Abstract
Introduction
Limited real-world data are available comparing multiple biologics on their adherence, persistence, and the use of concomitant biologics in the treatment of moderate-to-severe psoriasis in clinical practice. The objective was to compare persistence of and adherence to ixekizumab (IXE) treatment, as monotherapy or with concomitant medication, versus patients receiving other commonly prescribed biologics.
Methods
Patients who newly initiated IXE, adalimumab (ADA), etanercept (ETN), secukinumab (SEC), or ustekinumab (UST) in IBM MarketScan® databases with diagnosis of psoriasis were identified. Treatment comparisons on medication persistence, adherence, and monotherapy were based on balanced samples after inverse probability of treatment weighting (IPTW).
Results
A higher proportion of patients receiving IXE had had previous biologic therapies (50.3%) versus other biologics (ADA: 9.1%, ETN: 10.9%, SEC: 33.9%, UST: 19.7%). Patients treated with IXE showed statistically (p < 0.001) greater persistence than patients treated with SEC, ADA, UST, or ETN at both 1-year follow-up and up to 3 years of follow-up. Adherence for patients treated with IXE was significantly (p < 0.001) higher compared to ADA, ETN, and UST at both 1-year follow-up and up to 3 years of follow-up. There was no significantly higher adherence in patients treated with IXE compared to those treated with SEC at 1-year follow-up, but IXE had higher adherence than SEC (p < 0.05) at 1–3 year follow-up. IXE showed longer time on monotherapy than ADA (p < 0.001), ETN (p < 0.001), SEC (p < 0.05), and UST (p < 0.001) for both 1-year and 1–3 year follow-up. Sensitivity analyses on persistence, adherence, and monotherapy with further model adjustments after IPTW confirmed the findings.
Conclusions
Patients treated with IXE were more persistent on and adherent to treatment and remained on monotherapy longer compared to those on all other commonly prescribed biologics combined or with individual biologics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Although most biologics were approved as monotherapy for the treatment of moderate-to-severe psoriasis, corticosteroids and oral systemic medications are often used as add-on medications in real-world practice |
Limited real-world data are available comparing multiple biologics on their adherence, persistence, and use of concomitant biologics in the treatment of moderate-to-severe psoriasis in clinical practice |
What was learned from the study? |
Results from this study suggest that, in real-world settings, patients with psoriasis were significantly more persistent and adherent on ixekizumab treatment compared to those treated with other commonly prescribed biologics |
Patients with psoriasis remained on ixekizumab significantly longer as a monotherapy compared to other biologics |
The findings from this analysis can inform treatment decisions for the management of moderate-to-severe psoriasis |
Introduction
Psoriasis is a common, chronic inflammatory disease characterized by well demarcated, red, scaly plaques on the skin as well as numerous possible comorbidities [1, 2]. For patients with moderate-to-severe psoriasis, treatment often includes oral medications, biologics, and/or (less frequently) phototherapy [3]. Although biologics are approved as monotherapy for the treatment of moderate-to-severe psoriasis, other systemic medications are often used as add-on medications in real-world practice [4]. Studies have shown that concomitant use of methotrexate with biologics such as etanercept [5,6,7] or adalimumab [7] increases the efficacy of these agents compared with biologic monotherapy in patients with moderate-to-severe psoriasis.
Adherence is the extent to which a patient takes a medication as prescribed while medication persistence is characterized by the duration of time a patient remains on a medication from initiation of therapy to discontinuation [8]. Continued adherence and persistence are key to achieving satisfactory disease control and improved quality of life. Non-adherence and non-persistence in psoriasis treatment management lead to increased risk of recurrence and treatment failure, as well as increased health-care costs [8, 9]. Therefore, understanding adherence and persistence differences in psoriasis treatments in real-world settings is essential in informing decisions of patients, providers, and payers when considering biologic therapies. Currently, there are limited data comparing the adherence and effectiveness of using biologics as monotherapy.
Ixekizumab (IXE) is a high-affinity monoclonal antibody that selectively targets interleukin (IL)-17A and is Food and Drug Administration (FDA) and European Medicines Agency (EMA) approved for the treatment of moderate-to-severe plaque psoriasis, active psoriatic arthritis, and spondylarthritis. The objective of the current retrospective analysis was to compare persistence, adherence, and monotherapy days among patients with psoriasis treated with IXE versus those treated with other commonly prescribed biologics, including secukinumab (SEC), ustekinumab (UST), adalimumab (ADA), and etanercept (ETN), using an administrative claims database. At the time this study was conducted, data were insufficient to include IL-23 inhibitors in the analysis.
Methods
Research Design and Data Source
This is a retrospective cohort analysis aiming to characterize patients with psoriasis treated with biologics including IXE, SEC, UST, ADA, and ETN using IBM Marketscan® Research Databases (The Commercial and Medicare Supplemental Database, supplemented with more recent data by the Early View Database). IBM Marketscan® Research Databases are collections of de-identified claims data for commercially insured people in the US capturing patient-level data on demographics, healthcare resource utilization, expenditures, and enrollment across inpatient, outpatient, prescription drug, and carve-out services. No institutional review board approval was required as the statistical analyses utilized a de-identified secondary data source.
Sample Selection
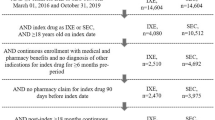
Selected patients received newly initiated biologics (IXE, SEC, UST, ADA, or ETN) between July 1, 2016, and July 1, 2018, from IBM MarketScan® Databases. The index date was set at the date of the first claim of the index biologic. The index biologic was the first biologic claimed during the study window. Patients were assigned to the IXE, SEC, UST, ADA, or ETN cohort based on the medication claim on the index date. Patients were additionally required to have continuous enrollment with medical and pharmacy benefits for at least 6 months before biologic initiation (“pre-index”) and a minimum of 12 months after the index date (“post-index”). Patients included in the cohort had at least one inpatient or two outpatient psoriasis diagnosis claims (at least 21 days apart) (ICD-9-CM codes 696.1 × or ICD-10 codes L40.0–L40.4 or L40.8). At least one of the PsO diagnosis claims occurred pre-index. Patients had to be at least 18 years of age at their index date. Patients diagnosed with other autoimmune diseases including ankylosing spondylitis, rheumatoid arthritis, Crohn’s disease, or ulcerative colitis during the pre-index period were excluded to avoid inclusion of patients taking biologics for other disease than psoriasis.
Outcomes
Patient demographic and clinical characteristics along with treatment patterns were reported for each index biologic at baseline.
Adherence to each index biologic was measured by the proportion of days covered (PDC), defined by the sum of the number of days covered on the index medication divided by the follow-up days; overlapping days between claims were truncated to avoid potential double-counting. Patients were deemed to be highly adherent if they had PDC ≥ 80%. Monotherapy was defined as days of the index medication without concomitant systemic, phototherapy, or other biologics. PDCs of monotherapy were also reported for each index biologic. PDC of concomitant medication, defined as the use of any systemic medications including other biologics and phototherapy during the post-period, was reported.
Persistence was measured by calculating the time from index date to treatment interruption. Patients were persistent if they received continuous treatment with the same study drug without a prescription gap of > 60 days (between a prescription’s last day of supply and date of next refill) from the index date to the end of continuous enrollment or the end of the study period.
Statistical Analysis
The patient populations for this data analysis were [1] those with prior 6-month eligibility (pre-index) and post-index 1-year follow-up and [2] prior 6-month eligibility (pre-index) and post-index > 1-year follow-up. Inverse probability of treatment weighting (IPTW) was applied before comparison to address cohort imbalances in patient demographic characteristics (index age, gender, geographic region, health plan type), clinical characteristics in the baseline period (Deyo-Charlson comorbidity index and comorbid conditions, including anxiety, cerebrovascular disease, depression, diabetes, hyperlipidemia, multiple sclerosis, obesity), baseline biologic/systemic/topical/phototherapy use, and prior 6-month total health care costs. The PDC and percent of patients achieving ≥ 80% PDC on adherence, monotherapy, and concomitant medication were compared between treatments using weighted t-tests and weighted logistic regression models.
Kaplan-Meier curves were used to estimate the observed time to the first medication gap of > 60 days, and weighted Cox proportional hazards model was used to obtain the hazard ratio (HR) of IXE versus other biologics on medication discontinuation. Sensitivity analyses on adherence and persistence were also conducted with further adjustments in the respective tests using the same variables as those for IPTW.
Results
Demographic and Baseline Characteristics
Patient demographic and baseline characteristics are provided in Table 1. A total of 7797 patients met the inclusion criteria, of which 742 initiated IXE, 3592 ADA, 524 ETN, 1027 SEC, and 1912 UST. Mean age across biologic treatment cohorts ranged from 46.2 years (ADA) to 49.3 years (IXE). Percentage of females across the biologics ranged from 44.2% (IXE) to 48.5% (ETN). Most biologic users resided in the South (46.7%–51.1%) and were covered by commercial insurance (92.7%–97.0%). A higher proportion of patients receiving IXE had previous biologic therapies (50.3%) versus other biologics (ADA: 9.1%, ETN: 10.9%, SEC: 33.9%, UST: 19.7%).
Persistence to Biologics
1-year Post-Index Period
Observed median time in days (95% CI) to treatment persistence for IXE was overall higher when compared to all of the other biologics combined (358 [353–364] vs. 258 [247–269]) and when compared to each biologic evaluated separately: ADA (300 [285–314]), ETN (181 [168–200]), SEC (328 [302–346]), and UST (176 [155–193]) (Fig. 1).
Time to discontinue the index biologic. Days to discontinue the index biologics in the 1-year post-index period of IXE, all other biologics, ADA, ETN, SEC, and UST. Observed data are presented. All includes SEC, UST, ADA, and ETN. ADA adalimumab, CI confidence interval, ETN etanercept, IXE ixekizumab, SEC secukinumab, UST ustekinumab
Patients treated with IXE were less likely to be non-persistent to therapy when compared with all of the other biologics combined (HR: 0.72, p < 0.001) and when compared with each biologic individually: ADA (HR: 0.82, p < 0.001), ETN (HR: 0.50, p < 0.001), SEC (HR: 0.83, p < 0.001), and UST (HR: 0.55, p < 0.001) (Fig. 2a).
Medication persistence. HR for IXE versus other biologics to discontinue the index biologics in the post 1-year follow-up (a), and in the minimum 1-year follow-up and maximum 3-year follow-up (b). All includes SEC, UST, ADA, and ETN. ADA adalimumab, ETN etanercept, HR hazard ratio, IXE ixekizumab, SEC secukinumab, UST ustekinumab
More than 1-Year Follow-Up
Consistent with the 1-year follow-up results, among patients with a minimum of 1 year and up to 3-year follow-up, observed median time in days (95% CI) to treatment persistence was higher in patients receiving IXE when compared to all of the other biologics combined (414 [370–474] vs. 259 [249–270]) and when compared with each biologic evaluated separately: ADA (301 [286–315]), ETN (181 [168–200]), SEC (335 [307–363]), and UST (176 [155–193]) (Supplementary Fig. 1).
Patients treated with IXE were less likely to be non-persistent compared with other biologics combined (HR: 0.75, p < 0.001), ADA (HR: 0.83, p < 0.001), ETN (HR: 0.56, p < 0.001), SEC (HR: 0.83, p < 0.001), and UST (HR: 0.62, p < 0.001) (Fig. 2b).
Sensitivity analyses with further model adjustments after IPTW confirmed the findings on all persistence findings.
Medical Adherence to Biologics
One-Year Post-Index Period
At 1-year, mean adherence, measured as PDC, was significantly (p < 0.001) higher for patients taking IXE compared with all biologics combined (0.66 vs. 0.60, p < 0.001), ADA (0.66 vs. 0.62), ETN (0.67 vs. 0.50), and UST (0.66 vs. 0.57) (Table 2). There were no statistically significant differences in adherence measured by PDC between IXE and SEC (0.67 vs. 0.64, p = 0.055) at 1-year follow-up. Patients taking IXE had a statistically (p < 0.001) greater level of high adherence compared to all biologics combined (43.6% vs. 34.0%), ADA (43.2% vs. 38.7%), ETN (43.6% vs. 18.0%), SEC (44.1% vs. 37.8%), and UST (43.9% vs. 27.6%) as measured by PDC 80% or higher (Table 2).
More than 1-Year Follow-Up
In patients with at least 1 year and up to 3 years of follow-up, adherence measured by PDC was significantly (p < 0.001) better in patients treated with IXE compared with all combined biologics (0.53 vs. 0.46), and when compared with individual biologics ADA (0.53 vs. 0.46), UST (0.53 vs. 0.46), and ETN (0.53 vs. 0.33) and with SEC (0.53 vs. 0.51, p < 0.05) (Table 2). A significantly higher percentage of patients (p < 0.001) taking IXE was highly adherent (PDC 80% or higher) compared with all biologics combined (22.0% vs. 17.0%) and when compared to individual biologics ADA (22.7% vs. 18.3%), ETN (22.5% vs. 8.3%), and UST (21.4% vs. 15.8%) (Table 2). There were no statistically significant differences in high adherence (PDC ≥ 80%) between IXE and SEC (22.5% vs. 20.6%, p = 0.175) after 1-year and up to 3 years of follow-up.
Monotherapy and Concomitant Medication
Among patients with 1-year follow-up, the PDC on monotherapy was significantly (p < 0.001) higher in patients taking IXE compared with all biologics combined (0.66 vs. 0.59) and compared with individual biologics: ADA (0.66 vs. 0.61), ETN (0.66 vs. 0.48), and UST (0.66 vs. 0.56) and with SEC (0.66 vs. 0.63, p < 0.05) as well (Table 2). Similar results were observed for patients with 1–3 years of follow-up. Sensitivity analyses with further model adjustments after IPTW confirmed the findings on adherence.
At 1-year post follow-up, concomitant medication use was significantly shorter in patients treated with IXE compared with all biologics combined and when compared with ADA and ETN but not with SEC and UST (Table 2). However, as the follow-up extended from 1 to 3 years, IXE showed significantly shorter concomitant medication use than all other biologics combined and compared to ADA, ETN, SEC, and UST, respectively (Table 2).
Discussion
Psoriasis has a significant impact on patients' lives, and newer biologic treatments for patients with moderate-to-severe disease have greatly improved quality of life and have revolutionized the management of psoriasis. However, poor adherence and persistence to chronic biologic therapy can lead to suboptimal health outcomes. Improving adherence to and persistence on biologics is vital in ensuring patients realize optimum benefits from those treatments and in reducing the health care costs [10, 11]. Here, in a real-world retrospective analysis, we demonstrated patients with psoriasis who were prescribed IXE were significantly more persistent, adherent, and remained longer on monotherapy compared to those prescribed other commonly prescribed biologics. In addition, we showed that patients with psoriasis demonstrated better persistence on drug for up to 3 years of follow-up than with other commonly prescribed biologics. In analysis with at least 1 year and up to 3 years of follow-up, by the end of year 3, most patients were already censored because of having < 3 years of follow-up or discontinued the medication. As a result, the cumulative probability time to discontinue the index biologic curves converged.
These results are consistent with those of a recent claims analysis evaluating the adherence and/or persistence of IXE compared with other biologics [12,13,14]. Two prior studies examined the real-world treatment patterns of patients with psoriasis treated with IXE versus ADA [12] and IXE versus SEC, [13] using the same MarketScan® databases. The first study found patients treated with IXE had longer persistence and higher adherence and were less likely to discontinue or switch their treatment compared with patients receiving ADA [12]. In the second study comparing two IL-17A inhibitors, IXE and SEC, it was shown that patients treated with IXE had longer persistence, higher adherence, and lower discontinuation than SEC users [13]. In contrast to the present study, these two studies do not have data on monotherapy versus concomitant medication use during treatment with these biologics, and comparisons between IXE and ETN or UST were not included [12, 13].
In real-world settings, patients with moderate-to-severe psoriasis are often receiving topical corticosteroids and systemic medications in combination with biologics [4]. A study of patients with moderate-to-severe psoriasis evaluating the concomitant use of methotrexate with ETN or ADA compared with each biologic in monotherapy demonstrated an increased response rate when methotrexate was added [7]. In addition, the jointly developed American Academy of Dermatology and National Psoriasis Foundation guidelines recommend the use of topical corticosteroids alone or in combination with biologics to augment efficacy [4]. Our study showed that patients remained longer on IXE as a monotherapy compared to all other commonly prescribed biologics combined and compared to each biologic considered separately. Our findings suggest that patients with moderate-to-severe psoriasis receiving IXE do not require additional concomitant therapy to the same extent as required by other biologics. Our study confirms prior observations that real-world patients with psoriasis are more likely to adhere to a treatment plan when early positive results are noted.
In the treatment of psoriasis, prior biologic use could be predictive of lower persistence [15,16,17,18]. In our analysis, patients receiving IXE were more likely to be bio-experienced compared to the other biologics, but they were still more persistent on and adherent to treatment and remained on monotherapy longer compared to those other commonly prescribed biologics in this study.
Limitations of this study are typical of retrospective analyses using claims data and include the potential for inaccurate coding or omissions and lack of clinical details from the patient’s medical chart (i.e., disease severity, patient comorbidities, and patient body weight) that may influence the treatment used or ability to accurately calculate dosage. In addition, claims data do not capture patient behaviors, and prescription fill/refill dates were assumed to reflect how the patient took the medication. Finally, this analysis is limited to patients with commercial insurance; therefore, results cannot be extrapolated to other patients. The results must therefore be interpreted with these limitations in mind. The main strength of this analysis was the use IBM MarketScan® databases, which provide data across the US. The large sample size analyzed provides robustness to the real-world evidence and helps make the results more applicable to routine clinical practice settings.
Conclusion
In summary, among patients with moderate-to-severe psoriasis, IXE-treated patients were more adherent, had longer persistence, and remained longer on monotherapy treatment than did patients treated with other commonly prescribed biologics. The findings from this analysis may help inform clinicians when making treatment decisions for the management of moderate-to-severe psoriasis in the real world. Further studies are needed to identify underlying factors that can have an influence on adherence and persistence such as gender, age, loss of efficacy, posology, or copayment amount.
References
Boehncke WH, Schon MP. Psoriasis Lancet. 2015;386(9997):983–94.
Leonardi C, Matheson R, Zachariae C, Cameron G, Li L, Edson-Heredia E, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012;366(13):1190–9.
Kaushik SB, Lebwohl MG. Psoriasis: Which therapy for which patient: Psoriasis comorbidities and preferred systemic agents. J Am Acad Dermatol. 2019;80(1):27–40.
Menter A, Strober BE, Kaplan DH, Kivelevitch D, Prater EF, Stoff B, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Gottlieb AB, Langley RG, Strober BE, Papp KA, Klekotka P, Creamer K, et al. A randomized, double-blind, placebo-controlled study to evaluate the addition of methotrexate to etanercept in patients with moderate to severe plaque psoriasis. Br J Dermatol. 2012;167(3):649–57.
Zachariae C, Mork NJ, Reunala T, Lorentzen H, Falk E, Karvonen SL, et al. The combination of etanercept and methotrexate increases the effectiveness of treatment in active psoriasis despite inadequate effect of methotrexate therapy. Acta Derm Venereol. 2008;88(5):495–501.
Takeshita J, Wang S, Shin DB, Callis Duffin K, Krueger GG, Kalb RE, et al. Comparative effectiveness of less commonly used systemic monotherapies and common combination therapies for moderate to severe psoriasis in the clinical setting. J Am Acad Dermatol. 2014;71(6):1167–75.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Wang W, Qiu Y, Zhao F, Zhang F. Poor medication adherence in patients with psoriasis and a successful intervention. J Dermatolog Treat. 2019;30(6):525–8.
Seale L, Cardwell LA, Feldman SR. Adherence to biologics in patients with psoriasis. Expert Rev Clin Immunol. 2018;14(2):155–61.
Blauvelt A, Shi N, Burge R, Malatestinic WN, Lin CY, Lew CR, et al. Comparison of Real-World Treatment Patterns Among Psoriasis Patients Treated with Ixekizumab or Adalimumab. Patient Prefer Adherence. 2020;14:517–27.
Blauvelt A, Shi N, Burge R, Malatestinic WN, Lin CY, Lew CR, et al. Comparison of real-world treatment patterns among patients with psoriasis prescribed ixekizumab or secukinumab. J Am Acad Dermatol. 2020;82(4):927–35.
Hendrix N, Marcum ZA, Veenstra DL. Medication persistence of targeted immunomodulators for plaque psoriasis: A retrospective analysis using a US claims database. Pharmacoepidemiol Drug Saf. 2020;29(6):675–83.
Papp KA, Gordon KB, Langley RG, Lebwohl MG, Gottlieb AB, Rastogi S, et al. Impact of previous biologic use on the efficacy and safety of brodalumab and ustekinumab in patients with moderate-to-severe plaque psoriasis: integrated analysis of the randomized controlled trials AMAGINE-2 and AMAGINE-3. Br J Dermatol. 2018;179(2):320–8.
Menter A, Papp KA, Gooderham M, Pariser DM, Augustin M, Kerdel FA, et al. Drug survival of biologic therapy in a large, disease-based registry of patients with psoriasis: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Eur Acad Dermatol Venereol. 2016;30(7):1148–58.
Warren RB, Smith CH, Yiu ZZN, Ashcroft DM, Barker J, Burden AD, et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the british association of dermatologists biologic interventions register (BADBIR). J Invest Dermatol. 2015;135(11):2632–40.
Ruiz Salas V, Puig L, Alomar A. Ustekinumab in clinical practice: response depends on dose and previous treatment. J Eur Acad Dermatol Venereol. 2012;26(4):508–13.
Acknowledgements
Funding
This work and the journal’s Rapid Service and Open Access Fees were supported by Eli Lilly and Company.
Medical Writing
Elsa Mevel, PhD, provided writing and editorial assistance. Funding for this assistance was provided by Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the analysis and interpretation of data and provided critical revisions of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Prior Presentation
Portions of this work were presented at the 2020 American Academy of Dermatology annual Meeting, June 12–14, 2020.
Disclosures
C. Leonardi has been a consultant, and/or investigator, and/or has received honoraria/other financial benefit from: AbbVie, Amgen, Boehringer Ingelheim, Celgene, Corrona, Dermira, Eli Lilly and Company, Galderma, Janssen, Leo Pharma, Merck, Novartis, Pfizer, Sandoz, Sienna Tribute, UCB Pharma, and Vitae Pharmaceuticals. B. Zhu, W. N. Malatestinic, W. J. Eastman, J. Guo, M. J. Murage, C. Kar-Chan Choong, and R. Burge are employees and/or shareholders of Eli Lilly and Company. A. Blauvelt has served as a scientific adviser and/or clinical study investigator for: AbbVie, Abcentra, Aligos, Almirall, Amgen, Arcutis, Arena, Aslan, Athenex, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, Eli Lilly and Company, Evommune, Forte, Galderma, Incyte, Janssen, Landos, Leo, Novartis, Pfizer, Rapt, Regeneron, Sanofi Genzyme, Sun Pharma, and UCB Pharma.
Compliance with Ethics Guidelines
This article is based administrative data claims for commercially insured people in the U.S and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The datasets used during the current study are available from IBM MarketScan® Databases.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leonardi, C., Zhu, B., Malatestinic, W.N. et al. Real-World Biologic Adherence, Persistence, and Monotherapy Comparisons in US Patients with Psoriasis: Results from IBM MarketScan® Databases. Adv Ther 39, 3214–3224 (2022). https://doi.org/10.1007/s12325-022-02155-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02155-9