Abstract
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder that affects multiple organ systems. The most prevalent manifestations include constitutional symptoms, arthritis, and rash. An SLE flare is defined as a measurable increase in disease activity that may prompt a change in treatment. According to the European Alliance of Associations for Rheumatology guidance, SLE treatments should be aimed at reducing disease activity and flares, as well as preventing organ damage. Standard-of-care treatment of SLE includes glucocorticoids, but their long-term use is associated with damage accrual. Repository corticotropin injection (RCI; Acthar® Gel) is a naturally sourced complex mixture of adrenocorticotropic hormone analogs and other pituitary peptides that has anti-inflammatory and immunomodulatory effects beyond its steroidogenic effect, and has been US Food and Drug Administration–approved for the treatment of SLE flares and as a maintenance therapy. This review summarizes data from three clinical trials that evaluated the efficacy and safety of RCI in the treatment of patients with moderate–severe refractory SLE. These clinical trials confirmed that RCI improved global disease activity scores and some SLE clinical manifestations. Analysis of pooled data from these trials showed that RCI treatment significantly improved the British Isles Lupus Assessment Group 2004 (BILAG-2004) index scores after 8 weeks of treatment, and tender and swollen joint counts after 4 weeks. These clinical trials demonstrated an acceptable safety profile with few serious adverse events reported. The distinct mechanisms of action from standard-of-care therapies and the favorable safety and good efficacy profiles support the use of RCI as therapy for patients with refractory SLE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many patients with systemic lupus erythematosus (SLE) have refractory disease that is not responsive to standard-of-care therapies, such that alternative treatments are needed. |
Repository corticotropin injection (RCI; Acthar® Gel) is a naturally sourced complex mixture of adrenocorticotropic hormone analogs and other pituitary peptides indicated for the treatment of SLE that has anti-inflammatory and immunomodulatory effects beyond its steroidogenic effect. |
The clinical trial results and the pooled data analysis presented here demonstrate that RCI treatment provided early reduction in the SLE Disease Activity Index (SLEDAI), the British Isles Lupus Assessment Group 2004 (BILAG-2004) index, and swollen and tender joint counts. |
Treatment with RCI showed an acceptable safety profile with generally mild–moderate adverse events and few serious adverse events. |
The data reported in these clinical trials suggest that RCI may be safe and effective for the treatment of moderate–severe refractory SLE. |
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder with an unpredictable course and the potential for affecting multiple organ systems [1, 2]. The most common manifestations of SLE are fatigue, arthritis, and rash [1, 3,4,5,6]. Like other autoimmune disorders, SLE has a relapsing–remitting or a chronic progressive course with fluctuating disease activity. SLE flares are measurable exacerbations of disease activity in one or more organ systems [7]. Most patients with SLE have recurrent disease flares [8]. Risk factors for repeated SLE flares include African American race, male sex, disease onset at ≤ 25 years of age, presence of neuropsychiatric symptoms, cytopenia, nephritis, vasculitis, and poor treatment adherence [8]. Triggers include sun exposure, medication changes, hormonal changes, and infections [2]. Preventing and reducing damage accrual is a primary goal of SLE treatment, and this is best achieved by reducing disease activity, preventing flares, and minimizing steroid use [8].
The pathophysiology of SLE is not entirely understood [1, 9]. Environmental, hormonal, and genetic factors lead to abnormal innate and adaptive immune responses, production of auto-antibodies, inflammation, tissue damage, and the clinical manifestations of SLE [1, 2]. Dysregulated and hyper-reactive B cells are central to the immune dysfunction in SLE [10, 11]. B cells serve as antigen-presenting cells (of self-antigens in SLE) and produce auto-antibodies, leading to overexpression of pro-inflammatory cytokines including tumor necrosis factor α (TNF-α), interleukin (IL)-6, IL-10, B cell activating factor (BAFF), and a proliferation-inducing ligand (APRIL) [11, 12].
This review summarizes the evidence supporting the use of repository corticotropin injection (RCI; Acthar® Gel) as a treatment option for SLE from studies published after 2010. This manuscript is based on previously performed and published studies and does not contain any new human participants or animal studies performed by any of the authors.
Steroids are a Standard Treatment Option for SLE
The selection of therapies for SLE is determined by the disease manifestations, their severity, and comorbidities [1]. In general, treatment of SLE is divided into two phases: induction of remission/low disease activity and maintenance. Based on the recent guidelines from the European Alliance of Associations for Rheumatology and others, treatment goals are to lower disease activity, achieve remission, and prevent flares in order to reduce cumulative organ damage, morbidity, and mortality [13,14,15]. These treatment guidelines recommend antimalarials and glucocorticoids as first-line therapies, whereas immunosuppressants and biologics are administered to those with disease that is more difficult to treat [13,14,15]. Suboptimal response rates and treatment side effects, especially those adverse events (AEs) caused by steroids, underscore the need for safer and more effective therapies [12]. Chronic glucocorticoid use may contribute to hypertension (> 30%), cataracts, osteoporosis (21–30%), hyperglycemia (fourfold increase), cardiovascular events (4%), Cushingoid appearance (4–70%), psychiatric manifestations, and/or avascular necrosis [16, 17]. It is estimated that approximately 80% of the damage that occurs in SLE can be attributed to steroid exposure [18]. Despite these substantial risks, steroids have been transformative in the care of patients with inflammatory diseases. However, many patients who receive treatment with maximized standard-of-care therapies, including glucocorticoids, may continue to experience SLE flares. Therefore, alternative treatments for refractory SLE are needed.
RCI for the Treatment of SLE
RCI is a naturally sourced complex mixture of adrenocorticotropic hormone analogs and other pituitary peptides that is US Food and Drug Administration–approved for the treatment of SLE flares and as a maintenance therapy [19]. As an agonist of all five melanocortin receptors (MCRs), RCI likely provides therapeutic efficacy in the treatment of SLE via multiple mechanisms of action. Preclinical studies have shown that RCI is a full agonist of MC1R, MC2R, MC3R, and MC4R and a partial agonist of MC5R [20]. The anti-inflammatory mechanism of action for RCI was originally thought to be via activation of MC2R on adrenocortical cells, which stimulates production of endogenous cortisol; however, recent evidence has shown that RCI has relatively low agonistic activity of MC2R [20, 21]. This is supported by studies in animals [20] and healthy human subjects [21, 22], which showed lower levels of endogenous corticosteroid production after administration of RCI compared to synthetic ACTH1–24 (Fig. 1).
Baseline-corrected plasma free cortisol concentrations in healthy human subjects after RCI or synthetic ACTH1–24 depot administration on study day 1 (A) and day 4 (B); baseline-corrected free cortisol concentrations were calculated by subtracting the time-matched baseline (day−1) free cortisol concentrations from the respective day 1 and day 4 free cortisol concentrations for each study drug. The basal range of plasma free cortisol concentration (0.2–23.0 ng/mL) is shaded gray. ACTH1–24 first 24 amino acids of adrenocorticotropic hormone, RCI repository corticotropin injection, SEM standard error of the mean. Reproduced from Poola et al. [22] under the CC BY-NC-ND 4.0 open access license
In vitro and animal studies have demonstrated direct, steroidogenesis-independent, immunomodulatory effects of RCI [10, 22,23,24,25,26]. Studies of human B cells reported that RCI inhibits their activation and proliferation and reduces immunoglobulin G (IgG) production [23, 25]. In human monocyte-derived macrophages, RCI directly reduced inflammatory cytokine release, including TNF-α and IL-6 [26]. Mouse models of SLE have shown that RCI treatment significantly reduced levels of splenic follicular and germinal center B cells, as well as T helper and dendritic cells [10, 24]. Taken together, preclinical evidence supports that RCI functions through multiple, direct, non-steroidogenic mechanisms in different immune cell types (Fig. 2). Additional studies are needed to demonstrate a direct immunomodulatory effect of RCI in patients with SLE.
To our knowledge, head-to-head mechanistic studies of RCI versus glucocorticoids have not been performed. While both have anti-inflammatory effects, the molecular mechanisms are different. Glucocorticoids activate the glucocorticoid receptor [27], and RCI activates MCRs [20], likely inducing different signaling mechanisms. How MCR versus glucocorticoid receptor signaling causes different immunomodulatory or anti-inflammatory responses is currently unclear. While RCI does stimulate glucocorticoid release from the adrenal cortex, the cortisol levels are relatively low (as shown in Fig. 1). Therefore, it has been hypothesized that the primary mechanism of action for RCI may be through direct modulation of immune cell activity, as most immune cells express MCRs [23, 25, 28].
Studies on the molecular and cellular mechanisms of RCI are sparse; however, clinical studies have supported that RCI has a unique mechanism of action that differs from glucocorticoids, since RCI has demonstrated efficacy in subjects with refractory inflammatory diseases despite receiving glucocorticoid treatment [29,30,31]. A recent systematic review comparing the safety of RCI with glucocorticoids in the treatment of rheumatoid arthritis demonstrated that RCI has a more favorable safety profile with fewer AEs compared to glucocorticoids, further suggesting that RCI has a unique mechanism of action beyond its steroidogenic effects [31].
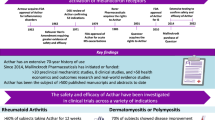
As reported by three recent clinical trials, RCI demonstrated efficacy in patients with SLE that had not responded to standard-of-care therapies, including glucocorticoids (summarized in Table 1) [29, 32,33,34,35]. Additionally, two retrospective chart reviews found that RCI improved disease activity scores in patients with SLE that had not responded to standard SLE therapies [36, 37].
The efficacy and safety of RCI in reducing disease activity, when used as an adjunctive treatment in patients with moderate–severe SLE, was evaluated in a 28-day open-label study in 10 female patients [32], followed by a 6-month extension in 5 female patients [33]. Outcomes included physician (PGA) and patient global assessments (PtGA); SLE Disease Activity Index-2000 (SLEDAI-2K); British Isles Lupus Assessment Group 2004 (BILAG-2004) index; swollen, tender, and total joint counts; Lupus Quality of Life (Lupus QoL) questionnaire; Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) questionnaire; erythrocyte sedimentation rate (ESR); and C-reactive protein (CRP) [32, 33]. Outcomes were assessed weekly for 28 days, then every 3 months for 6 months. The study results showed that SLEDAI-2K scores (primary endpoint) significantly improved from baseline at day 28, month 3, and month 6 [32, 33]. Significant improvements in all clinical outcome measures, except CRP, were observed at day 28, whereas tender joint count, swollen joint count, and the combined total joint count also significantly improved from baseline at month 3 and month 6 [32, 33]. No serious adverse events (SAEs) after RCI initiation were reported in these studies [32, 33]. These results suggested that RCI may significantly and safely reduce SLE disease activity among patients who were not responsive to conventional treatments.
A pilot study [34] and post hoc analyses [35] assessed the efficacy and safety of RCI in patients with glucocorticoid-treated SLE over an 8-week double-blind, placebo-controlled period, and an optional 44-week open-label extension period. Although the proportion of patients showing a response to treatment based on a hybrid SLEDAI (hSLEDAI) measured at week 4 (primary endpoint) did not reach statistical significance, several secondary endpoints were attained (BILAG-2004; Cutaneous Lupus Erythematosus Disease Area and Severity Index [CLASI]-Activity; tender and swollen joint count; PGA). Several post hoc analyses have demonstrated that RCI treatment was associated with improvements in disease activity measures in patients with persistent disease activity despite glucocorticoid treatment [34, 35]. No new safety signals were identified, although the incidence of infections was higher in the RCI group than in the placebo group; the most common treatment-emergent AE after administration of RCI was weight gain [34, 35].
A multicenter, double-blind, randomized, placebo-controlled study [29] evaluated the efficacy and safety of RCI in patients with persistently active SLE despite the use of moderate-dose glucocorticoids. Although the proportion of SLE Responder Index-4 (SRI-4) responders at week 16 (primary endpoint) did not reach statistical significance, there were improvements for subjects treated with RCI versus placebo in the secondary endpoints of 28 swollen joint count/tender joint count and CLASI-Activity scores [29]. Post hoc analyses of data from subjects with high levels of disease activity revealed significantly more SRI-4 responders among those who received RCI versus placebo [29]. RCI treatment resulted in a greater number of BILAG-based Combined Lupus Assessment (BICLA) responders than placebo in a post hoc analysis of the modified intention-to-treat population [29]. Further, cytokine analysis showed that BAFF levels significantly decreased from baseline values in subjects receiving RCI compared to the placebo group [29]. BAFF increases B cell activity and function and is central to the pathophysiology of SLE [38]. Therefore, the reduction of BAFF after treatment of SLE with RCI may contribute to the observed clinical outcomes of reduced disease activity.
Safety results were consistent with the established safety profile of RCI, and no new safety signals were observed [29]. The most common AEs reported by patients treated with RCI were upper respiratory tract infection, insomnia, headache, hypertension, and urinary tract infection; SAEs included SLE flare, herpes zoster, hyperglycemia, and nephrotic syndrome (Table 2) [29]. Notably, more subjects treated with RCI reported hypertension and hyperglycemia, whereas twice as many subjects in the placebo group reported SAEs (Table 2) [29]. No changes in the bone turnover markers N-terminal propeptide of type I collagen (PINP) and C-terminal crosslinking telopeptide of type I collagen (CTX-I) were observed, suggesting that RCI treatment had no adverse effect on bone [29].
Post hoc analyses of these clinical trial data [29] further investigated the molecular and cellular biomarkers underlying the effects of RCI on B cell immunomodulation [39]. Data were analyzed in subgroups stratified by disease activity at baseline, comparing results from subjects with SLEDAI-2K ≥ 10 versus SLEDAI-2K < 10 or anti-dsDNA ≥ 15 IU/mL versus anti-dsDNA < 15 IU/mL or from BICLA responders versus BICLA nonresponders [39]. BAFF levels were reduced from baseline with RCI treatment compared with placebo in nearly every subgroup, and time point analyzed [39]. Lower levels of IL-6 were observed in patients treated with RCI versus placebo at most time points across all disease-activity subgroups [39]. RCI treatment decreased numbers of CD19+ B cells in all subgroups at weeks 16 and 24 compared with placebo in patients with high disease activity [39]. RCI-treated subjects with high baseline disease activity showed lower levels of CD19+IgD−CD27−CD95+ atypical activated memory B cells than placebo-treated subjects; similar results were noted in BICLA nonresponders [39]. Elevated levels of CD19+ B cells or CD19+IgD−CD27−CD95+ memory B cells correlate with increased SLE disease activity [40, 41]; therefore, this reduction in B cells with RCI therapy may provide insights into the clinical outcomes observed in the clinical trial and the mechanisms of action of RCI [29]. Analysis of complement levels revealed that, after RCI treatment, C3 and C4 levels increased in subjects with high baseline disease activity. Since complement C3 and C4 are often low in patients with immune-mediated diseases, these results suggest that RCI may restore normality of the complement system in patients with SLE [39].
Patient-reported outcomes from subjects in the aforementioned clinical trial [29] were analyzed using the Lupus QoL questionnaire and the Work Productivity and Activity Impairment (WPAI)-Lupus questionnaire [42]. Post hoc analysis uncovered significant improvements with RCI treatment in quality of life and work productivity, particularly in patients with high disease activity. Compared with placebo, subjects treated with RCI reported significant improvements in the Lupus QoL pain, planning, and fatigue domains and in the domains of WPAI-Lupus percentage impairment while working and percentage work time missed [42].
To further define the effects of RCI in a larger population of patients with SLE, data from week 4 and week 8 of the clinical trial [29] were pooled with those from the pilot study [34]. Analysis of the pooled data revealed a significantly larger reduction from baseline in 28-joint count (tender and swollen) total scores (Fig. 3) and BILAG-2004 total scores (Fig. 4) in subjects receiving RCI than in those receiving placebo.
Pooled data analysis of 28-joint count (tender and swollen) total scores by visit. RCI repository corticotropin injection. Data were pooled from a recent clinical trial (Askanase et al. [29]) and a pilot study (Furie et al. [34]). Symbols represent mean change ± SEM. Data were analyzed using analysis of covariance models with the change from baseline as the dependent variable, treatment as the factor, and baseline value of the corresponding endpoint as the covariate. Data were adjusted for the stratification variables used for randomization, location (US and outside the US), and prednisone equivalent dose (≤ 20 and > 20 mg/day)
Pooled data analysis of BILAG-2004 total scores by visit. BILAG-2004 British Isles Lupus Assessment Group-2004 index, RCI repository corticotropin injection. Data were pooled from a recent clinical trial (Askanase et al. [29]) and a pilot study (Furie et al. [34]). Symbols represent mean change ± SEM. Data were analyzed using analysis of covariance models with the change from baseline as the dependent variable, treatment as the factor, and baseline value of the corresponding endpoint as the covariate. Data were adjusted for the stratification variables used for randomization, location (US and outside the US), and prednisone equivalent dose (≤ 20 and > 20 mg/day)
Pooled data analyses also demonstrated greater reductions from baseline in SLEDAI (SLEDAI-2K and hSLEDAI), CLASI-Activity, and PGA scores in the RCI group compared with the placebo group (Table 3). A greater proportion of SRI-4 and BICLA responders were observed with RCI treatment compared with placebo (Table 4).
Discussion
This article provides a review of the recently published data on RCI in SLE. The results of pooled data from a pilot study and a clinical trial revealed early improvement in the 28-joint counts (total and swollen) and BILAG-2004 scores in patients with SLE receiving RCI, as well as greater proportions of SRI-4 and BICLA responders in the RCI group compared with placebo, supporting a role for RCI in the treatment of SLE.
No new safety signals were observed in these clinical trials, comparable to composing the long-established safety profile of RCI, and few SAEs were observed [29, 32,33,34,35,36,37]. Treatment-related SAEs included chest discomfort/gastroesophageal disease, pelvic abscess, and pyelonephritis [34, 35]. A 26-week study of RCI for the treatment of rheumatoid arthritis in 259 subjects reported a similar low frequency of SAEs: 1 case each of chest pain, craniocerebral injury, and pneumonia [31, 43]. The acceptable safety profile of RCI is advantageous when considering patients with refractory SLE who require additional therapies or increased doses of corticosteroids.
RCI likely derives its efficacy via activation of all five MCRs [20, 32, 37]. In vitro studies have found that treatment with RCI directly reduced cytokine release from macrophages [26] and inhibited B cell proliferation [23]. In the clinical trial, patients with SLE treated with RCI had reduced levels of IL-6 and BAFF [39]. Elevated levels of IL-6 in patients with SLE result in systemic and local inflammatory effects, including induction of leukocyte differentiation (B and T cells) and proliferation (T cells and macrophages), autoantibody production, and increased SLE disease activity [44]. Dysfunctional BAFF signaling underlies mouse models of SLE, in which increased BAFF levels cause an SLE-like autoimmune disease, and reduced BAFF levels cause immunodeficiency [38]. BAFF is primarily secreted by macrophages, dendritic cells, and neutrophils and activates multiple BAFF-receptor subtypes expressed on B cells, increasing their maturation and survival [38]. Notably, treatment of patients with SLE with RCI reduced total B cells (CD19+) and atypical activated memory B cells (CD19+IgD−CD27−CD95+) [39], which correlate with SLE disease activity [39,40,41]. Together, these data suggest that RCI effects on IL-6 and BAFF signaling may reduce activated B cells [29, 39].
While glucocorticoids are central to the treatment of SLE, the long-term side effects, such as hypertension, osteoporosis, diabetes, and their contribution to organ damage accrual, limit their use [16,17,18]. Despite standard treatment, many patients experience continued disease activity and SLE flares and require additional therapies. Patients with SLE showed improvement in disease activity scores and clinical outcomes after treatment with RCI in addition to stable doses of glucocorticoids (7.5–30 mg prednisone equivalent) [29, 32,33,34,35,36,37], suggesting that the effectiveness of RCI is due to a mechanism that is additive to or separate from its classical steroidogenic mechanism of action via MC2R activation in the adrenal cortex. Additionally, RCI may have a steroid-sparing effect, as reported by Fietchner et al. [33] and Li et al. [37]. While data are limited, the current review supports the positive effects of RCI in the treatment of SLE and substantiates the need for a larger clinical trial to further define the role of RCI in SLE and to assess its potential to be a safer alternative to the current glucocorticoid regimens.
Conclusions
There are unmet needs in the treatment of SLE, especially for patients who continue to experience flares despite receiving standard-of-care therapies. Currently, there is no defined role for RCI in SLE clinical guidelines. The data presented here suggest that RCI may be a safe and effective adjunctive treatment for patients with refractory SLE. The unique mechanism of action of RCI provides an alternative treatment option for patients with insufficient disease control using current standard-of-care treatments. Given its few treatment-related SAEs, positive efficacy results, and distinct mechanisms of action, clinicians may consider using RCI as an early-line therapy, particularly for patients with refractory SLE.
References
Fortuna G, Brennan MT. Systemic lupus erythematosus: epidemiology, pathophysiology, manifestations, and management. Dent Clin North Am. 2013;57(4):631–55. https://doi.org/10.1016/j.cden.2013.06.003.
Fernandez D, Kirou KA. What causes lupus flares? Curr Rheumatol Rep. 2016;18(3):14. https://doi.org/10.1007/s11926-016-0562-3.
Azizoddin DR, Gandhi N, Weinberg S, Sengupta M, Nicassio PM, Jolly M. Fatigue in systemic lupus: the role of disease activity and its correlates. Lupus. 2019;28(2):163–73. https://doi.org/10.1177/0961203318817826.
Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25(11):1271–7. https://doi.org/10.1002/art.1780251101.
Petri M, Orbai AM, Alarcon GS, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–86. https://doi.org/10.1002/art.34473.
Thong B, Olsen NJ. Systemic lupus erythematosus diagnosis and management. Rheumatology (Oxford). 2017;56(suppl_1):i3–13. https://doi.org/10.1093/rheumatology/kew401.
Ruperto N, Hanrahan LM, Alarcon GS, et al. International consensus for a definition of disease flare in lupus. Lupus. 2011;20(5):453–62. https://doi.org/10.1177/0961203310388445.
Adamichou C, Bertsias G. Flares in systemic lupus erythematosus: diagnosis, risk factors and preventive strategies. Mediterr J Rheumatol. 2017;28(1):4–12. https://doi.org/10.31138/mjr.28.1.4.
Carter EE, Barr SG, Clarke AE. The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol. 2016;12(10):605–20. https://doi.org/10.1038/nrrheum.2016.137.
Decker DA, Grant C, Oh L, Becker PM, Young D, Jordan S. Immunomodulatory effects of H.P. Acthar Gel on B cell development in the NZB/W F1 mouse model of systemic lupus erythematosus. Lupus. 2014;23(8):802–12. https://doi.org/10.1177/0961203314531840.
Dorner T, Giesecke C, Lipsky PE. Mechanisms of B cell autoimmunity in SLE. Arthritis Res Ther. 2011;13(5):243. https://doi.org/10.1186/ar3433.
Durcan L, Petri M. Immunomodulators in SLE: clinical evidence and immunologic actions. J Autoimmun. 2016;74:73–84. https://doi.org/10.1016/j.jaut.2016.06.010.
Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736–45. https://doi.org/10.1136/annrheumdis-2019-215089.
Pons-Estel BA, Bonfa E, Soriano ER, et al. First Latin American clinical practice guidelines for the treatment of systemic lupus erythematosus: Latin American Group for the Study of Lupus (GLADEL, Grupo Latino Americano de Estudio del Lupus)-Pan-American League of Associations of Rheumatology (PANLAR). Ann Rheum Dis. 2018;77(11):1549–57. https://doi.org/10.1136/annrheumdis-2018-213512.
Gordon C, Amissah-Arthur MB, Gayed M, et al. The British Society for Rheumatology guideline for the management of systemic lupus erythematosus in adults. Rheumatology (Oxford). 2018;57(1):e1–45. https://doi.org/10.1093/rheumatology/kex286.
Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39(11):2216–29. https://doi.org/10.1016/j.clinthera.2017.09.011.
Liu D, Ahmet A, Ward L, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. 2013;9(1):30. https://doi.org/10.1186/1710-1492-9-30.
Gladman DD, Urowitz MB, Rahman P, Ibanez D, Tam LS. Accrual of organ damage over time in patients with systemic lupus erythematosus. J Rheumatol. 2003;30(9):1955–9.
Mallinckrodt ARD. Acthar Gel (Repository Corticotropin Inection). Bedminster: Mallinckrodt ARD LLC; 2021. https://www.acthar.com/Static/pdf/Acthar-PI.pdf. Published February 2021. Accessed March 2, 2022.
Huang YJ, Galen K, Zweifel B, Brooks LR, Wright AD. Distinct binding and signaling activity of Acthar Gel compared to other melanocortin receptor agonists. J Recept Signal Transduct Res. 2021;41(5):425–33. https://doi.org/10.1080/10799893.2020.1818094.
Wang X, Pham L, Poola N, Brooks LR, Due B. Comparison of steroidogenic exposure following the administration of repository corticotropin injection with a synthetic ACTH1–24 depot and methylprednisolone in healthy subjects. Clin Pharmacol Drug Dev. 2021;10(7):777–88. https://doi.org/10.1002/cpdd.894.
Poola N, Due B, Wright D, Brooks LR, Zaman F. Pharmacokinetics and pharmacodynamics of repository corticotropin injection compared with synthetic ACTH1–24 depot and methylprednisolone in healthy subjects. Clin Pharmacol Drug Dev. 2021. https://doi.org/10.1002/cpdd.1020 (Epub ahead of print).
Olsen NJ, Decker DA, Higgins P, et al. Direct effects of HP Acthar Gel on human B lymphocyte activation in vitro. Arthritis Res Ther. 2015;17:300. https://doi.org/10.1186/s13075-015-0823-y.
Higgins P, Decker D, Becker P. Immunomodulatory effects of repository corticotropin injection (H.P. Acthar® gel) on the MRL/lpr model of lupus. J Immunol. 2016;196(1 Supplement):210.11. https://doi.org/10.1177/0961203314531840.
Benko AL, McAloose CA, Becker PM, et al. Repository corticotrophin injection exerts direct acute effects on human B cell gene expression distinct from the actions of glucocorticoids. Clin Exp Immunol. 2018;192(1):68–81. https://doi.org/10.1111/cei.13089.
Healy LM, Jang JH, Lin YH, Rao V, Antel JP, Wright D. Melanocortin receptor mediated anti-inflammatory effect of repository corticotropin injection on human monocyte-derived macrophages [ECTRIMS-ACTRIMS abstract EP1481]. Mult Scler J. 2017;23(suppl 3):777. https://doi.org/10.1186/s12891-020-03609-3.
Timmermans S, Souffriau J, Libert C. A general introduction to glucocorticoid biology. Front Immunol. 2019;10:1545. https://doi.org/10.3389/fimmu.2019.01545.
Catania A, Lonati C, Sordi A, Carlin A, Leonardi P, Gatti S. The melanocortin system in control of inflammation. Sci World J. 2010;10:1840–53. https://doi.org/10.1100/tsw.2010.173.
Askanase AD, Zhao E, Zhu J, Bilyk R, Furie RA. Repository corticotropin injection for persistently active systemic lupus erythematosus: results from a phase 4, multicenter, randomized, double-blind, placebo-controlled trial. Rheumatol Ther. 2020;7(4):893–908. https://doi.org/10.1007/s40744-020-00236-1.
Baughman RP, Sweiss N, Keijsers R, et al. Repository corticotropin for chronic pulmonary sarcoidosis. Lung. 2017;195(3):313–22. https://doi.org/10.1007/s00408-017-9994-4.
Fleischmann R, Furst DE, Connolly-Strong E, Liu J, Zhu J, Brasington R. Repository corticotropin injection for active rheumatoid arthritis despite aggressive treatment: a randomized controlled withdrawal trial. Rheumatol Ther. 2020;7(2):327–44. https://doi.org/10.1007/s40744-020-00199-3.
Fiechtner JJ, Montroy T. Treatment of moderately to severely active systemic lupus erythematosus with adrenocorticotropic hormone: a single-site, open-label trial. Lupus. 2014;23(9):905–12. https://doi.org/10.1177/0961203314532562.
Fiechtner J, Montroy T. Six months’ treatment of moderately to severely active systemic lupus erythematosus with repository corticotropin injection: an extension of a single-site, open-label trial. J Immunol Clin Res. 2016;3(1):1025–30.
Furie R, Mitrane M, Zhao E, Das M, Li D, Becker PM. Efficacy and tolerability of repository corticotropin injection in patients with persistently active SLE: results of a phase 4, randomised, controlled pilot study. Lupus Sci Med. 2016;3(1): e000180. https://doi.org/10.1136/lupus-2016-000180.
Furie RA, Mitrane M, Zhao E, Becker PM. Repository corticotropin injection in patients with persistently active SLE requiring corticosteroids: post hoc analysis of results from a two-part, 52-week pilot study. Lupus Sci Med. 2017;4(1): e000240. https://doi.org/10.1136/lupus-2017-000240.
Ho-Mahler N, Turner B, Eaddy M, Hanke ML, Nelson WW. Treatment with repository corticotropin injection in patients with rheumatoid arthritis, systemic lupus erythematosus, and dermatomyositis/polymyositis. Open Access Rheumatol. 2020;12:21–8. https://doi.org/10.2147/OARRR.S231667.
Li X, Golubovsky J, Hui-Yuen J, et al. Adrenocorticotropic hormone gel in the treatment of systemic lupus erythematosus: a retrospective study of patients. F1000Res. 2015;4:1103. https://doi.org/10.12688/f1000research.7192.2.
Vincent FB, Morand EF, Schneider P, Mackay F. The BAFF/APRIL system in SLE pathogenesis. Nat Rev Rheumatol. 2014;10(6):365–73. https://doi.org/10.1038/nrrheum.2014.33.
Askanase AD, Wright D, Zhao E, Zhu J, Bilyk R, Furie RA. Post hoc biomarker analyses from a phase 4, multicenter, randomized, double-blind, placebo-controlled trial of repository corticotropin injection (Acthar(R) Gel) for persistently active systemic lupus erythematosus. Rheumatol Ther. 2021;8(4):1871–86. https://doi.org/10.1007/s40744-021-00351-7.
Jacobi AM, Reiter K, Mackay M, et al. Activated memory B cell subsets correlate with disease activity in systemic lupus erythematosus: delineation by expression of CD27, IgD, and CD95. Arthritis Rheum. 2008;58(6):1762–73. https://doi.org/10.1002/art.23498.
Wei C, Anolik J, Cappione A, et al. A new population of cells lacking expression of CD27 represents a notable component of the B cell memory compartment in systemic lupus erythematosus. J Immunol. 2007;178(10):6624–33. https://doi.org/10.4049/jimmunol.178.10.6624.
Askanase AD, Zhao E, Zhu J, Bilyk R, Furie RA. Patient-reported outcomes from a phase 4, multicenter, randomized, double-blind, placebo-controlled trial of repository corticotropin injection (Acthar((R)) Gel) for persistently active systemic lupus erythematosus. Rheumatol Ther. 2021;8(1):573–84. https://doi.org/10.1007/s40744-021-00294-z.
Fleischmann R, Furst DE. Safety of repository corticotropin injection as an adjunctive therapy for the treatment of rheumatoid arthritis. Expert Opin Drug Saf. 2020;19(8):935–44. https://doi.org/10.1080/14740338.2020.1779219.
Ohl K, Tenbrock K. Inflammatory cytokines in systemic lupus erythematosus. J Biomed Biotechnol. 2011;2011: 432595. https://doi.org/10.1155/2011/432595.
Acknowledgements
Funding
Sponsorship for this study, the Rapid Service Fee and the Open Access Fee was provided by Mallinckrodt Pharmaceuticals (Hampton, NJ, USA).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the conception or design of the work; acquisition, analysis, or interpretation of data; drafting or critically revising the work for important intellectual content; and final approval of the manuscript.
Medical Writing and/or Editorial Assistance
Professional writing and editorial support were provided by Nestor G. Davila, PhD, of MedLogix Communications, LLC, Itasca, Illinois, USA, under the direction of the authors and was funded by Mallinckrodt Pharmaceuticals.
Author Disclosures
Anca D. Askanase has received grant and/or research support from AstraZeneca, Eli Lilly, GlaxoSmithKline, Idorsia, Janssen, Mallinckrodt Pharmaceuticals, and Pfizer. Richard A. Furie has received grant and/or research support from Genentech/Roche and GlaxoSmithKline.
Compliance with Ethics Guidelines
This manuscript is based on previously performed and published studies and does not contain any new human participant or animal studies performed by any of the authors.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Askanase, A.D., Furie, R.A. A Narrative Review of Repository Corticotropin Injection for the Treatment of Systemic Lupus Erythematosus. Adv Ther 39, 3088–3103 (2022). https://doi.org/10.1007/s12325-022-02160-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02160-y