Abstract
Spinocerebellar ataxia type 11 (SCA11) is a rare type of autosomal dominant cerebellar ataxia, mainly characterized by progressive cerebellar ataxia, abnormal eye signs and dysarthria. SCA11 is caused by variants in TTBK2, which encodes tau tubulin kinase 2 (TTBK2) protein. Only a few families with SCA11 were described to date, all harbouring small deletions or insertions that result in frameshifts and truncated TTBK2 proteins. In addition, TTBK2 missense variants were also reported but they were either benign or still needed functional validation to ascertain their pathogenic potential in SCA11. The mechanisms behind cerebellar neurodegeneration mediated by TTBK2 pathogenic alleles are not clearly established. There is only one neuropathological report and a few functional studies in cell or animal models published to date. Moreover, it is still unclear whether the disease is caused by TTBK2 haploinsufficiency of by a dominant negative effect of TTBK2 truncated forms on the normal allele. Some studies point to a lack of kinase activity and mislocalization of mutated TTBK2, while others reported a disruption of normal TTBK2 function caused by SCA11 alleles, particularly during ciliogenesis. Although TTBK2 has a proven function in cilia formation, the phenotype caused by heterozygous TTBK2 truncating variants are not clearly typical of ciliopathies. Thus, other cellular mechanisms may explain the phenotype seen in SCA11. Neurotoxicity caused by impaired TTBK2 kinase activity against known neuronal targets, such as tau, TDP-43, neurotransmitter receptors or transporters, may contribute to neurodegeneration in SCA11.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hereditary cerebellar ataxias
Hereditary cerebellar ataxias (HCAs) comprise a heterogeneous group of neurodegenerative disorders characterized by incoordination of movement, often associated with speech and eye movement disturbances. Symptoms are mainly caused by degeneration of cerebellar Purkinje neurons and spinocerebellar tracts. Additional neurological and non-neurological signs can also be present in patients [1, 2]. Currently, no effective pharmacological treatments are available for use in patients with HCAs, except for some episodic ataxias. The main problem in finding effective therapies is HCAs heterogeneity, which leads to a need for specific therapeutics focused on genotypes/disease mechanisms [2, 3]. Genetically, HCAs are very complex and can present with all modes of inheritance (mainly autosomal dominant and autosomal recessive, and a few forms of X-linked and mitochondrial inherited ataxias) [4, 5].
X-linked cerebellar ataxias (XLCAs) are a variable group of disorders mainly characterized by cerebellar dysgenesis (hypoplasia, atrophy, or dysplasia). XLCAs are caused by genomic imbalances or gene variants on the X chromosome, where more than 20 genes have been associated with cerebellar defects. These disorders are quite rare, except for fragile X syndrome, which is caused by CGG triplet expansions in the 5´UTR of FMR1 [6].
Mitochondrial ataxias are clinically and genetically complex and can be caused by variants in mitochondrial DNA (mtDNA) or in nuclear genes that regulate mitochondrial function. Within the group of ataxias caused by mtDNA variants, there are multisystem disorders caused by point variants, namely myoclonic epilepsy and ragged red fibers (MERRF) and encephalomyopathy, lactic acidosis and stroke-like episodes (MELAS), or by large scale rearrangements, as in Kearns-Sayre syndrome (KSS) [7].
Autosomal recessive cerebellar ataxias (ARCAs) are a heterogeneous group of disorders caused by a multitude of genes [8]. Among more than 50 ARCAs, there are two forms caused by intronic repeat expansions that are relatively frequent: Friedreich’s ataxia caused by GAA repeat expansions in FXN [8] and cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS) caused by a pentanucleotide repeat expansion in RFC1 [9]. Other relatively common ARCAs, such as ataxia-telangiectasia (AT) and ataxia with oculomotor apraxia (AOA), and also rare forms are caused by conventional mutations [8]. Congenital ataxias and ataxias associated with metabolic disorders also have an autosomal recessive inheritance pattern [10].
Autosomal dominant cerebellar ataxias, also termed spinocerebellar ataxias (SCAs), are also a heterogeneous group of disorders with an intricate genotype–phenotype spectrum. Currently, these group include 50 SCA types, dentatorubral-pallidoluysian atrophy (DRPLA) and eight episodic ataxias (EA1-EA8). SCAs were numbered from SCA1 to SCA50 in the chronological order in which the disease locus was identified. However, only 44 loci are recognized since SCA9 and SCA33 are unassigned, SCA15, 16 and 29 were linked to the same locus, SCA19 and 22 were also connected to the same locus and SCA24 was proven to be recessively inherited (now referred as SCAR4), and considering NPTX1 as the causal gene for SCA50 [11,12,13]. Moreover, there are five SCAs with known loci but with unknown causal genes (SCA4, 20, 30, 32, 39) [4, 14]. The genetic background of SCAs revealed different underlying mutational mechanisms: (1) coding repeat expansions of CAG triplets cause polyglutamine (polyQ) diseases (SCA1-3, 6, 7, 17 and DRLPA); (2) noncoding triplet, quintuplet or hexaplet repeat expansions (SCA10, 12, 31, 36 and 37) primarily cause disease at the RNA level; (3) other triplet coding repeat expansion can also generate a polyQ protein (SCA8, where a CTG expansion is transcribed in both directions); (4) conventional variants or rearrangements, such as missense variants (e.g., SCA13), frameshift variants (e.g., SCA11), deletions (e.g., SCA15) and duplications (e.g., SCA20), cause different SCAs forms [11, 14, 15]. One SCA-associated gene can be associated with more than one of these mechanisms, as is the case for FGF14. Missense and frameshift variants in FGF14 have previously been reported to cause SCA27 but, very recently, an intronic GAA repeat expansion was found to interfere with FGF14 transcription causing ATX-FGF14 [16, 17]. The polyQ ataxias are the most common SCAs. In most population-based analysis, SCA3/Machado-Joseph Disease is the most frequent subtype, but the relative frequency varies in different populations due to founder effects [18, 19].
Several cellular and molecular processes underlying HCAs pathogenesis have been identified, including transcriptional dysregulation, protein aggregation, autophagy impairment, alterations of calcium homeostasis and mitochondrial defects [8, 20]. However, the reason why all these mechanisms lead to cerebellar neurodegeneration remains largely elusive. Nevertheless, the identification of common pathogenic pathways between the different HCAs forms would be crucial for understanding the basis of cerebellar neurodegeneration [21, 22].
A more detailed description of HCAs clinical features, genetics and pathogenesis can found in Matilla-Dueñas et al. [4] and Klockgether et al. [15].
Spinocerebellar ataxia type 11 (SCA11)
Spinocerebellar ataxia type 11 (SCA11) is a rare form of HCA with an autosomal dominant inheritance pattern. SCA11 prevalence is unknown, but it should account for less than 1% of SCAs in Europe [23]. SCA11 has been characterized as a slowly progressive cerebellar ataxia, with limb and gait imbalance, dysarthria, and oculomotor abnormalities. An overview of the main clinical findings in SCA11 cases is shown in Table 1. All affected individuals showed mild to severe cerebellar atrophy in both hemispheres and the vermis when examined by magnetic resonance imaging (MRI) [23,24,25,26]. Positron emission tomography (PET) scan showed reduced metabolic activity in the cerebellum and pons in the Danish case [26]. In addition to cerebellar ataxia, SCA11 cases mostly presented dysarthria and ocular disturbance signs [23,24,25,26]. Pyramidal signs, such as hyperreflexia, were also observed in some patients [24,25,26]. The age of onset in SCA11 usually range from early to late adulthood, with an average of about 30 years (range from 4–64 years). The life span is thought to be normal, but most patients require walking aid (e.g., wheelchair) later in life [23, 26].
SCA11-associated variants
So far, only a few families have been identified with SCA11. SCA11 was first described in a large British family as a slowly progressive pure cerebellar ataxia, genetically linked to the locus 15q14–21 [25]. Later, the TTBK2 gene located at chromosome 15q15.2, which encodes tau tubulin kinase 2 (TTBK2) protein, was identified as the causal gene for SCA11 [24]. In this study, two heterozygous variants were identified in SCA11 patients: a one-base insertion in TTBK2 (c.1329insA, p.Arg444Thrfs*7) in the British family and a deletion of a dinucleotide in TTBK2 (c.1284_1285delAG, p.Glu429Aspfs*21) in another family of Pakistani ancestry [24]. Interestingly, in a 2013 next-generation sequencing (NGS) study, the variant present in the British family was identified in a patient with cerebellar atrophy, suggesting a possible link between them [27]. Three additional families with TTBK2 truncating variants have been reported: one from France and another from Germany bearing the same variant (c.1306_1307delGA, p.Asp436Tyrfs*14) [23], and one from Denmark (c.1205_1207delinsA, p.Thr402Lysfs*48) [26]. Later, a different truncating variant (c.1302dupC, p.Arg435Glnfs*16) was identified by NGS in a patient of European origin with ataxia and spasticity signs [28]. A detailed description of the SCA11 cases along with the identified TTBK2 pathogenic variants can be found in Table 1.
More recently, some heterozygous missense variants in TTBK2 (Table 2) have been reported in patients presenting with cerebellar ataxia [28,29,30,31,32,33,34,35,36]. However, as far as we understand, none of them were clearly evaluated as pathogenic (pathogenicity predictions and conservations scores of these TTBK2 missense variants are shown in Table S1). Indeed, two of these variants were reported as being normal rare variants [31], while several other variants were classified as variants of unknown significance [28, 33, 36]. Moreover, in any of these reports, functional studies were performed to prove the detrimental effect of the missense variants.
Tau tubulin kinase 2 (TTBK2) protein
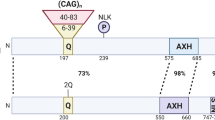
TTBK2 is a serine-threonine protein kinase that belongs to the casein kinase (CK1) group of eukaryotic protein kinases [37]. The other TTBK family member is TTBK1, which is encoded by a different gene (TTBK1) and is neuron specific. The N-terminal kinase domains of TTBK1 and TTBK2 (Fig. 1) have 88% identity and 96% similarity. The rest of their sequence has only 35% identity and 63% similarity, but there is a small C-terminal domain with 43% identity and 58% similarity [38]. Both TTBK1 and TTBK2 have at least two serine any amino acid isoleucine proline (SxIP) motifs at their C-terminal region (Fig. 1b), which are recognized by end binding proteins (EB) proteins [39, 40]. Although TTBK1 and TTBK2 are conserved among vertebrates, only the catalytic domain is preserved in invertebrates, suggesting that TTBK1 and TTBK2 diversified from a common shorter TTBK gene during evolution [38].
TTBK2 genomic location and protein domains. (a) TTBK2 gene is located at chromosome 15q15.2 and has 14 coding exons (exon 1 is non-coding). b TTBK1 (amino acids 34–297) and TTBK2 (amino acids 21–284) have highly similar N-terminal kinase domains (88% identity and 96% similarity). At the C-terminal end, both TTBK1 and TTBK2 have serine-rich polypeptide regions containing SxIP (serine-any amino acid-isoleucine-proline) motifs. TTBK1 also has a central polyglutamate (polyE) region
TTBK2 can encode multiple protein isoforms by alternative splicing; the longest has 1244 amino acids and an expected molecular weight of 137 kDa. TTBK2 protein is ubiquitously expressed in human adult and fetal tissues [24]. In particular, it is highly expressed and exhibit high kinase activity in brain and testis [41]. Within the brain, TTBK2 is expressed in all regions, with high expression in the Purkinje and granular cell layers of the cerebellum, the hippocampus, the midbrain, and the substantia nigra. On other hand, low expression levels were detected in the brain cortex [24].
TTBK2 was first identified based on its ability to phosphorylate the microtubule-associated proteins tau and β-tubulin in vitro [42, 43]. Since then, several cellular functions have been attributed to TTBK2, but few have been described in detail. TTBK2 potential functions include: (1) ciliogenesis [44]; (2) regulation of microtubule dynamics [40]; (3) modulation of membrane transporters and receptors [45,46,47]; (4) phosphorylation of the transactive response DNA-binding protein 43 kDa (TDP-43) [48]; (5) mitosis [49, 50]; (6) cancer progression [51]; (7) and maintenance of the connectivity and viability of Purkinje cells [52]. A summarised description of TTBK2 targets in these cellular processes can be found in Fig. 2.
TTBK2 targets and associated cellular processes. (a) TDP-43, a DNA/RNA binding protein, continuously shuttles between the nucleus and cytoplasm. TTBK2 phosphorylates TDP-43, which can lead to TDP-43 recruitment into cytoplasmic inclusions. (b) Through an unknown mechanism, TTBK2 is able to increase BGT1 abundance at the plasma membrane, enhancing GABA-induced inward current. (c) Conversely, TTBK2 seems to stimulate Gluk2 internalization through Rab5-dependent endocytosis, decreasing Gluk2 protein abundance at the plasma membrane and the glutamate-induced currents. (d) TTBK2 is critical for ciliogenesis initiation from the basal body, namely by phosphorylating and/or recruiting several essential proteins in the process (e.g., CEP164, CEP83, DVL2/3, IFT88) and by promoting CP110 removal from the mother centrioles. Also, MPP9 phosphorylation by TTBK2 promotes its own proteasomal degradation and further removal of the CP110-CEP97 complex, promoting ciliogenesis. (e) TTBK2 participates in microtubules dynamics regulation by phosphorylating β-tubulin, tau and KIF2A. TTBK2 also binds to EB1/3 that allows KIF2A phosphorylation, which in turn inhibits KIF2A/microtubules interaction and decreases KIF2A microtubule depolymerizing activity. (f) TTBK2 phosphorylates SV2A within cluster 2, thus promoting SV2A binding SYT1, which is essential for SYT1 retrieval during synaptic vesicle endocytosis
TTBK2 role in microtubules dynamics
Microtubules are dynamic structures composed of α/β tubulin heterodimers tightly controlled to ensure the normal function and division of eukaryotic cells. In addition to the phosphorylation of β-tubulin and tau protein [42, 43], TTBK2 also acts as a plus-end tracking protein (+ TIP) by tracking growing microtubules ends in a kinase-independent manner [39]. TTBK2 binds to the end binding proteins 1/3 (EB1/3), which enables the phosphorylation of kinesin family member 2A (KIF2A) (Fig. 2e) at Ser135 in vitro, inhibiting KIF2A interaction with the microtubules and decreasing KIF2A microtubule depolymerizing activity [40]. In the absence of TTBK2, KIF2A exhibit an extensive localization to the microtubules, which induces short-lived microtubules with an increased shrink rate and a decreased rescue frequency. On the other hand, overexpression of TTBK2 displaces EB1 from the microtubules, suggesting that it may regulate the association of + TIPs and other microtubule-associated proteins with newly polymerized ends. Therefore, the EB–TTBK2 interaction appears to antagonize the microtubule-depolymerizing machinery, primarily affecting KIF2A [40].
One study also suggested that centrosomal protein of 164 kDa (CEP164) may play a role in recruiting TTBK2 to the midbody during cytokinesis [53]. Although, neither this theory was confirmed nor the role of TTBK2 at the midbody [50, 53]. Another study reported the TTBK homolog in D. melanogaster (Asator) to be localized in the cytoplasm during interphase but redistributed to the mitotic spindle during mitosis, where it interacts with the spindle matrix protein Megator (homolog of the human translocated promotor region protein) that take part in the spindle assembly checkpoint. Thus, it was proposed that Asator kinase activity may regulate spindle function and microtubule dynamics [49].
TTBK2 function in ciliogenesis
TTBK2 plays a pivotal role in the initiation of ciliogenesis from the basal body (Fig. 2d). TTBK2 is localized at the distal end of the mother centriole, where it is responsible for the removal of the centriolar coiled coil protein 110 (CP110; negative regulator) and recruitment of the intraflagellar transport 88, 140 and 81 proteins (IFT88, IFT140 and IFT81; positive regulators and cargo carriers in the cilium) [44, 54, 55]. It has also been suggested that TTBK2 regulates a final step in cilia initiation by recruiting Inturned (INTU; core subunit of the ciliogenesis and planar polarity effector complex) to the mother centriole, which in turn recruits the small guanosine triphosphatase RSG1 (positive regulator) [56]. Indeed, TTBK2 localization at the mother centriole is a critical step in ciliogenesis initiation, being mediated by CEP164 [55, 57].
In addition to the basal body, TTBK2 is also found at the transition zone of the cilium, where it could regulate the maintenance of ciliogenesis [44, 54]. Indeed, Bowie et al. reported that TTBK2 also plays a role in controlling cilia length, stability, and trafficking [54]. They showed that TTBK2 hypomorphic mutant cells present decreased cilia length and frequency of cilia formation, and disrupted trafficking of the Sonic Hedgehog (SHH) downstream effector Smoothened (SMO) and regulator KIF7 (controls cilium structure) [54].
Furthermore, ciliogenesis significantly depends on TTBK2 kinase activity [44]. TTBK2 phosphorylates several proteins required for ciliogenesis initiation, such as CEP164, CEP83, CEP89, Rabin8, coiled-coil domain containing 92 (CCDC92) and dishevelled 2/3 (DVL2/3), in their intrinsically disordered regions (IDRs) [58]. Although the effect of TTBK2-dependent phosphorylation on these proteins was not determined, it was hypothesized that it may regulate protein interactions and complexes necessary for primary cilium formation [58]. In accordance with this, Oda et al. have shown that CEP164 and/or DVL3 phosphorylation by TTBK2 inhibited CEP164-DVL3 interaction [57]. Moreover, Lo et al. reported that CEP83 phosphorylation by TTBK2 controls membrane vesicle docking, which promotes CP110 removal from the mother centrioles and further ciliogenesis initiation [59]. Other interesting effect of TTBK2-dependent phosphorylation may be targeting ciliary proteins for degradation [60]. Phosphorylation of M-Phase Phosphoprotein 9 (MPP9) by TTBK2 at the beginning of ciliogenesis promotes proteasomal degradation of MPP9 (a negative regulator of ciliogenesis). This facilitates the removal of MPP9 and the CP110-CEP97 complex (negative regulator) from the distal end of the mother centriole, promoting the initiation of ciliogenesis [60].
Therefore, TTBK2 appears to play a major role in controlling cilia initiation, maintenance, stability, and trafficking through phosphorylation and/or protein interactions.
TTBK2 role in neuronal processes
One of the main targets of TTBK2 is the cytoskeletal tau protein [43]; abnormal tau hyperphosphorylation is associated with neurofibrillary tangles (NFTs) formation and neurodegeneration in Alzheimer’s Disease [61]. Interestingly, the two TTBK2-dependent phosphorylation sites in tau (Ser208 and Ser210) have been reported as elevated phosphorylation sites in Alzheimer’s disease brain [62, 63]. Moreover, tau phosphorylation at Ser208 increased tau affinity towards microtubules and contributed to tau aggregation, being a unique marker of aggregation and mature NFTs compared to other phosphorylation sites [63]. Intracellular aggregates of hyperphosphorylated tau are also a hallmark of frontotemporal lobar degeneration associated with tau inclusions (FTLD-tau). Elevated levels of TTBK2 and increased immunoreactivity of TTBK2 in the frontal cortex and hippocampus were observed in post-mortem tissues from FTLD-tau patients [64]. Evidence of tau-related neurodegeneration promoted by TTBK2 was observed in C. elegans models. One study reported that knocking down the TTBK2 C. elegans homolog (TTBK) in the presence of a mutant tau transgene (linked to FTLD and parkinsonism linked to chromosome 17) enhanced worms uncoordinated movement phenotype [65]. A second study showed that co-expression of human TTBK2 in a human tau background in C. elegans reduced worms lifespan, exacerbated behavioural defects and cause a significant loss of GABAergic motor neurons and axonal abnormalities [64]. Moreover, high levels of TTBK2 were lethal in combination with high levels of tau in worms. In the same study, other potential TTBK2-dependent phosphorylation sites in tau were identified (Thr181, Ser202, Thr231, and Ser396/404) [64].
TTBK2 has also been found to phosphorylate TDP-43, a DNA/RNA binding protein, at Ser409/410 in vitro and in vivo [48]. Loss of functional TDP-43 in the nucleus and accumulation of hyperphosphorylated and ubiquitinated TDP-43 in cytoplasmic inclusions are hallmarks of amyotrophic lateral sclerosis (ALS) and FTLD associated with TDP-43 inclusions (FTLD-TDP). TDP-43 positive inclusions have been also detected in patients with other neurological disorders [66]. Overexpression of TTBK1 and TTBK2 in cells can induce TDP-43 phosphorylation and recruitment into cytoplasmic inclusions (Fig. 2a), similar to the neuropathology seen in neurological disorders [48]. Moreover, TTBK2 immunostaining is increased in FTLD-TDP frontal cortex compared to controls, and TTBK2 co-localize with TDP-43 positive inclusions in FTLD-TDP frontal cortex and ALS spinal cord [48, 64].
Other neuronal targets of TTBK2 include the synaptic vesicle protein 2A (SV2A) [67], the betain/GABA transporter 1 (BGT1) [45] and the glutamate (kainate) receptor subunit 2 (GluK2) [47].
Both TTBK1 and TTBK2 can phosphorylate SV2A at two clusters of sites in the N-terminal cytoplasmic region but TTBK2 is more effective in phosphorylating the Thr84 residue within cluster 2 (Fig. 2f). This event is critical in promoting SV2A binding to the Ca2+ binding domain C2B of synaptogamin-1 (SYT1), a Ca2+ sensor that triggers neurotransmitter release. The interaction between SV2A and SYT1 is essential for the specific retrieval of synaptotagmin-1 during synaptic vesicle endocytosis [67].
TTBK2 seems to have opposite effects on BGT1 and GluK2 activities in Xenopus oocytes models. Co-expression of TTBK2 with BGT1 enhanced GABA induced currents [45] while co-expression with GluK2 decreased glutamate-induced currents [47]. Upregulation of BGT1 and downregulation of GluK2 by TTBK2 is mediated, at least in part, by respectively increasing or decreasing BGT1 and GluK2 protein abundances at the cell membrane (Fig. 2b and c) [45, 47]. Moreover, it is possible that TTBK2 stimulates Gluk2 internalization through small G-protein (GTPase) Rab5-dependent endocytosis, ultimately mediating neuroexcitotoxicity protection [47].
Therefore, it is possible that TTBK2 contributes to synapse homeostasis/stability through modulation of synaptic vesicles transport, and neuronal receptors and transporters localization and activity.
SCA11 pathogenesis
Despite all the functions attributed to TTBK2, the mechanisms underlying cerebellar neurodegeneration in SCA11 are still not clearly stablished. Moreover, there is only one neuropathological report on SCA11. Post-mortem neuropathological examination of the brain of one affected individual from the British family (c.1329insA) revealed gross atrophy of the cerebellum accompanied by severe loss of Purkinje cells and granule cells, mild gliosis of the cerebellar white matter, and neuronal loss in the dentate nucleus [24, 68, 69]. The brainstem was well preserved, while the medulla revealed severe neuronal loss, and the cerebral hemispheres revealed atrophy consistent with the patient’s age (77 years old) [68, 69]. There were other alterations related with aging, such as, neurofibrillary tangles and β-amyloid-positive plaques within the hippocampus, neocortex, and transentorhinal, entorhinal and insular cortex. Neuronal intranuclear or cytoplasmic inclusions positive for p62 or ubiquitin were not detected [24, 68]. This neuropathological report is unique amongst SCA11 cases.
Functional studies showing the impact of TTBK2 variants are scarce and include two with non-concordant results [24, 41]. Lymphoblasts from SCA11 patients (c.1329insA; c.1284_1285delAG) presented mRNA levels reduced by approximately 50%, when compared to unaffected individuals, suggesting that mutated mRNA is prematurely degraded by nonsense-mediated decay (NMD), causing TTBK2 haploinsufficiency. Still, it seems that a proportion of the abnormal mRNA escapes NMD [24]. Contrarily, at the protein level, overexpression studies showed that the same TTBK2 truncating mutants were expressed at higher levels compared to wild-type TTBK2. Moreover, TTBK2 mutants partially promoted the relocalization of TTBK2 from the cytosol to the nucleus and suppressed its kinase activity [41]. Additional studies showed that a truncated TTBK2 form (at residue 450) is kinase inactive, not being able to regulate the activities of a membrane receptor and a transporter in Xenopus models [45, 47].
Interestingly, homozygous mutant mice for the TTBK2 truncating variant c.1329insA were embryonic lethal after embryonic day 10. Embryos at day 10 showed major abnormalities, such as developmental delay, indistinct brain subdivisions and distorted caudal bodies. On the other hand, heterozygous mutant mice for the same variant were viable and fertile, with no apparent abnormalities, and a regular lifespan [41]. Moreover, analysis of TTBK2 kinase activity showed a 40–50% reduction in the brain of heterozygous mutant mice and nearly a 90% reduction in mouse embryonic fibroblasts (MEFs) from homozygous mutant mice [41].
Additionally, some studies have suggested that SCA11 truncating variants cause abnormalities in ciliogenesis [44, 54, 55], which is possibly the most well studied function of TTBK2 (described above). Primary cilia are microtubule-based extensions of the plasma membrane that are linked to hereditary developmental syndromes termed ciliopathies [70]. Primary cilia formation is triggered at the distal end of the mother centriole (basal body) during the quiescent state (G0 phase) [71]. In MEFs derived from mice bearing a TTBK2 null mutation, ciliogenesis is blocked because TTBK2 is required for ciliogenesis initiation by removing the negative regulator CP110 from the mother centriole and by recruiting IFT proteins [44]. In the same way, heterozygous and homozygous embryos mice for a SCA11 truncated variant (c.1329insA) lacked cilia in most tissues [54]. Rescue experiments showed that while wild-type TTBK2 overexpression promoted cilia formation in TTBK2 null MEFs, the same did not occur in homozygous mutant mice, in which the frequency of cilia rescue was significantly lower. Moreover, SCA11 truncated proteins (c.1329insA; c.1284_1285delAG) lacked activity and seemed to interfere with the function of wild-type TTBK2 in ciliogenesis, pointing to a dominant negative effect of TTBK2 truncated forms [44, 54]. Nevertheless, these truncated proteins were stable and partially retained a normal centrosomal localization [44]. Another study reported that CEP164 is responsible for recruiting TTBK2 to centrioles, thus promoting ciliogenesis. However, the SCA11-truncated protein (c.1329InsA) was unable to bind to CEP164, which might explain the partial localization defects of TTBK2 truncated proteins in cells [55].
In overall, these functional studies point to both a loss of function and a dominant negative effect of TTBK2 truncating variants but mostly focus on the role of TTBK2 during ciliogenesis.
Conclusions
SCA11 is a rare form of HCA caused by heterozygous small deletions or insertions in TTBK2 (Table 1), generating truncated proteins with intact N-terminal kinase domains. Nevertheless, loss of the C-terminal region may abolish other functional domains, yet uncharacterized, and/or lead to conformational changes that impact TTBK2 stability, interactions, and functions. Thus, SCA11 has been linked to both haploinsufficiency [24] and a dominant negative mechanism where mutated TTBK2 interferes with the normal allele functions [44]. Additionally, TTBK2 missense variants were reported in patients with cerebellar ataxia but, in our understanding, additional studies are needed to validate their pathogenicity (Table 2 and S1). Validation of new variant types may uncover new disease mechanisms behind SCA11 and expand the number of SCA11 cases. The most well studied mechanism disrupted by TTBK2 truncating variants is perhaps ciliogenesis [44, 54, 55], where TTBK2 plays a pivotal role, particularly in cilia formation. Pathogenic variants in ciliary proteins can result in early embryonic lethality or severe diseases termed ciliopathies [72]. Most of these disorders are inherited in an autosomal recessive manner with symptoms start during childhood or adolescence but some are more genetically complex, presenting digenic inheritance, modifiers genes or gene-dosage effects [72]. Since SCA11 and ciliopathies genetic inheritance and phenotypes seem to differ quite substantially, it is possible that other disease mechanisms underlie SCA11 in addition to ciliary defects [50]. The role of TTBK2 as + TIP and regulator of tubulin, tau or KIF2A through phosphorylation [40, 42, 43] also points to a disturbance in microtubule-based and axonal transport in SCA11. Subsequently, TTBK2 may play a role in synaptic vesicles transport and neurotransmitter release [67], and also in controlling the transport process and activity of neuronal receptors and transporters [45, 47]. Although, additional studies are needed to explore these functions and their implications in SCA11.
Data availability
Not applicable.
References
Harding AE. Classification of the Hereditary Ataxias and Paraplegias. Lancet. 1983;321:1151–5.
Marsden JF. Cerebellar ataxia. Handb Clin Neurol. Elsevier B.V.; 2018. p. 261–81.
Jones TM, Shaw JD, Sullivan K, Zesiewicz TA. Treatment of cerebellar ataxia. Neurodegener Dis Manag. 2014;4:379–92.
Matilla-Dueñas A, Corral-Juan M, Rodríguez-Palmero Seuma A, Vilas D, Ispierto L, Morais S, et al. Rare Neurodegenerative Diseases: Clinical and Genetic Update. Adv Exp Med Biol. 2017;1031:443–96.
Hersheson J, Haworth A, Houlden H. The inherited ataxias: Genetic heterogeneity, mutation databases, and future directions in research and clinical diagnostics. Hum Mutat. 2012;33:1324–32.
Zanni G, Bertini E. X-linked ataxias. Handb Clin Neurol. Elsevier B.V.; 2018. p. 175–189.
Vernon HJ, Bindoff LA. Mitochondrial ataxias. Handb Clin Neurol. Elsevier B.V.; 2018. p. 129–41.
Fogel BL. Autosomal-recessive cerebellar ataxias. Handb Clin Neurol. Elsevier B.V.; 2018. p. 187–209.
Cortese A, Simone R, Sullivan R, Vandrovcova J, Tariq H, Yan YW, et al. Biallelic expansion of an intronic repeat in RFC1 is a common cause of late-onset ataxia. Nat Genet. Springer US; 2019;51:649–58.
Palau F, Espinós C. Autosomal recessive cerebellar ataxias. Orphanet J Rare Dis. 2006;1:47.
Witek N, Hawkins J, Hall D. Genetic ataxias: update on classification and diagnostic approaches. Curr Neurol Neurosci Rep. Current Neurology and Neuroscience Reports; 2021;21:13.
Corral-Juan M, Casquero P, Giraldo-Restrepo N, Laurie S, Martinez-Piñeiro A, Mateo-Montero RC, et al. New spinocerebellar ataxia subtype caused by SAMD9L mutation triggering mitochondrial dysregulation (SCA49). Brain Commun. 2022;4.
Coutelier M, Jacoupy M, Janer A, Renaud F, Auger N, Saripella GV, et al. NPTX1 mutations trigger endoplasmic reticulum stress and cause autosomal dominant cerebellar ataxia. Brain. 2022;145:1519–34.
Mundwiler A, Shakkottai VG. Autosomal-dominant cerebellar ataxias. 1st ed. Handb. Clin. Neurol. Elsevier B.V.; 2018.
Klockgether T, Mariotti C, Paulson HL. Spinocerebellar ataxia. Nat Rev Dis Prim. 2019;5:1–21.
Rafehi H, Read J, Szmulewicz DJ, Davies KC, Snell P, Fearnley LG, et al. An intronic GAA repeat expansion in FGF14 causes the autosomal-dominant adult-onset ataxia SCA50/ATX-FGF14. Am J Hum Genet. 2023;110:105–19.
Pellerin D, Danzi MC, Wilke C, Renaud M, Fazal S, Dicaire M-J, et al. Deep Intronic FGF14 GAA Repeat Expansion in Late-Onset Cerebellar Ataxia. N Engl J Med. 2023;388:128–41.
Ruano L, Melo C, Silva MC, Coutinho P. The Global Epidemiology of Hereditary Ataxia and Spastic Paraplegia: A Systematic Review of Prevalence Studies. Neuroepidemiology. 2014;42:174–83.
Coutinho P, Ruano L, Loureiro JL, Cruz VT, Barros J, Tuna A, et al. Hereditary ataxia and spastic paraplegia in Portugal: A population-based prevalence study. JAMA Neurol. 2013;70:746–55.
Matilla-Dueñas A, Ashizawa T, Brice A, Magri S, McFarland KN, Pandolfo M, et al. Consensus paper: pathological mechanisms underlying neurodegeneration in spinocerebellar ataxias. Cerebellum. 2014;13:269–302.
Eidhof I, Van De Warrenburg BP, Schenck A. Integrative network and brain expression analysis reveals mechanistic modules in ataxia. J Med Genet. 2019;56:283–92.
Robinson KJ, Watchon M, Laird AS. Aberrant Cerebellar Circuitry in the Spinocerebellar Ataxias. Front Neurosci. 2020;14:1–27.
Bauer P, Stevanin G, Beetz C, Synofzik M, Schmitz-Hübsch T, Wüllner U, et al. Spinocerebellar ataxia type 11 (SCA11) is an uncommon cause of dominant ataxia among French and German kindreds. J Neurol Neurosurg Psychiatry. 2010;81:1229–32.
Houlden H, Johnson J, Gardner-Thorpe C, Lashley T, Hernandez D, Worth P, et al. Mutations in TTBK2, encoding a kinase implicated in tau phosphorylation, segregate with spinocerebellar ataxia type 11. Nat Genet. 2007;39:1434–6.
Worth PF, Giunti P, Gardner-Thorpe C, Dixon PH, Davis MB, Wood NW. Autosomal dominant cerebellar ataxia type III: Linkage in a large british family to a 7.6-cM region on chromosome 15.q14–21.3. Am J Hum Genet. 1999;65:420–6.
Lindquist SG, Møller LB, Dali CI, Marner L, Kamsteeg EJ, Nielsen JE, et al. A Novel TTBK2 De Novo Mutation in a Danish Family with Early-Onset Spinocerebellar Ataxia. Cerebellum. 2017;16:268–71.
Németh AH, Kwasniewska AC, Lise S, Parolin Schnekenberg R, Becker EBE, Bera KD, et al. Next generation sequencing for molecular diagnosis of neurological disorders using ataxias as a model. Brain. 2013;136:3106–18.
Coutelier M, Hammer MB, Stevanin G, Monin ML, Davoine CS, Mochel F, et al. Efficacy of exome-targeted capture sequencing to detect mutations in known cerebellar ataxia genes. JAMA Neurol. 2018;75:591–9.
Deng Y, Fu J, Zhong YQ, Zhang M, Qi X. First finding of familial spinal cerebellar Ataxia11 in China: clinical, imaging and genetic features. Neurol Sci. 2020;41:155–60.
Galatolo D, De Michele G, Silvestri G, Leuzzi V, Casali C, Musumeci O, et al. NGS in Hereditary Ataxia: When Rare Becomes Frequent. Int J Mol Sci. 2021;22:8490.
Edener U, Kurth I, Meiner A, Hoffmann F, Hübner CA, Bernard V, et al. Missense exchanges in the TTBK2 gene mutated in SCA11. J Neurol. 2009;256:1856–9.
Jiao Q, Sun H, Zhang H, Wang R, Li S, Sun D, et al. The combination of whole-exome sequencing and copy number variation sequencing enables the diagnosis of rare neurological disorders. Clin Genet. 2019;96:140–50.
Iqbal Z, Rydning SL, Wedding IM, Koht J, Pihlstrøm L, Rengmark AH, et al. Targeted high throughput sequencing in hereditary ataxia and spastic paraplegia. Brusgaard K, editor. PLoS One. 2017;12:e0174667.
Fakhro KA, Robay A, Rodrigues-Flores JL, Mezey JG, Al-Shakaki AA, Chidiac O, et al. Point of Care Exome Sequencing Reveals Allelic and Phenotypic Heterogeneity Underlying Mendelian disease in Qatar. Hum Mol Genet. 2019;28:3970–81.
Choi K-D, Kim J-S, Kim H-J, Jung I, Jeong S-H, Lee S-H, et al. Genetic Variants Associated with Episodic Ataxia in Korea. Sci Rep. 2017;7:13855.
Coutelier M, Coarelli G, Monin M-L, Konop J, Davoine C-S, Tesson C, et al. A panel study on patients with dominant cerebellar ataxia highlights the frequency of channelopathies. Brain. 2017;140:1579–94.
Manning G, Whyte DB, Martinez R, Hunter T, Sudarsanam S. The protein kinase complement of the human genome. Science (80- ). 2002;298:1912–34.
Ikezu S, Ikezu T. Tau-tubulin kinase. Front Mol Neurosci. 2014;7.
Jiang K, Toedt G, Montenegro Gouveia S, Davey NE, Hua S, van der Vaart B, et al. A Proteome-wide Screen for Mammalian SxIP Motif-Containing Microtubule Plus-End Tracking Proteins. Curr Biol. 2012;22:1800–7.
Watanabe T, Kakeno M, Matsui T, Sugiyama I, Arimura N, Matsuzawa K, et al. TTBK2 with EB1/3 regulates microtubule dynamics in migrating cells through KIF2A phosphorylation. J Cell Biol. 2015;210:737–51.
Bouskila M, Esoof N, Gay L, Fang EH, Deak M, Begley MJ, et al. TTBK2 kinase substrate specificity and the impact of spinocerebellar- ataxia-causing mutations on expression, activity, localization and development. Biochem J. 2011;437:157–67.
Takahashi M, Tomizawa K, Ishiguro K, Takamatsu M, Fujita SC, Imahori K. Involvement of τ Protein Kinase I in Paired Helical Filament-Like Phosphorylation of the Juvenile τ in Rat Brain. J Neurochem. 1995;64:1759–68.
Tomizawa K, Omori A, Ohtake A, Sato K, Takahashi M. Tau-tubulin kinase phosphorylates tau at Ser-208 and Ser-210, sites found in paired helical filament-tau. FEBS Lett. 2001;492:221–7.
Goetz SC, Liem KF, Anderson KV. The spinocerebellar ataxia-associated gene tau tubulin kinase 2 controls the initiation of ciliogenesis. Cell. 2012;151:847–58.
Almilaji A, Munoz C, Hosseinzadeh Z, Lang F. Upregulation of Na, Cl - -coupled betaine/γ-amino-butyric acid transporter BGT1 by tau tubulin kinase 2. Cell Physiol Biochem. 2013;32:334–43.
Alesutan I, Sopjani M, Dërmaku-Sopjani M, Munoz C, Voelkl J, Lang F. Upregulation of Na + -coupled Glucose transporter SGLT1 by Tau Tubulin Kinase 2. Cell Physiol Biochem. 2012;30:458–65.
Nieding K, Matschke V, Meuth SG, Lang F, Seebohm G, Strutz-Seebohm N. Tau Tubulin Kinase TTBK2 Sensitivity of Glutamate Receptor GluK2. Cell Physiol Biochem. 2016;39:1444–52.
Liachko NF, McMillan PJ, Strovas TJ, Loomis E, Greenup L, Murrell JR, et al. The Tau Tubulin Kinases TTBK1/2 Promote Accumulation of Pathological TDP-43. PLoS Genet. 2014;10.
Qi H, Yao C, Cai W, Girton J, Johansen KM, Johansen J. Asator, a tau-tubulin kinase homolog in Drosophila localizes to the mitotic spindle. Dev Dyn. 2009;238:3248–56.
Liao J-C, Yang TT, Weng RR, Kuo C-T, Chang C-W. TTBK2: A Tau Protein Kinase beyond Tau Phosphorylation. Biomed Res Int. 2015;2015:1–10.
Bender C, Ullrich A. PRKX, TTBK2 and RSK4 expression causes sunitinib resistance in kidney carcinoma- and melanoma-cell lines. Int J Cancer. 2012;131:E45-55.
Bowie E, Goetz SC. Ttbk2 and primary cilia are essential for the connectivity and survival of cerebellar purkinje neurons. Elife. 2020;9.
Chaki M. Exome capture reveals ZNF423 and CEP164 mutations, linking renal ciliopathies to DNA damage response signaling. Cell. 2012;150:533–48.
Bowie E, Norris R, Anderson K V., Goetz SC. Spinocerebellar ataxia type 11-associated alleles of Ttbk2 dominantly interfere with ciliogenesis and cilium stability. PLoS Genet. 2018;14.
Čajánek L, Nigg EA. Cep164 triggers ciliogenesis by recruiting Tau tubulin kinase 2 to the mother centriole. Proc Natl Acad Sci U S A. 2014;111:E2841–50.
Agbu SO, Liang Y, Liu A, Anderson KV. The small GTPase RSG1 controls a final step in primary cilia initiation. J Cell Biol. 2018;217:413–27.
Oda T, Chiba S, Nagai T, Mizuno K. Binding to Cep164, but not EB1, is essential for centriolar localization of TTBK2 and its function in ciliogenesis. Genes Cells. 2014;19:927–40.
Bernatik O, Pejskova P, Vyslouzil D, Hanakova K, Zdrahal Z, Cajanek L. Phosphorylation of multiple proteins involved in ciliogenesis by Tau Tubulin kinase 2. Zheng Y, editor. Mol Biol Cell. 2020;31:1032–46.
Lo C-H, Lin I-H, Yang TT, Huang Y-C, Tanos BE, Chou P-C, et al. Phosphorylation of CEP83 by TTBK2 is necessary for cilia initiation. J Cell Biol. 2019;218:3489–505.
Huang N, Zhang D, Li F, Chai P, Wang S, Teng J, et al. M-Phase Phosphoprotein 9 regulates ciliogenesis by modulating CP110-CEP97 complex localization at the mother centriole. Nat Commun. 2018;9:4511.
Hanger DP, Anderton BH, Noble W. Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol Med. 2009;15:112–9.
Hanger DP, Noble W. Functional Implications of Glycogen Synthase Kinase-3-Mediated Tau Phosphorylation. Int J Alzheimers Dis. 2011;2011:1–11.
Xia Y, Prokop S, Gorion K-MM, Kim JD, Sorrentino ZA, Bell BM, et al. Tau Ser208 phosphorylation promotes aggregation and reveals neuropathologic diversity in Alzheimer’s disease and other tauopathies. Acta Neuropathol Commun. 2020;8:88.
Taylor LM, McMillan PJ, Liachko NF, Strovas TJ, Ghetti B, Bird TD, et al. Pathological phosphorylation of tau and TDP-43 by TTBK1 and TTBK2 drives neurodegeneration. Mol Neurodegener. 2018;13:7.
Kraemer BC, Burgess JK, Chen JH, Thomas JH, Schellenberg GD. Molecular pathways that influence human tau-induced pathology in Caenorhabditis elegans. Hum Mol Genet. 2006;15:1483–96.
Prasad A, Bharathi V, Sivalingam V, Girdhar A, Patel BK. Molecular mechanisms of TDP-43 misfolding and pathology in amyotrophic lateral sclerosis. Front Mol Neurosci. 2019;12:45.
Zhang N, Gordon SL, Fritsch MJ, Esoof N, Campbell DG, Gourlay R, et al. Phosphorylation of Synaptic Vesicle Protein 2A at Thr84 by Casein Kinase 1 Family Kinases Controls the Specific Retrieval of Synaptotagmin-1. J Neurosci. 2015;35:2492–507.
Giunti P, Houlden H, Gardner-Thorpe C, Worth PF, Johnson J, Hilton DA, et al. Spinocerebellar ataxia type 11. Handb Clin Neurol. Elsevier B.V.; 2012. p. 521–34.
Johnson J, Wood N, Giunti P, Houlden H. Clinical and genetic analysis of spinocerebellar ataxia type 11. Cerebellum. 2008;7:159–64.
Reiter JF, Leroux MR. Genes and molecular pathways underpinning ciliopathies. Nat Rev Mol Cell Biol. 2017;18:533–47.
Goetz SC, Anderson KV. The primary cilium: A signalling centre during vertebrate development. Nat Rev Genet. 2010;11:331–44.
Braun DA, Hildebrandt F. Ciliopathies Cold Spring Harb Perspect Biol. 2017;9: a028191.
Funding
Open access funding provided by FCT|FCCN (b-on). This study was developed while under the support from Ataxia UK (Small grant—ZGRACA). MS acknowledges funding from FCT- Fundação para a Ciência e a Tecnologia through program DL 57/2016—Norma Transitória. DS is the recipient of a fellowship (UI/BD/154402/2023) funded by FCT.
Author information
Authors and Affiliations
Contributions
MS conceived the study. DF performed the literature search. DF and MS wrote the manuscript draft and critically revised and edited the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12311_2023_1540_MOESM1_ESM.xlsx
Supplementary file1 Table S1 Pathogenicity and conservation predictions of the TTBK2 missense variants reported in patients with inherited cerebellar ataxia.CADD, REVEL and DANN scores are considered as deleterious above 20, 0.5, and 0.5, respectively. In nucleotide conservation scores, the larger the score, the more conserved the site. GERP++ RS, PhastCons (17, 30 and 100way), PhyloP100way, Phylo30way,and Phylo17way range from -12,3 to 6,17; 0 to 1; -20 to 10,003; -20 to 1,312; and -13,362 to 0,756, respectively.MAF, minor allele frequency in Gnomad v2.1.1. NA, not available. Nº software, the number of software predicting a deleterious effect amongst all the prediction software for the variants. * PP4 criteria was attributed in all cases considering that all patients’ phenotypes are specific for SCA11; PP3 criteria was attributed to missense variants with Nº software > 7 (from 14 in total); BP4 criteria was attributed to missense variants with Nº software ≤ 7 (from 14 in total); PM1 criteria was considered for variants affecting TTBK2 kinase domain. ** The variant was considered of uncertain significance but borderline likely pathogenic. (XLSX 15 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Felício, D., Santos, M. Spinocerebellar ataxia type 11 (SCA11): TTBK2 variants, functions and associated disease mechanisms. Cerebellum 23, 678–687 (2024). https://doi.org/10.1007/s12311-023-01540-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-023-01540-6