Vandormael K, Frederickson A, Piperdi B. Pembrolizumab+chemotherapy versus atezolizumab+chemotherapy+/−bevacizumab for the first-line treatment of non-squamous NSCLC: a matching-adjusted indirect comparison. Lung Cancer. 2021;155:175–82.
Chu P, Antoniou M, Bhutani MK, Aziez A, Daigl M. Matching-adjusted indirect comparison: entrectinib versus crizotinib in ROS1 fusion-positive non-small cell lung cancer. J Comp Eff Res. 2020;9(12):861–76.
Halmos B, Burke T, Kalyvas C, et al. A matching-adjusted indirect comparison of pembrolizumab + chemotherapy vs. nivolumab + ipilimumab as first-line therapies in patients with PD-L1 TPS ≥1% metastatic NSCLC. Cancers (Basel). 2020;12(12):3648.
Drilon A, Clark JW, Weiss J, et al. Antitumor activity of crizotinib in lung cancers harboring a MET exon 14 alteration. Nat Med. 2020;26(1):47–51.
Yu Y, Ren Y, Fang J, et al. Abstract CT158: ctDNA analysis in the savolitinib phase II study in non-small cell lung cancer (NSCLC) patients (pts) harboring MET exon 14 skipping alterations (METex14). Cancer Res. (2021);81(13_Supplement):CT158.
Felip E, Garassino MC, Sakai H, et al. P45.03 Tepotinib in patients with MET exon 14 skipping NSCLC as identified by liquid or tissue biopsy. J Thorac Oncol. 2021;16(10):S1085.
Garassino MCC, Felip E, Sakai H, et al. 1254P Efficacy and safety of tepotinib in patients (pts) with advanced age: VISION subgroup analysis of pts with MET exon 14 (METex14) skipping NSCLC. Ann Oncol. 2021;32:S984–5.
Guyot P, Ades A, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan–Meier survival curves. BMC Med Res Methodol. 2012;12(1):9.
Center for Drug Evaluation and Research. NDA/BLA Multi-disciplinary Review and Evaluation NDA 213591 (TABRECTA, Capmatinib), 2020. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/213591Orig1s000MultidisciplineR.pdf. Accessed Feb 2022.
Wolf J, Garon EB, Groen HJM, et al. Capmatinib in MET exon 14-mutated, advanced NSCLC: updated results from the GEOMETRY mono-1 study. J Clin Oncol. 2021;39(15_suppl):9020–9020.
Karim NA, Schuster J, Eldessouki I, et al. Pulmonary sarcomatoid carcinoma: University of Cincinnati experience. Oncotarget. 2018;9(3):4102–8.
Steuer CE, Behera M, Liu Y, et al. Pulmonary sarcomatoid carcinoma: an analysis of the national cancer data base. Clin Lung Cancer. 2017;18(3):286–92.
Ishak KJ, Proskorovsky I, Benedict A. Simulation and matching-based approaches for indirect comparison of treatments. Pharmacoeconomics. 2015;33(6):537–49.
Socinski MA, Pennell NA, Davies KD. MET exon 14 skipping mutations in non–small-cell lung cancer: an overview of biology, clinical outcomes, and testing considerations. JCO Precis Oncol. 2021;3(5):653–63.
Coleman N, Harbery A, Heuss S, Vivanco I, Popat S. Targeting un-MET needs in advanced non-small cell lung cancer. Lung Cancer. 2022;164:56–68.
Drusbosky LM, Dawar R, Rodriguez E, Ikpeazu CV. Therapeutic strategies in METex14 skipping mutated non-small cell lung cancer. J Hematol Oncol. 2021;14(1):1–10.
Hong L, Zhang J, Heymach JV, Le X. Current and future treatment options for MET exon 14 skipping alterations in non-small cell lung cancer. Ther Adv Med Oncol. 2021;13:1–16.
Camidge DR, Bang Y-J, Kwak EL, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011–9.
Acknowledgements
Funding
This study and the VISION trial, the journal’s Rapid Service and Open Access Fees were funded by the healthcare business of Merck KGaA, Darmstadt, Germany.
Medical writing, editorial and other assistance
Medical writing assistance and editorial assistance was provided by Syneos Health Communications, London, UK, and funded by the healthcare business of Merck KGaA, Darmstadt, Germany.
Authorship
All named authors met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, took responsibility for the integrity of the work as a whole, and had given approval for this manuscript to be published.
Author contributions
Conceptualization: Boris M. Pfeiffer & Helene Vioix, Methodology: Paul K. Paik, Boris M. Pfeiffer and Maarten J. Postma, Formal analysis and investigation: Boris M. Pfeiffer, Helene Vioix and Andrea Garcia, Writing—original draft preparation: Paul K. Paik, Boris M. Pfeiffer, Helene Vioix, Andrea Garcia and Maarten J. Postma, Writing—review and editing: Paul K. Paik, Boris M. Pfeiffer, Helene Vioix, Andrea Garcia and Maarten J. Postma, Resources: Boris M. Pfeiffer & Helene Vioix.
Disclosures
PKP holds advisory roles at AstraZeneca, Calithera, Takeda, EMD Serono, Xencor, Bicara, Boehringer Ingelheim, GlaxoSmithKline and CrownBio alongside his research institution having received research expenses from Bicara, Boehringer Ingelheim, and EMD Serono. BMP and HV are full-time employees of the healthcare business of Merck KGaA, Darmstadt, Germany. AG is a full-time employee of Cytel. MJP was supported in co-developing the methodology of this paper with a grant from the healthcare business of Merck KGaA, Darmstadt, Germany. MJP receives further grants and honoraria from various pharmaceutical companies, all unrelated to this research. MJP holds stocks in Health-Ecore (Zeist, The Netherlands) and Pharmacoeconomics Advice Groningen (Groningen, The Netherlands).
Compliance with ethics guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data availability
Any requests for data by qualified scientific and medical researchers for legitimate research purposes will be subject to the healthcare business of Merck KGaA, Darmstadt, Germany, Data Sharing Policy. All requests should be submitted in writing to the healthcare business of Merck KGaA, Darmstadt, Germany, data sharing portal (https://www.emdgroup.com/en/research/our-approach-to-research-and-development/healthcare/clinical-trials/commitment-responsible-data-sharing.html).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Paik, P.K., Pfeiffer, B.M., Vioix, H. et al. Matching-Adjusted Indirect Comparison (MAIC) of Tepotinib with Other MET Inhibitors for the Treatment of Advanced NSCLC with MET Exon 14 Skipping Mutations. Adv Ther 39, 3159–3179 (2022). https://doi.org/10.1007/s12325-022-02163-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02163-9