Abstract
Chronic inflammatory diseases (CIDs) represent a substantial clinical and economic burden to patients, providers, payers and society overall. Biologics, such as tumor necrosis factor inhibitors (TNFi), have emerged as effective treatment options for patients with CIDs. However, the therapeutic potential of biologics is not always achieved in clinical practice, with results from studies examining the use of biologics in real-world settings suggesting lower levels of treatment effectiveness compared with clinical trial results. Using a targeted approach, this literature review demonstrates that compliance and persistence with biologic therapy is suboptimal and that this has implications for both clinical outcomes and treatment costs. The review identified a variety of predictors of treatment compliance and persistence, including increased age, female gender, presence of comorbidities, increased disease activity, longer disease duration, smoking, increased body mass index, higher biologic treatment dose, higher treatment cost and lower health-related quality-of-life scores. Patients often cited factors associated with medication delivery as a reason for non-compliance and non-persistence, and device-related improvements to treatment delivery were associated with higher rates of compliance and persistence. The articles identified in this review provide insights that have the potential to help guide the development of new solutions to improve disease management and optimize treatment regimens. This has the potential to benefit patients’ health by improving clinical outcomes and to reduce the burden to society by limiting the economic impact of patients’ disease.
Funding
UCB Pharma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic inflammatory diseases (CIDs) are a group of related autoimmune diseases that include rheumatoid arthritis (RA), axial spondyloarthritis (axSpA), inflammatory bowel disease (IBD), juvenile idiopathic arthritis (JIA), psoriatic arthritis (PsA), psoriasis (PsO) and Crohn’s disease (CD). Together CIDs affect between 5 and 7% of the Western population [1] and represent a significant economic and societal burden [2]. As a consequence of the inflammation and loss of function of the affected tissue, these conditions are associated with chronic disability, significant pain and reduced functional impairment (in arthritic conditions). Patients require long-term therapy and often have significantly reduced productivity and quality of life, increased morbidity and premature mortality [2].
Biologics have emerged as effective therapeutic options for patients with CIDs who fail to respond to first-line treatments such as methotrexate [3]. For example, clinical trials examining the efficacy and safety of tumor necrosis factor inhibitors (TNFi) have demonstrated that disease remission is a realistic target for some of these patients [3, 4]. It is difficult to compare randomized-controlled trials (RCTs) with real-world studies since measures of effectiveness may not be the same, co-therapy changes are frequent, therapy patterns are not dictated by protocols, and patient heterogeneity in real-world studies results in broader populations under medication. However, the biologic therapeutic potential observed in clinical trials is rarely achieved in clinical practice, with results from studies examining the use of biologics in real-world settings suggesting lower levels of treatment effectiveness [5, 6]. In real-world clinical settings, recommended treatment regimens are not always adhered to. This may be due to a variety of factors including physicians tailoring therapy to patients’ needs, for example, guided treatment withdrawal [7, 8]; however, a number of studies have also reported suboptimal patient compliance and persistence with biologic therapy, which may reduce the clinical effectiveness of the prescribed treatment [9,10,11].
Generally, comparing studies is challenging as a plethora of definitions are used to describe compliance and persistence, and study designs often vary. There is evidence that factors associated with patients’ experience during treatment, and not solely those linked to the efficacy and safety of a drug, may play a role. For example, biologics are often administered by self-injection, which can be associated with significant patient anxiety [12, 13]. Although there are clear challenges to understanding the causes leading to non-compliance and non-persistence, understanding the driving factors represents a potential opportunity to reduce the burden associated with CIDs by maximizing treatment effectiveness, ensuring the full efficacy potential of biologics is achieved.
Here we report the findings from a review of the available literature on compliance and persistence with biologic therapies across multiple conditions including axSpA, CD, IBD, JIA, PsA, PsO and RA. The aims of this review were to: (1) provide an overview of compliance and persistence with biologic therapeutics in the context of CIDs, aligning the studies to predefined definitions of persistence and compliance, (2) examine the impact of any treatment-related factors identified as contributing to non-compliance and non-persistence, focusing on the impact of using different self-injection devices and patient-support services and (3) review the clinical and economic consequences of suboptimal treatment compliance and persistence.
Methods
Search Strategy and Study Selection
Two targeted literature searches were performed. The first was designed to provide a broad overview of the comparative landscape of anti-TNF biologic therapies used to treat CIDs. Electronic searches were performed in PubMed/MEDLINE for indexed literature published between January 2000 and October 2015. The search strategy identified literature reporting economic, clinical and health-related quality of life (HRQoL) outcomes associated with the use of different biologic therapies. The search terms used included the specific disease indications (RA, CD, PsA, AS, axSpA, PsO, JIA, pediatric CD and uveitis), economic outcomes (e.g., ‘resources’, ‘costs’), and clinical and HRQoL outcomes (e.g., ‘ASAS20’, ‘BASMI’, ‘IBDQ’, ‘work impairment’). Electronic searches were complemented by a review of conference proceedings [European League Against Rheumatism (EULAR), American College of Rheumatology (ACR), International Society for Pharmacoeconomics and Outcomes Research (ISPOR), European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCEPP)], ClinicalTrials.gov and therapy manufacturers’ websites from the preceding 2 years.
The second targeted literature search was designed to identify any additional studies published after 2015 that reported data on the impact of devices on compliance and persistence and on the clinical and economic outcomes related to non-compliance and non-persistence. The search was conducted in OVID (including MEDLINE, EMBASE, CRD, Cochrane, Econlit and the ACP Journal Club) for indexed literature published between January 2015 and May 2017. In addition, the bibliographies of key review articles were manually reviewed to supplement the electronic searches.
For both searches, English language studies were included if they could be described as real-world data studies, such as observational studies using databases and registries, pragmatic clinical trials, phase IV trials/post-marketing open-label/'off-label' studies, patient and population surveys, chart reviews or economic models based on real-world data. Once the selection criteria had been applied to all identified studies, included publications were grouped according to their reported outcomes as described below.
Definitions Used to Align Measures of Persistence and Compliance
The definitions used by researchers to define compliance and persistence, the use of different data sources (e.g., prescription data, patient self-reported measures and doctors’ observations) and methods used to calculate rates, and the geographic location of the health system can all influence the reported values of compliance and persistence.
For this review, all included studies were examined to identify the methods used to calculate rates of compliance and persistence. These methods were compared with the definitions recommended by ISPOR, described below, to categorize the studies as compliance- or persistence-focused as appropriate: [14]
-
Compliance: The extent to which a patient acts in accordance with the prescribed interval and dose of a dosing regimen.
-
Persistence: The duration of time from initiation to discontinuation of therapy.
Both compliance and persistence are calculated using a number of different methods. Compliance can be calculated using the Medication Possession Ratio (MPR, the proportion of days’ supply for all fills of a drug in the total medication period) and/or the Proportion of Days Covered (PDC; defined as the proportion of days a patient is ‘covered’ by their drug supply in the medication period). In the event of overlapping refills, PDC will not change while the MPR value will be higher. MPR and PDC data do not necessarily take into account when patients are following their treatment regimen or how optimal the regimen is, but rather whether they are in possession of treatment. Consequently, they may underestimate the rates of non-compliance [15].
Persistence can be described using either the continuation rate (also known as the retention rate and defined as the proportion of patients adhering to a given treatment in a given time) [16] or drug survival (defined as the number of days individual patients maintained treatment) [14].
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Results
Search Results
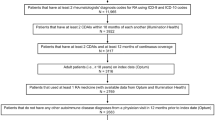
The initial literature search identified 7823 studies of potential interest via PubMed, 6857 documents from conference proceedings and 673 clinical trials. Following the final application of the eligibility criteria (Table 1), 125 peer-reviewed studies (Supplementary Figure S1), 109 conference abstracts/posters, and 20 ongoing or completed clinical trials, identified from ClinicalTrials.gov, were included for review. The literature review update identified an additional 826 publications of potential interest via PubMed, Embase, Cochrane, CRD, Econlit, ACP Journal Club and conference proceedings. From this search, a further 17 relevant studies were identified and included for review (Supplementary Figure S2).
Overview of Compliance and Persistence with Biologic Therapy
In total, 19 publications reporting compliance data, and 110 publications reporting persistence data were identified during the first literature search.
The majority of studies reported on the treatment of RA patients with conventional biologics such as etanercept, adalimumab and infliximab. The methodology, study designs, patient populations and time points used to measure compliance and persistence were highly inconsistent, leading to a wide range of reported estimates. Across all the literature reviewed, rates of persistence and compliance varied considerably (Supplementary Table S1). Of the studies reviewed, approximately one-third (n = 32) provided information on previous biologic experience.
Compliance with TNFi Therapy
Nineteen studies were identified reporting compliance data (summarized in Supplementary Table S1). The studies identified covered RA and CD patients treated with infliximab, adalimumab, golimumab or etanercept. Of these studies, 13 were conducted in the US and used data from large administrative claims databases. A summary of the reported compliance results over 1 year is provided in Table 2.
The methodology used to calculate compliance also differed across studies, which may have contributed to the variable results observed. Seven studies assessed compliance using the MPR or PDC by medication during the follow-up period [39, 41, 48,49,50,51], 1 assessed MPR using a fixed interval (365 days) as a denominator [41], and 2 studies used total days’ supply of the medication as numerator and total days in the study period as denominator [39]. Compliance rates from studies using the MPR ranged from 52%, when MPR was calculated using total number of days of medication supply divided by total number of days in the study period, to 88%, when calculated by summing the days’ supply value of the index treatment and dividing this amount by the sum of days between the index date and the most recent index treatment fill plus the days’ supply value of the last fill.
No studies were identified comparing compliance rates between TNFi-naïve and TNFi-experienced patients, and no clear trends in treatment compliance over time were identified.
Persistence with TNFi Therapy
Only 53/110 identified studies reporting persistence described the methods used to define persistence. These included studies using large administrative claims databases and registries, which generally provided definitions and methodology for analyzing treatment persistence. Of the studies that did provide this information, there was significant heterogeneity in the methods used. For example, non-persistence was calculated using a variety of thresholds to measure the treatment gap (i.e., the number of days a patient had to be off therapy after exhausting their supply of drug): 13 studies used a > 90-day treatment gap after a biologic prescription was exhausted [17,18,19,20,21,22,23,24,25,26,27,28,29], 6 studies used a > 60-day treatment gap [30,31,32,33,34,35], 3 studies used a > 45-day treatment gap [36,37,38], and 3 studies used a > 30-day treatment gap [39,40,41].
Approximately two-thirds (75/110) of studies reporting persistence data used administrative databases or registries. In Europe, persistence data were often reported from large registry-based analyses; rates were generally shown to be highest in the UK and France, and lowest in Nordic countries, and ranged from 70–86% at 1 year of treatment [23, 42]. In the US, data were more often from large administrative claims databases and persistence rates were lower, ranging from 46–73% at 1 year (Table 3) [43,44,45,46].
Generally, the rates of persistence were higher in biologic-naïve patients, and there was no clear evidence to suggest a difference between switching within class (i.e., to another TNFi) or switching to a biologic with a different mechanism of action [47].
Factors Leading to Suboptimal Persistence and Compliance
Cox regression modeling has been used in a number of studies to identify factors that may predict rates of treatment persistence. A variety of factors were identified as potentially predictive of suboptimal treatment persistence. These included increased age, female gender, presence of a comorbidity, high disease activity at diagnosis, longer disease duration, smoking, increased body mass index, higher treatment dose, higher treatment cost and lower HRQoL scores [17,18,19,20, 22, 26, 28, 39, 52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Several studies have identified a variety of patient-reported reasons for non-compliance and non-persistence. Reasons have included forgetfulness, intentional non-compliance, supply issues, patient misunderstanding of their treatment regimen, medication ineffectiveness, cost/affordability of treatment, a lack of motivation or social support, fear of self-injection and reduced hand dexterity [12, 15, 73,74,75].
Impact of Drug Delivery Devices and Patient Support Services on Compliance and Persistence
Patients often cited factors associated with medication delivery as a reason for non-compliance and non-persistence. Four studies utilizing various methodologies examined the effect of treatment self-administration with various delivery devices on compliance and persistence (Table 4), reporting results indicating that self-injection devices may offer solutions to some of the reasons for non-compliance and non-persistence.
Switching from a prefilled syringe to an auto-injector was associated with improved treatment compliance and persistence; patients with chronic diseases reported that auto-injection devices were preferable over prefilled syringes because they were less painful and simpler to use [74, 76, 77]. In one study, a 30% increase was observed in the number of patients self-administrating medication after switching to an auto-injector, which in turn led to a decrease in the proportion of patients requiring outpatient visits or additional assistance [76]. Two single-center studies reported similar results in patients switching from a prefilled syringe to an auto-injection pen; the first enrolled 55 patients and demonstrated 100% persistence with an adalimumab auto-injection pen over 8 weeks, while the second enrolled 104 patients and demonstrated > 95% compliance with an etanercept auto-injection pen over 8 weeks [74, 76]. Similar results were also seen with golimumab. The GO-MORE trial, reporting the use of the GOL SmartJect® (Janssen Biotech Inc, Horsham, PA, USA) auto-injection device in RA patients, reported that high persistence and compliance were maintained throughout the study, with 91.7% of patients completing 6 months of treatment and > 80% of patients adhering to the recommended monthly dosing frequency [77].
One paper was identified highlighting the benefits of patient support services on treatment compliance (Table 4). The study described the impact of patient enrollment on myHUMIRA® (AbbVie, North Chicago, IL, USA) patient support program (PSP) and indicated that patients enrolled in the PSP showed greater intent to comply with treatment, had higher treatment satisfaction and had greater perception of treatment benefits. However, it must be noted that patients enrolled voluntarily in the PSP; thus, compliance results are likely to be more favorable [78]. No studies reporting the impact of patient support services on treatment persistence with TNFi therapy were found during the review.
Clinical and Economic Consequences of Treatment Non-Compliance and Non-Persistence
Patient non-compliance and non-persistence have been shown to have a significant impact on treatment outcomes from both a clinical and economic perspective. Suboptimal treatment compliance and persistence are associated with increased morbidity and mortality, as well as suboptimal outcomes in terms of treatment benefit and symptomatic improvement. In turn, this leads to higher healthcare costs and more frequent outpatient visits [10, 14].
Multiple studies identified during the review indicated that suboptimal persistence and compliance were associated with lower clinical effectiveness (Table 5). For example, one study demonstrated that RA patients who received TNFi, and had higher persistence rates, had significantly lower disease activity scores (DAS [28]) than those with lower persistence rates [79]. Another study demonstrated that high compliance rates were associated with a greater reduction in DAS28 scores over 6 months of subcutaneous TNFi therapy [80].
Overall, evidence suggests that suboptimal compliance and persistence are associated with higher costs and increased burden on healthcare services (Table 5). In studies of patients with CD, suboptimal compliance was found to be associated with significantly higher rates of hospitalization and surgery, more emergency room visits, significantly longer hospital stays and higher healthcare costs in comparison with compliant patients [81,82,83]. A Swedish retrospective registry study demonstrated that the healthcare resource utilization cost in AS, PsA and RA non-persistent patients was higher following a period of treatment non-persistence than at the start of therapy, whereas reduced healthcare resource costs were seen in persistent patients [34].
During first-line biologic treatment, non-persistent patients with RA had significantly higher healthcare costs (hospitalizations, specialist care, etc.); patients undergoing a treatment switch to a second TNFi following a failure to respond to the first incurred the highest 1-year total healthcare costs, and the treatment costs for patients switching from the initial treatment during the first year of follow-up were higher than for patients who did not switch [84]. When comparing switching to another TNFi as opposed to switching out of class, all-cause costs were higher in patients switching to a non-TNFi biologic DMARD compared with an alternative biologic TNFi [84]. Overall, RA patients with high rates of persistence (> 80%) had higher total healthcare costs, driven by higher pharmacy costs; however, the total non-pharmacy costs, including in- and outpatient visits and laboratory services, were lower than costs reported for patients with persistence rates of < 80% (Table 5) [85, 86].
Discussion
This targeted literature review examined treatment compliance and persistence and their drivers in patients undergoing biologic treatment across a number of CIDs to understand the role of different treatment-related factors and the potential consequences of suboptimal compliance and persistence. In the majority of studies, the terms compliance and persistence were mixed without adequate description of the methodology used in the analyses, making interpretation of the results very difficult. In studies that did describe the methodology, notable heterogeneity in the methods used to measure treatment persistence and compliance was identified. Furthermore, the data sources used varied significantly from study to study and were often associated with specific limitations or biases. For example, registries were reliant on doctors’ notes that were based on patient self-reported data on drug intake, prescription data did not necessarily take into account the doctor-prescribed dose, and studies where patients were recruited from routine clinical practice generally had a small sample size with low geographic representativeness.
When looking at geographic patterns, persistence rates to prescribed biologics were higher in the UK and France than in Nordic countries, and EU studies generally reported higher rates than US studies. Within the EU, there are variations between country guidelines for the management of CIDs, for example, the approach to dose optimization and tapering differs from country to country. Differences also exist in the local availability of biologics and in the type of practice or specialist (e.g., dermatologist, gastroenterologist or rheumatologist) prescribing treatments for these indications, which may explain some of the differences observed between countries. The lower levels of compliance and persistence reported in the US compared with the EU may be, in part, due to the lack of a national health insurance scheme in the US as well as due to the key differences in data sources and data collection methods.
The review also identified papers showing that patients who cycle through multiple biologic therapies incur higher costs and become less responsive to treatment [84, 86]. Therefore, in the context of chronic diseases, it is beneficial to both individual patients and health systems to optimize patient journeys to ensure patients can cope with their treatment and remain compliant and persistent so as to avoid frequent cycling of multiple treatment options.
Both qualitative and quantitative research methods were used to assess the impact of devices on compliance and persistence; no standard questionnaire or measurement was used to evaluate the device usability and acceptability, patients’ preferences and treatment satisfaction. These limitations made it challenging to synthesize data in an informative way, so it is difficult to review the general treatment experience and impact of treatment devices on compliance and persistence. Despite these challenges, this review identified a number of factors associated with treatment delivery that appear to influence compliance and persistence and so represent possible targets for future interventions. For example, a number of studies reported improvements in compliance and persistence following changes to the delivery device. Interventions, such as easing the route of medication administration through the use of auto-injection pen devices, providing support to patients to ensure they are able make informed decisions about their device choice to ensure it meets their specific needs, and device design improvements such as dose reminder functions were all associated with high compliance and persistence rates. General patterns were observed suggesting treatment non-compliance and non-persistence were associated with poorer clinical outcomes and higher treatment and healthcare costs, and compliant patients tended to experience fewer clinical events. However, this may be due to underlying differences in patients’ disease severity and comorbidities, which may confound the effect of non-compliance on outcomes.
While this review highlighted that compliance and persistence represent two key areas that, if improved, would positively impact treatment outcomes, there were several limitations. The aim of this review was to provide a broad overview of biologic therapy so a targeted approach was used to identify real-world studies reporting compliance and persistence data. Consequently, it is possible that studies may have been missed; however, as the heterogeneity of data reported within the literature limits any comparison of compliance and persistence between studies, it is unlikely that including any additional studies would impact the conclusions of this review. The majority of studies focused on treatment of patients with RA or AS using the conventional biologics, etanercept, adalimumab and infliximab, so may not be truly representative of treatment across other CIDs. Prescription orders from doctors are often unavailable in the databases used to calculate compliance, and so the reported rates may not take into account alternative dose regimens (in- or off-label). Therefore, compliance estimates are often blinded to dose escalation or dose down-tapering. Although this is unlikely to impact the results from patients starting treatment, they are common practices in these conditions and thus important determining factors [7, 8, 87]. Finally, data used to calculate compliance are mainly self-reported by patients and so are subject to self-reporting bias.
The results of this review clearly demonstrate that non-compliance and non-persistence are important public health considerations that affect the success of therapeutic treatment, disease remission and disease severity [88]. To understand what interventions can influence compliance and persistence, the methods used to report these measures first need to be aligned; without consistency in the methods and definitions used, it is difficult to draw comparisons between studies to fully understand patients’ reasons for non-compliance and non-persistence or understand individual barriers to optimal treatment use. Gaining a complete understanding of the intentional and unintentional causes driving non-compliance and non-persistence in individual patients will enable tailored solutions, such as improved devices, services and patient support interventions, to be developed to tackle each of these barriers. As persistence and compliance with biologic therapies have the potential to reduce the treatment costs and improve patients’ clinical outcomes and quality of life, this is an important area for future research.
Conclusions
Biologic therapy non-compliance and non-persistence have implications for both clinical and economic outcomes. A variety of factors contributing to treatment compliance and persistence were identified during this review of the available literature, and this evidence should be used to develop solutions to improve disease management and optimize treatment regimens. Tailoring treatment delivery devices and patient support services has the potential to improve compliance and persistence and so represents an important area for future research. This has the potential to benefit patients’ health by improving clinical outcomes and reducing the burden to society by limiting the economic impact of patients’ disease.
References
El-Gabalawy H, Guenther LC, Bernstein CN. Epidemiology of immune-mediated inflammatory diseases: incidence, prevalence, natural history, and comorbidities. J Rheumatol Suppl. 2010;85:2–10.
Jacobs P, Bissonnette R, Guenther LC. Socioeconomic burden of immune-mediated inflammatory diseases–focusing on work productivity and disability. J Rheumatol Suppl. 2011;88:55–61.
Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):644.
Nam J, Winthrop K, van Vollenhoven RF, et al. Current evidence for the management of rheumatoid arthritis with biological disease-modifying antirheumatic drugs: a systematic literature review informing the EULAR recommendations for the management of RA. Ann Rheum Dis 2010 (annrheumdis126573).
Sokka T, Hannonen P, Mäkinen H. Remission: a realistic goal in rheumatoid arthritis? Int J Clin Rheumatol. 2011;6(6):643.
Greenberg JD, Kishimoto M, Strand V, et al. Tumor necrosis factor antagonist responsiveness in a United States rheumatoid arthritis cohort. Am J Med. 2008;121(6):532–8.
Furst DE, Fleischman R, Kalden J, et al. Documentation of off-label use of biologics in Rheumatoid Arthritis. Ann Rheum Dis. 2013;72(Suppl 2):ii35–51.
Brezinski EA, Armstrong AW. Off-label biologic regimens in psoriasis: a systematic review of efficacy and safety of dose escalation, reduction, and interrupted biologic therapy. PLoS One. 2012;7(4):e33486. https://doi.org/10.1371/journal.pone.0033486
Harrold LR, Andrade SE. Medication adherence of patients with selected rheumatic conditions: a systematic review of the literature. Semin Arthritis Rheum. 2009;38(5):396–402.
World Health Organization. Adherence to long-term therapies: evidence for action. 2003. http://www.who.int/chp/knowledge/publications/adherence_report/en/. Accessed 3 Aug 2018.
Curtis JR, Bykerk VP, Aassi M, Schiff M. Adherence and persistence with methotrexate in rheumatoid arthritis: a systematic review. J Rheumatol. 2016;43(11):1997–2009.
UCB Data on File. Expert interviews, 2015, pp. 9.
Schiff M, Saunderson S, Mountian I, Hartley P. Chronic disease and self-injection: ethnographic investigations into the patient experience during treatment. Rheumatol Ther. 2017;4(2):445–63.
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
van Mierlo T, Fournier R, Ingham M. Targeting medication non-adherence behavior in selected autoimmune diseases: a systematic approach to digital health program development. PLoS One. 2015;10(6):e0129364.
Gisondi P, Tessari G, Di Mercurio M, Girolomoni G. Retention rate of systemic drugs in patients with chronic plaque psoriasis. Clin Dermatol. 2013;1(1):8–14.
Esposito M, Gisondi P, Cassano N, et al. Survival rate of antitumour necrosis factor-alpha treatments for psoriasis in routine dermatological practice: a multicentre observational study. Br J Dermatol. 2013;169(3):666–72.
Glintborg B, Ostergaard M, Krogh NS, et al. Clinical response, drug survival and predictors thereof in 432 ankylosing spondylitis patients after switching tumour necrosis factor alpha inhibitor therapy: results from the Danish nationwide DANBIO registry. Ann Rheum Dis. 2013;72(7):1149–55.
Leffers HC, Ostergaard M, Glintborg B, et al. Efficacy of abatacept and tocilizumab in patients with rheumatoid arthritis treated in clinical practice: results from the nationwide Danish DANBIO registry. Ann Rheum Dis. 2011;70(7):1216–22.
Glintborg B, Ostergaard M, Dreyer L, et al. Treatment response, drug survival, and predictors thereof in 764 patients with psoriatic arthritis treated with anti-tumor necrosis factor alpha therapy: results from the nationwide Danish DANBIO registry. Arthritis Rheum. 2011;63(2):382–90.
McErlane F, Foster HE, Davies R, et al. Biologic treatment response among adults with juvenile idiopathic arthritis: results from the British Society for Rheumatology Biologics Register. Rheumatology (Oxford). 2013;52(10):1905–13.
Saad AA, Ashcroft DM, Watson KD, Hyrich KL, Noyce PR, Symmons DP. Persistence with anti-tumour necrosis factor therapies in patients with psoriatic arthritis: observational study from the British Society of Rheumatology Biologics Register. Arthritis Res Ther. 2009;11(2):R52.
Zhu B, Edson-Heredia E, Gatz JL, Guo J, Shuler CL. Treatment patterns and health care costs for patients with psoriatic arthritis on biologic therapy: a retrospective cohort study. Clin Ther. 2013;35(9):1376–85.
Di Lernia V, Tasin L, Pellicano R, Zumiani G, Albertini G. Impact of body mass index on retention rates of anti-TNF-alfa drugs in daily practice for psoriasis. J Dermatolog Treat. 2012;23(6):404–9.
Zhang J, Xie F, Delzell E, et al. Impact of biologic agents with and without concomitant methotrexate and at reduced doses in older rheumatoid arthritis patients. Arthritis Care Res (Hoboken). 2015;67(5):624–32.
Glintborg B, Gudbjornsson B, Krogh NS, et al. Impact of different infliximab dose regimens on treatment response and drug survival in 462 patients with psoriatic arthritis: results from the nationwide registries DANBIO and ICEBIO. Rheumatology (Oxford). 2014;53(11):2100–9.
van den Reek JM, Zweegers J, Kievit W, et al. ‘Happy’ drug survival of adalimumab, etanercept and ustekinumab in psoriasis in daily practice care: results from the BioCAPTURE network. Br J Dermatol. 2014;171(5):1189–96.
Scire CA, Caporali R, Sarzi-Puttini P, et al. Drug survival of the first course of anti-TNF agents in patients with rheumatoid arthritis and seronegative spondyloarthritis: analysis from the MonitorNet database. Clin Exp Rheumatol. 2013;31(6):857–63.
Du Pan SM, Dehler S, Ciurea A, Ziswiler HR, Gabay C, Finckh A. Comparison of drug retention rates and causes of drug discontinuation between anti-tumor necrosis factor agents in rheumatoid arthritis. Arthritis Rheum. 2009;61(5):560–8.
Voulgari PV, Alamanos Y, Nikas SN, Bougias DV, Temekonidis TI, Drosos AA. Infliximab therapy in established rheumatoid arthritis: an observational study. Am J Med. 2005;118(5):515–20.
Zhang HF, Gauthier G, Hiscock R, Curtis JR. Treatment patterns in psoriatic arthritis patients newly initiated on oral nonbiologic or biologic disease-modifying antirheumatic drugs. Arthritis Res Ther. 2014;16(4):420.
Chastek B, Fox KM, Watson C, Gandra SR. Etanercept and adalimumab treatment patterns in psoriatic arthritis patients enrolled in a commercial health plan. Adv Ther. 2012;29(8):691–7.
Chastek B, Fox KM, Watson C, Kricorian G, Gandra SR. Psoriasis treatment patterns with etanercept and adalimumab in a United States health plan population. J Dermatolog Treat. 2013;24(1):25–33.
Dalen J, Svedbom A, Black CM, et al. Treatment persistence among patients with immune-mediated rheumatic disease newly treated with subcutaneous TNF-alpha inhibitors and costs associated with non-persistence. Rheumatol Int. 2016;36(7):987–95.
Svedbom A, Dalen J, Mamolo C, Cappelleri JC, Petersson IF, Stahle M. Treatment patterns with topicals, traditional systemics and biologics in psoriasis—a Swedish database analysis. J Eur Acad Dermatol Venereol. 2015;29(2):215–23.
Fisher MD, Watson C, Fox KM, Chen YW, Gandra SR. Dosing patterns of three tumor necrosis factor blockers among patients with rheumatoid arthritis in a large United States managed care population. Curr Med Res Opin. 2013;29(5):561–8.
Bonafede M, Johnson BH, Fox KM, Watson C, Gandra SR. Treatment patterns with etanercept and adalimumab for psoriatic diseases in a real-world setting. J Dermatolog Treat. 2013;24(5):369–73.
Bonafede M, Fox KM, Watson C, Princic N, Gandra SR. Treatment patterns in the first year after initiating tumor necrosis factor blockers in real-world settings. Adv Ther. 2012;29(8):664–74.
Curkendall S, Patel V, Gleeson M, Campbell RS, Zagari M, Dubois R. Compliance with biologic therapies for rheumatoid arthritis: do patient out-of-pocket payments matter? Arthritis Rheum. 2008;59(10):1519–26.
Yazici Y, Krasnokutsky S, Barnes JP, Hines PL, Wang J, Rosenblatt L. Changing patterns of tumor necrosis factor inhibitor use in 9074 patients with rheumatoid arthritis. J Rheumatol. 2009;36(5):907–13.
Borah BJ, Huang X, Zarotsky V, Globe D. Trends in RA patients’ adherence to subcutaneous anti-TNF therapies and costs. Curr Med Res Opin. 2009;25(6):1365–77.
Vander Cruyssen B, Durez P, Westhovens R, De Keyser F. Seven-year follow-up of infliximab therapy in rheumatoid arthritis patients with severe long-standing refractory disease: attrition rate and evolution of disease activity. Arthritis Res Ther. 2010;12(3):R77.
Glintborg B, Ostergaard M, Krogh NS, et al. Clinical response, drug survival, and predictors thereof among 548 patients with psoriatic arthritis who switched tumor necrosis factor alpha inhibitor therapy: results from the Danish Nationwide DANBIO Registry. Arthritis Rheum. 2013;65(5):1213–23.
Ostergaard M, Unkerskov J, Linde L, et al. Low remission rates but long drug survival in rheumatoid arthritis patients treated with infliximab or etanercept: results from the nationwide Danish DANBIO database. Scand J Rheumatol. 2007;36(2):151–4.
Saougou I, Markatseli TE, Papagoras C, Voulgari PV, Alamanos Y, Drosos AA. Sustained clinical response in psoriatic arthritis patients treated with anti-TNF agents: a 5-year open-label observational cohort study. Semin Arthritis Rheum. 2011;40(5):398–406.
Nell-Duxneuner V, Schroeder Y, Reichardt B, Bucsics A. The use of TNF-inhibitors in ankylosing spondylitis in Austria from 2007 to 2009—a retrospective analysis. Int J Clin Pharmacol Ther. 2012;50(12):867–72.
Greenberg JD, Reed G, Decktor D, et al. A comparative effectiveness study of adalimumab, etanercept and infliximab in biologically naive and switched rheumatoid arthritis patients: results from the US CORRONA registry. Ann Rheum Dis. 2012;71(7):1134–42.
Stockl KM, Shin JS, Lew HC, et al. Outcomes of a rheumatoid arthritis disease therapy management program focusing on medication adherence. J Manag Care Pharm. 2010;16(8):593–604.
Oladapo A, Barner JC, Lawson KA, et al. Medication effectiveness with the use of tumor necrosis factor inhibitors among Texas Medicaid patients diagnosed with rheumatoid arthritis. J Manag Care Spec Pharm. 2014;20(7):657–67.
Tkacz J, Ellis L, Bolge SC, Meyer R, Brady BL, Ruetsch C. Utilization and adherence patterns of subcutaneously administered anti-tumor necrosis factor treatment among rheumatoid arthritis patients. Clin Ther. 2014;36(5):737–47.
Harley CR, Frytak JR, Tandon N. Treatment compliance and dosage administration among rheumatoid arthritis patients receiving infliximab, etanercept, or methotrexate. Am J Manag Care. 2003;9(6 Suppl):S136–43.
Kristensen LE, Saxne T, Nilsson JA, Geborek P. Impact of concomitant DMARD therapy on adherence to treatment with etanercept and infliximab in rheumatoid arthritis. Results from a six-year observational study in southern Sweden. Arthritis Res Ther. 2006;8(6):R174.
Gulfe A, Kristensen LE, Geborek P. Six and 12 weeks treatment response predicts continuation of tumor necrosis factor blockade in rheumatoid arthritis: an observational cohort study from southern Sweden. J Rheumatol. 2009;36(3):517–21.
Matsubara H, Kojima T, Kaneko A, et al. Longterm retention rate and risk factor for discontinuation due to insufficient efficacy and adverse events in Japanese patients with rheumatoid arthritis receiving etanercept therapy. J Rheumatol. 2014;41(8):1583–9.
Zink A, Listing J, Kary S, et al. Treatment continuation in patients receiving biological agents or conventional DMARD therapy. Ann Rheum Dis. 2005;64(9):1274–9.
Flouri I, Markatseli TE, Voulgari PV, et al. Comparative effectiveness and survival of infliximab, adalimumab, and etanercept for rheumatoid arthritis patients in the Hellenic Registry of Biologics: low rates of remission and 5-year drug survival. Semin Arthritis Rheum. 2014;43(4):447–57.
Yang CT, Kuo CF, Luo SF, Yu KH. Discontinuation of anti-TNF-alpha therapy in a Chinese cohort of patients with rheumatoid arthritis. Clin Rheumatol. 2012;31(11):1549–57.
Cho SK, Sung YK, Choi CB, Bae SC. Impact of comorbidities on TNF inhibitor persistence in rheumatoid arthritis patients: an analysis of Korean National Health Insurance claims data. Rheumatol Int. 2012;32(12):3851–6.
Desai A, Zator ZA, de Silva P, et al. Older age is associated with higher rate of discontinuation of anti-TNF therapy in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(2):309–15.
Carmona L, Gomez-Reino JJ. Survival of TNF antagonists in spondylarthritis is better than in rheumatoid arthritis. Data from the Spanish registry BIOBADASER. Arthritis Res Ther. 2006;8(3):R72.
Glintborg B, Ostergaard M, Krogh NS, Dreyer L, Kristensen HL, Hetland ML. Predictors of treatment response and drug continuation in 842 patients with ankylosing spondylitis treated with anti-tumour necrosis factor: results from 8 years’ surveillance in the Danish nationwide DANBIO registry. Ann Rheum Dis. 2010;69(11):2002–8.
Gniadecki R, Kragballe K, Dam TN, Skov L. Comparison of drug survival rates for adalimumab, etanercept and infliximab in patients with psoriasis vulgaris. Br J Dermatol. 2011;164(5):1091–6.
Kristensen LE, Karlsson JA, Englund M, Petersson IF, Saxne T, Geborek P. Presence of peripheral arthritis and male sex predicting continuation of anti-tumor necrosis factor therapy in ankylosing spondylitis: an observational prospective cohort study from the South Swedish Arthritis Treatment Group Register. Arthritis Care Res (Hoboken). 2010;62(10):1362–9.
Pavelka K, Forejtova S, Stolfa J, et al. Anti-TNF therapy of ankylosing spondylitis in clinical practice. Results from the Czech national registry ATTRA. Clin Exp Rheumatol. 2009;27(6):958–63.
Markenson JA, Gibofsky A, Palmer WR, et al. Persistence with anti-tumor necrosis factor therapies in patients with rheumatoid arthritis: observations from the RADIUS registry. J Rheumatol. 2011;38(7):1273–81.
Tynjala P, Vahasalo P, Honkanen V, Lahdenne P. Drug survival of the first and second course of anti-tumour necrosis factor agents in juvenile idiopathic arthritis. Ann Rheum Dis. 2009;68(4):552–7.
Lie E, Kristensen LE, Forsblad-d’Elia H, Zverkova-Sandstrom T, Askling J, Jacobsson LT. The effect of comedication with conventional synthetic disease modifying antirheumatic drugs on TNF inhibitor drug survival in patients with ankylosing spondylitis and undifferentiated spondyloarthritis: results from a nationwide prospective study. Ann Rheum Dis. 2015;74(6):970–8.
Gomez-Reino JJ, Carmona L. Switching TNF antagonists in patients with chronic arthritis: an observational study of 488 patients over a four-year period. Arthritis Res Ther. 2006;8(1):R29.
Oei HB, Hooker RS, Cipher DJ, Reimold A. High rates of stopping or switching biological medications in veterans with rheumatoid arthritis. Clin Exp Rheumatol. 2009;27(6):926–34.
Fagerli KM, Lie E, van der Heijde D, et al. The role of methotrexate co-medication in TNF-inhibitor treatment in patients with psoriatic arthritis: results from 440 patients included in the NOR-DMARD study. Ann Rheum Dis. 2014;73(1):132–7.
Carrascosa JM, Vilavella M, Garcia-Doval I, et al. Body mass index in patients with moderate-to-severe psoriasis in Spain and its impact as an independent risk factor for therapy withdrawal: results of the Biobadaderm Registry. J Eur Acad Dermatol Venereol. 2014;28(7):907–14.
Staples MP, March L, Lassere M, Reid C, Buchbinder R. Health-related quality of life and continuation rate on first-line anti-tumour necrosis factor therapy among rheumatoid arthritis patients from the Australian Rheumatology Association Database. Rheumatology (Oxford). 2011;50(1):166–75.
Billioud V, Laharie D, Filippi J, et al. Adherence to adalimumab therapy in Crohn’s disease: a French multicenter experience. Inflamm Bowel Dis. 2011;17(1):152–9.
Borras-Blasco J, Gracia-Perez A, Castera MD, Rosique-Robles JD, Abad J. Educational session as a tool to increase patient satisfaction of switching etanercept from the prefilled syringe to the autoinjection pen. Expert Opin Biol Ther. 2013;13(8):1103–8.
Zimmer PA, Braun LT, Fraser R, Hecht L, Kelliher F. Promoting success in self-injection: listening to patients. Medsurg Nurs. 2015;24(4):279–82.
Borras-Blasco J, Gracia-Perez A, Rosique-Robles JD, Castera MD, Abad FJ. Acceptability of switching adalimumab from a prefilled syringe to an autoinjection pen. Expert Opin Biol Ther. 2010;10(3):301–7.
Schulze-Koops H, Giacomelli R, Samborski W, et al. Factors influencing the patient evaluation of injection experience with the SmartJect autoinjector in rheumatoid arthritis. Clin Exp Rheumatol. 2015;33(2):201–8.
Liu Y, Caldera F, Skup M, Tundia N, Chao J. Factors influencing self-reported perceptions of adherence, satisfaction, and benefits in patients receiving adalimumab therapy. J Managed Care Spec Pharm. 2015;21(4 Supp A):1–96.
An Y, Liu T, He D, et al. The usage of biological DMARDs and clinical remission of rheumatoid arthritis in China: a real-world large scale study. Clin Rheumatol. 2017;36(1):35–43.
Bluett J, Morgan C, Thurston L, et al. Impact of inadequate adherence on response to subcutaneously administered anti-tumour necrosis factor drugs: results from the Biologics in Rheumatoid Arthritis Genetics and Genomics Study Syndicate cohort. Rheumatology (Oxford). 2015;54(3):494–9.
Carter CT, Waters HC, Smith DB. Impact of infliximab adherence on Crohn’s disease-related healthcare utilization and inpatient costs. Adv Ther. 2011;28(8):671–83.
Kane SV, Chao J, Mulani PM. Adherence to infliximab maintenance therapy and health care utilization and costs by Crohn’s disease patients. Adv Ther. 2009;26(10):936–46.
Stein DJ, Ananthakrishnan AN, Issa M, et al. Impact of prior irregular infliximab dosing on performance of long-term infliximab maintenance therapy in Crohn’s disease. Inflamm Bowel Dis. 2010;16(7):1173–9.
Harnett J, Wiederkehr D, Gerber R, Gruben D, Koenig A, Bourret J. Real-world evaluation of TNF-inhibitor utilization in rheumatoid arthritis. J Med Econ. 2016;19(2):91–102.
Tang B, Rahman M, Waters HC, Callegari P. Treatment persistence with adalimumab, etanercept, or infliximab in combination with methotrexate and the effects on health care costs in patients with rheumatoid arthritis. Clin Ther. 2008;30(7):1375–84.
Degli Esposti L, Favalli EG, Sangiorgi D, et al. Persistence, switch rates, drug consumption and costs of biological treatment of rheumatoid arthritis: an observational study in Italy. ClinicoEcon Outcomes Res. 2017;9:9–17.
Alexis AF, Strober BE. Off-label dermatologic uses of anti-TNF-a therapies. J Cutan Med Surg. 2005;9(6):296–302.
National Institute for Health and Clinical Excellence. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. NICE guideline (CG76). 2009. https://www.nice.org.uk/guidance/cg76. Accessed 3 Aug 2018.
De Keyser F, Hoffman I, Durez P, Kaiser MJ, Westhovens R. Longterm followup of rituximab therapy in patients with rheumatoid arthritis: results from the Belgian MabThera in Rheumatoid Arthritis registry. J Rheumatol. 2014;41(9):1761–5.
Hetland ML, Lindegaard HM, Hansen A, et al. Do changes in prescription practice in patients with rheumatoid arthritis treated with biological agents affect treatment response and adherence to therapy? Results from the nationwide Danish DANBIO Registry. Ann Rheum Dis. 2008;67(7):1023–6.
Brocq O, Roux CH, Albert C, et al. TNFalpha antagonist continuation rates in 442 patients with inflammatory joint disease. Joint Bone Spine. 2007;74(2):148–54.
Duclos M, Gossec L, Ruyssen-Witrand A, et al. Retention rates of tumor necrosis factor blockers in daily practice in 770 rheumatic patients. J Rheumatol. 2006;33(12):2433–8.
Markatseli TE, Alamanos Y, Saougou I, Voulgari PV, Drosos AA. Survival of TNF-alpha antagonists in rheumatoid arthritis: a long-term study. Clin Exp Rheumatol. 2012;30(1):31–8.
Iannone F, Salaffi F, Marchesoni A, et al. Five-year survival on infliximab in rheumatoid arthritis patients: analysis from an Italian registry (GISEA) by different calendar years. Clin Exp Rheumatol. 2015;33(4):524–30.
Iannone F, Gremese E, Atzeni F, et al. Longterm retention of tumor necrosis factor-alpha inhibitor therapy in a large italian cohort of patients with rheumatoid arthritis from the GISEA registry: an appraisal of predictors. J Rheumatol. 2012;39(6):1179–84.
Santoleri F, Sorice P, Lasala R, Rizzo RC, Costantini A. Medication adherence and persistence in the treatment of rheumatoid arthritis with adalimumab and etanercept. Six years of analysis. J Med Econ. 2014;17(5):320–5.
Hirabara S, Takahashi N, Fukaya N, et al. Clinical efficacy of abatacept, tocilizumab, and etanercept in Japanese rheumatoid arthritis patients with inadequate response to anti-TNF monoclonal antibodies. Clin Rheumatol. 2014;33(9):1247–54.
Hishitani Y, Ogata A, Shima Y, et al. Retention of tocilizumab and anti-tumour necrosis factor drugs in the treatment of rheumatoid arthritis. Scand J Rheumatol. 2013;42(4):253–9.
Li P, Blum MA, Von Feldt J, Hennessy S, Doshi JA. Adherence, discontinuation, and switching of biologic therapies in medicaid enrollees with rheumatoid arthritis. Value Health. 2010;13(6):805–12.
Kane S, Dixon L. Adherence rates with infliximab therapy in Crohn’s disease. Aliment Pharmacol Ther. 2006;24(7):1099–103.
Calip GS, Adimadhyam S, Xing S, Rincon JC, Lee WJ, Anguiano RH. Medication adherence and persistence over time with self-administered TNF-alpha inhibitors among young adult, middle-aged, and older patients with rheumatologic conditions. Semin Arthritis Rheum 2017;47(2):157–64.
An Y, Liu T, He D, et al. The usage of biological DMARDs and clinical remission of rheumatoid arthritis in China: a real-world large scale study. Clin Rheumatol. 2017;36(1):35–43.
Courvoisier DS, Alpizar-Rodriguez D, Gottenberg JE, et al. Rheumatoid arthritis patients after initiation of a new biologic agent: trajectories of disease activity in a Large Multinational Cohort Study. EBioMedicine. 2016;11:302–6.
Foster SA, Zhu B, Guo J, et al. Patient characteristics, health care resource utilization, and costs associated with treatment-regimen failure with biologics in the treatment of psoriasis. J Manag Care Spec Pharm. 2016;22(4):396–405.
Inzinger M, Wippel-Slupetzky K, Weger W, et al. Survival and effectiveness of tumour necrosis factor-alpha inhibitors in the treatment of plaque psoriasis under daily life conditions: report from the Psoriasis Registry Austria. Acta Derm Venereol. 2016;96(2):207–12.
Lequerre T, Farran E, Menard JF, et al. Switching from an anti-TNF monoclonal antibody to soluble TNF-receptor yields better results than vice versa: An observational retrospective study of 72 rheumatoid arthritis switchers. Joint Bone Spine. 2015;82(5):330–7.
Sauer BC, Teng C-C, He T, et al. Effectiveness and costs of biologics in veterans with rheumatoid arthritis. Am J Pharm. 2015;7(6):280–9.
Svedbom A, Dalén J, Black CM, Kachroo S. Persistence and costs with subcutaneous TnF-alpha inhibitors in immune-mediated rheumatic disease stratified by treatment line. Patient Prefer Adherence. 2017;11:95.
Acknowledgements
Funding
UCB Pharma sponsored the review and development of the manuscript and funded all article processing charges. UCB Pharma reviewed the text to ensure that from a UCB Pharma perspective, the data presented in the publication are scientifically, technically and medically supportable, that they do not contain any information that has the potential to damage the intellectual property of UCB Pharma and that the publication complies with applicable laws, regulations, guidelines and good industry practice. The authors approved the final version to be published after critically revising the manuscript/publication for important intellectual content.
Medical Writing and Editorial Assistance
The authors thank ICON plc. for conducting the literature review and Jonas Nilsson, from ICON plc., for reviewing the final report. The authors also acknowledge Debbie Nixon, DPhil, from UCB Pharma, UK, for publication coordination and Bethan Du-Mont, BSc, and Simon Foulcer, PhD, from Costello Medical, UK, for medical writing and editorial assistance in preparing this manuscript for publication, based on the authors’ input and direction. Funding for this was provided by UCB Pharma.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Disclosures
Nikos Maniadakis received consultancy fees from UCB Pharma. Emese Toth is an employee of UCB Pharma. Michael Schiff serves as a consultant for UCB Pharma and has received grant/research support from UCB Pharma. Xuan Wang is an employee of ICON plc. and received study funding from UCB. Maria Nassim is an employee of ICON plc. and received study funding from UCB. Boglarka Szegvari is an employee of UCB Pharma. Irina Moutian is an employee of UCB Pharma. Jeffrey R. Curtis has received grant/research support and consultancy fees from Roche, Genentech, UCB Pharma, Janssen, Corrona, Amgen, Pfizer, Bristol-Myers Squibb, Myriad, Radius, Eli Lilly and AbbVie.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.6850133.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Maniadakis, N., Toth, E., Schiff, M. et al. A Targeted Literature Review Examining Biologic Therapy Compliance and Persistence in Chronic Inflammatory Diseases to Identify the Associated Unmet Needs, Driving Factors, and Consequences. Adv Ther 35, 1333–1355 (2018). https://doi.org/10.1007/s12325-018-0759-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-018-0759-0