Abstract
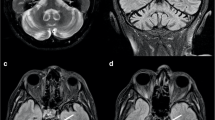
Evaluation of ataxia in children is challenging in clinical practice. This is particularly true for highly heterogeneous conditions such as primary mitochondrial disorders (PMD). This study aims to explore cerebellar and brain abnormalities identified on MRI as potential predictors of ataxia in patients with PMD and, likewise, to determine the effect of the patient’s genetic profile on these predictors as well as determination of the temporal relationship of clinical ataxia with MRI findings. We evaluated clinical, radiological, and genetic characteristics of 111 PMD patients younger than 21 years of age at The Children’s Hospital of Philadelphia. Data was extracted from charts. Blinded radiological evaluations were carried out by experienced neuroradiologists. Multivariate logistic regression and generalized equation estimates were used for analysis. Ataxia was identified in 41% of patients. Cerebellar atrophy or putaminal involvement with mitochondrial DNA (mtDNA) mutations (OR 1.18, 95% CI 1.1–1.3, p < 0.001) and nuclear DNA mutation with no atrophy of the cerebellum (OR 1.14, 95% CI 1.0–1.3, p = 0.007) predicted an increased likelihood of having ataxia per year of age. Central tegmental tract predicted the presence of ataxia independent of age and pathogenic variant origin (OR 9.8, 95% CI 2–74, p = 0.009). Ataxia tended to precede the imaging finding of cerebellar atrophy. Cerebellar atrophy and putaminal involvement on MRI of pediatric-onset PMD may predict the presence of ataxia with age in patients with mtDNA mutations. This study provides predicted probabilities of having ataxia per year of age that may help in family counseling and future research of the population.




Similar content being viewed by others
Change history
26 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12311-022-01370-y
References
Sanger TD, Chen D, Delgado MR, Gaebler-Spira D, Hallett M, Mink JW, et al. Definition and classification of negative motor signs in childhood. Pediatrics. 2006;118(5):2159–67.
Brandsma R, Lawerman TF, Kuiper MJ, Lunsing RJ, Burger H, Sival DA. Reliability and discriminant validity of ataxia rating scales in early onset ataxia. Dev Med Child Neurol. 2017;59(4):427–32.
Lawerman TF, Brandsma R, Burger H, Burgerhof JGM, Sival DA, the Childhood Ataxia and Cerebellar Group of the European Pediatric Neurology Society. Age-related reference values for the pediatric Scale for Assessment and Rating of Ataxia: a multicentre study. Dev Med Child Neurol. 2017;59(10):1077–82.
Musselman KE, Stoyanov CT, Marasigan R, Jenkins ME, Konczak J, Morton SM, et al. Prevalence of ataxia in children: a systematic review. Neurology. 2014;82(1):80–9.
Lynch DR, McCormick A, Schadt K, Kichula E. Pediatric ataxia: focus on chronic disorders. Semin Pediatr Neurol. 2018;5(25):54–64.
Vernon HJ, Bindoff LA. Mitochondrial ataxias. Handb Clin Neurol. 2018;155:129–41.
Hernandez-Castillo CR, Vaca-Palomares I, Barrios F, Martinez L, Boll MC, Fernandez-Ruiz J. Ataxia Severity Correlates with White Matter Degeneration in Spinocerebellar Ataxia Type 7. AJNR Am J Neuroradiol. 2016;37(11):2050–4.
Salman MS, Lee EJ, Tjahjadi A, Chodirker BN. The epidemiology of intermittent and chronic ataxia in children in Manitoba. Canada Dev Med Child Neurol. 2013;55(4):341–7.
Bargiela D, Shanmugarajah P, Lo C, Blakely EL, Taylor RW, Horvath R, et al. Mitochondrial pathology in progressive cerebellar ataxia. Cerebellum Ataxias. 2015;4(2):16.
Claeys KG, Abicht A, Häusler M, Kleinle S, Wiesmann M, Schulz JB, et al. Novel genetic and neuropathological insights in neurogenic muscle weakness, ataxia, and retinitis pigmentosa (NARP). Muscle Nerve. 2016;54(2):328–33.
Mattiazzi M, Vijayvergiya C, Gajewski CD, DeVivo DC, Lenaz G, Wiedmann M, et al. The mtDNA T8993G (NARP) mutation results in an impairment of oxidative phosphorylation that can be improved by antioxidants. Hum Mol Genet. 2004;13(8):869–79.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885.
C Alves, SR Teixeira, JS Martin-Saavedra, FG Goncalves, F Lo Russo, C Muraresku, et al. 2020 Pediatric leigh syndrome: neuroimaging features and genetic correlations. Ann Neurol
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Brandsma R, Spits AH, Kuiper MJ, Lunsing RJ, Burger H, Kremer HP, et al. Ataxia rating scales are age-dependent in healthy children. Dev Med Child Neurol. 2014;56(6):556–63.
Adinolfi S, Trifuoggi M, Politou AS, Martin S, Pastore A. A structural approach to understanding the iron-binding properties of phylogenetically different frataxins. Hum Mol Genet. 2002;11(16):1865–77.
Campuzano V, Montermini L, Lutz Y, Cova L, Hindelang C, Jiralerspong S, et al. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum Mol Genet. 1997;6(11):1771–80.
Pandolfo M. Neurologic outcomes in Friedreich ataxia. Neurology Genetics. 2020;6(3):e415.
Rummey C, Farmer JM, Lynch DR. Predictors of loss of ambulation in Friedreich’s ataxia. EClinicalMedicine. 2020;18:100213.
Galea CA, Huq A, Lockhart PJ, Tai G, Corben LA, Yiu EM, et al. Compound heterozygous FXN mutations and clinical outcome in friedreich ataxia. Ann Neurol. 2016;79(3):485–95.
Ng YS, Martikainen MH, Gorman GS, Blain A, Bugiardini E, Bunting A, et al. Pathogenic variants in MT-ATP6: A United Kingdom-based mitochondrial disease cohort study. Ann Neurol. 2019;86(2):310–5.
Leshinsky-Silver E, Shuvalov R, Inbar S, Cohen S, Lev D, Lerman-Sagie T. Juvenile Leigh syndrome, optic atrophy, ataxia, dystonia, and epilepsy due to T14487C mutation in the mtDNA-ND6 gene: a mitochondrial syndrome presenting from birth to adolescence. J Child Neurol. 2011;26(4):476–81.
Incecik F, Herguner OM, Besen S, Bozdoğan ST, Mungan NO. Late-Onset Leigh Syndrome due to NDUFV1 Mutation in a 10-Year-Old Boy Initially Presenting with Ataxia. J Pediatr Neurosci. 2018;13(2):205–7.
Thorburn DR, Rahman J, Rahman S, et al. Mitochondrial DNA-Associated Leigh Syndrome and NARP. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Mefford HC, et al., editors. GeneReviews(®). Seattle: University of Washington; 1993.
Berardo A, Emmanuele V, Vargas W, Tanji K, Naini A, Hirano M. Leber hereditary optic neuropathy plus dystonia, and transverse myelitis due to double mutations in MT-ND4 and MT-ND6. J Neurol. 2020;267(3):823–9.
Murai M, Enokido Y, Inamura N, Yoshino M, Nakatsu Y, van der Horst GT, et al. Early postnatal ataxia and abnormal cerebellar development in mice lacking Xeroderma pigmentosum Group A and Cockayne syndrome Group B DNA repair genes. Proc Natl Acad Sci USA. 2001;98(23):13379–84.
Edvardson S, Elbaz-Alon Y, Jalas C, Matlock A, Patel K, Labbé K, et al. A mutation in the THG1L gene in a family with cerebellar ataxia and developmental delay. Neurogenetics. 2016;17(4):219–25.
Heimer G, Gregory A, Hogarth P, Hayflick S, Ben Zeev B, et al. MECR-Related Neurologic Disorder. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, et al., editors. GeneReviews®. Seattle: University of Washington; 1993.
Head RA, Brown RM, Zolkipli Z, Shahdadpuri R, King MD, Clayton PT, et al. Clinical and genetic spectrum of pyruvate dehydrogenase deficiency: dihydrolipoamide acetyltransferase (E2) deficiency. Ann Neurol. 2005;58(2):234–41.
Pyle A, Ramesh V, Bartsakoulia M, Boczonadi V, Gomez-Duran A, Herczegfalvi A, et al. Behr’s Syndrome is typically associated with disturbed mitochondrial translation and mutations in the C12orf65 gene. J Neuromuscul Dis. 2014;1(1):55–63.
Tulli S, Del Bondio A, Baderna V, Mazza D, Codazzi F, Pierson TM, et al. Pathogenic variants in the AFG3L2 proteolytic domain cause SCA28 through haploinsufficiency and proteostatic stress-driven OMA1 activation. J Med Genet. 2019;56(8):499–511.
Bénit P, Chretien D, Kadhom N, de Lonlay-Debeney P, Cormier-Daire V, Cabral A, et al. Large-scale deletion and point mutations of the nuclear NDUFV1 and NDUFS1 genes in mitochondrial complex I deficiency. Am J Hum Genet. 2001;68(6):1344–52.
DiMauro S, Hirano M, et al. MERRF. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, et al., editors. GeneReviews®. Seattle: University of Washington; 1993.
Liu JC, Liu J, Holmström KM, Menazza S, Parks RJ, Fergusson MM, et al. MICU1 serves as a molecular gatekeeper to prevent in vivo mitochondrial calcium overload. Cell Rep. 2016;16(6):1561–73.
Tetreault M, Fahiminiya S, Antonicka H, Mitchell GA, Geraghty MT, Lines M, et al. Whole-exome sequencing identifies novel ECHS1 mutations in Leigh syndrome. Hum Genet. 2015;134(9):981–91.
Schara U, von Kleist-Retzow JC, Lainka E, Gerner P, Pyle A, Smith PM, et al. Acute liver failure with subsequent cirrhosis as the primary manifestation of TRMU mutations. J Inherit Metab Dis. 2011;34(1):197–201.
Meng F, Cang X, Peng Y, Li R, Zhang Z, Li F, et al. Biochemical evidence for a nuclear modifier allele (A10S) in TRMU (Methylaminomethyl-2-thiouridylate-methyltransferase) related to mitochondrial tRNA modification in the phenotypic manifestation of deafness-associated 12S rRNA mutation. J Biol Chem. 2017;292(7):2881–92.
El-Hattab AW, Li FY, Schmitt E, Zhang S, Craigen WJ, Wong LJ. MPV17-associated hepatocerebral mitochondrial DNA depletion syndrome: new patients and novel mutations. Mol Genet Metab. 2010;99(3):300–8.
Dines JN, Golden-Grant K, LaCroix A, Muir AM, Cintron DL, McWalter K, et al. TANGO2: expanding the clinical phenotype and spectrum of pathogenic variants. Genet Med. 2019;21(3):601–7.
Penque BA, Su L, Wang J, Ji W, Bale A, Luh F, et al. A homozygous variant in RRM2B is associated with severe metabolic acidosis and early neonatal death. Eur J Med Genet. 2019;62(11):103574.
Rezende TJR, Martinez ARM, Faber I, Girotto Takazaki KA, Martins MP, de Lima FD, et al. Developmental and neurodegenerative damage in Friedreich’s ataxia. Eur J Neurol. 2019;26(3):483–9.
Selvadurai LP, Harding IH, Corben LA, Stagnitti MR, Storey E, Egan GF, et al. Cerebral and cerebellar grey matter atrophy in Friedreich ataxia: the IMAGE-FRDA study. J Neurol. 2016;263(11):2215–23.
Mercadillo RE, Galvez V, Díaz R, Hernández-Castillo CR, Campos-Romo A, Boll M-C, et al. Parahippocampal gray matter alterations in Spinocerebellar Ataxia Type 2 identified by voxel based morphometry. J Neurol Sci. 2014;347(1–2):50–8.
Niyazov DM, Kahler SG, Frye RE. Primary mitochondrial disease and secondary mitochondrial dysfunction: importance of distinction for diagnosis and treatment. Mol Syndromol. 2016;7(3):122–37.
Işık U, Dinçer A. Central tegmentum tract hyperintensities in pediatric neurological patients: incidence or coincidence. Brain Dev. 2017;39(5):411–7.
Aguilera-Albesa S, Poretti A, Honnef D, Aktas M, Yoldi-Petri ME, Huisman TAGM, et al. T2 hyperintense signal of the central tegmental tracts in children: disease or normal maturational process? Neuroradiology. 2012;54(8):863–71.
Funding
Financial relationships during the last 12 months: JSMS was employed at CHOP until June 2020 and has been employed by St. Christopher’s Hospital for Children since July 2020. SRT, CAPFA, FGG, LOTG, CM, AG, and AV were employed and continue to be employed by CHOP. AV has received book authorship royalties from Oxford University Press, consultant fees from Syneos Health, and support via the CHOP mitochondrial medicine program from Cyclerion and Minovia, none related to this manuscript. CM and AG are part of The CHOP Mitochondrial Medicine Frontier Program. MK works as consultant for the Radiology Department at CHOP and has been employed by the Centre for Statistical Consultation (M.K.), University of Stellenbosch, South Africa.
Author information
Authors and Affiliations
Contributions
(1) Research project: A. Conception, B. Organization, C. Execution; (2) Statistical analysis: A. Design, B. Execution, C. Review and critique; (3) Manuscript preparation: A. Writing of the first draft, B. Review and critique.
JSSM: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B
SRT: 1A, 1B, 1C, 2A, 2C, 3B
CAPFA: 1A, 1B, 1C, 2A, 2C, 3B
FGG: 1A, 1B, 1C, 2A, 2C, 3B
LOTG: 1A, 1B, 1C, 2A, 2C, 3B
MK: 1A, 1B, 1C, 2A, 2B, 2C, 3B
CM: 1A, 1B, 1C, 2A, 2C, 3B
AG: 1A, 1B, 1C, 2A, 2C, 3B
AV: 1A, 1B, 1C, 2A, 2B, 2C, 3B
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martin-Saavedra, J.S., Teixeira, S.R., Alves, C.A.P.F. et al. Genetic and Clinical Predictors of Ataxia in Pediatric Primary Mitochondrial Disorders. Cerebellum 21, 116–131 (2022). https://doi.org/10.1007/s12311-021-01276-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-021-01276-1