Abstract
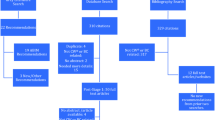
The 2022 revision of the Japanese Breast Cancer Society (JBCS) Clinical Practice Guidelines for surgical treatment of breast cancer was updated following a systematic review of the literature using the Medical Information Network Distribution Service (MINDS) procedure, which focuses on the balance of benefits and harms for various clinical questions (CQs). Experts in surgery designated by the JBCS addressed five areas: breast surgery, axillary surgery, breast reconstruction, surgical treatment for recurrent and metastatic breast cancer, and other related topics. The revision of the guidelines encompassed 4 CQs, 7 background questions (BQs), and 14 future research questions (FRQs). A significant revision in the 2022 edition pertained to axillary management after neoadjuvant chemotherapy in CQ2. The primary aim of the 2022 JBCS Clinical Practice Guidelines is to provide evidence-based recommendations to empower patients and healthcare professionals in making informed decisions regarding surgical treatment for breast cancer.
Similar content being viewed by others
Data availability
The raw data required to reproduce the above findings are available to download from https://jbcs.xsrv.jp/guideline/2022/g_index/.
References
Inokuchi M, Kutomi G, Kijima Y, et al. The Japanese Breast Cancer Society clinical practice guidelines for surgical treatment of breast cancer. Breast Cancer. 2020;27:4–8.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ—the LORD study. Eur J Cancer. 2015;51:1497–510.
Francis A, Thomas J, Fallowfield L, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer. 2015;51:2296–303.
Kanbayashi C, Iwata H. Current approach and future perspective for ductal carcinoma in situ of the breast. Jpn J Clin Oncol. 2017;47:671–7.
Hwang ES, Hyslop T, Lynch T, et al. The COMET (comparison of operative versus monitoring and endocrine therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9:e026797.
Galimberti V, Cole BF, Viale G, et al. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23–01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol. 2018;19:1385–93.
Solá M, Alberro JA, Fraile M, et al. Complete axillary lymph node dissection versus clinical follow-up in breast cancer patients with sentinel node micrometastasis: final results from the multicenter clinical trial AATRM 048/13/2000. Ann Surg Oncol. 2013;20:120–7.
Giuliano AE, Ballman KV, McCall L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318:918–26.
Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981–22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–10.
Sávolt Á, Péley G, Polgár C, et al. Eight-year follow up result of the OTOASOR trial: the optimal treatment of the axilla-surgery or radiotherapy after positive sentinel lymph node biopsy in early-stage breast cancer: a randomized, single centre, phase III, non-inferiority trial. Eur J Surg Oncol. 2017;43:672–9.
Geng C, Chen X, Pan X, Li J. The feasibility and accuracy of sentinel lymph node biopsy in initially clinically node-negative breast cancer after neoadjuvant chemotherapy: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0162605.
Boughey JC, Suman VJ, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455–61.
Kuehn T, Bauerfeind I, Fehm T, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14:609–18.
Caudle AS, Yang WT, Krishnamurthy S, et al. Improved axillary evaluation following neoadjuvant therapy for patients with node-positive breast cancer using selective evaluation of clipped nodes: implementation of targeted axillary dissection. J Clin Oncol. 2016;34:1072–8.
Eriksen C, Frisell J, Wickman M, et al. Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat. 2011;127:439–46.
Park SH, Han W, Yoo TK, et al. Oncologic safety of immediate breast reconstruction for invasive breast cancer patients: a matched case control study. J Breast Cancer. 2016;19:68–75.
Ryu JM, Paik HJ, Park S, et al. Oncologic outcomes after immediate breast reconstruction following total mastectomy in patients with breast cancer: a matched case-control study. J Breast Cancer. 2017;20:74–81.
Ryu JM, Park S, Paik HJ, et al. Oncologic safety of immediate breast reconstruction in breast cancer patients who underwent neoadjuvant chemotherapy: short-term outcomes of a matched case-control study. Clin Breast Cancer. 2017;17:204–10.
Baek SH, Bae SJ, Yoon CI, et al. Immediate breast reconstruction does not have a clinically significant impact on adjuvant treatment delay and subsequent survival outcomes. J Breast Cancer. 2019;22:109–19.
Bjöhle J, Onjukka E, Rintelä N, et al. Post-mastectomy radiation therapy with or without implant-based reconstruction is safe in terms of clinical target volume coverage and survival—a matched cohort study. Radiother Oncol. 2019;131:229–36.
Vieira R, Ribeiro LM, Carrara GFA, et al. Effectiveness and safety of implant-based breast reconstruction in locally advanced breast carcinoma: a matched case-control study. Breast Care (Basel). 2019;14:200–10.
Wu ZY, Kim HJ, Lee JW, et al. Long-term oncologic outcomes of immediate breast reconstruction vs conventional mastectomy alone for breast cancer in the setting of neoadjuvant chemotherapy. JAMA Surg. 2020;155:1142–50.
Soran A, Ozbas S, Kelsey SF, Gulluoglu BM. Randomized trial comparing locoregional resection of primary tumor with no surgery in stage IV breast cancer at the presentation (Protocol MF07-01): a study of Turkish Federation of the National Societies for Breast Diseases. Breast J. 2009;15:399–403.
Shien T, Nakamura K, Shibata T, et al. A randomized controlled trial comparing primary tumour resection plus systemic therapy with systemic therapy alone in metastatic breast cancer (PRIM-BC): Japan Clinical Oncology Group Study JCOG1017. Jpn J Clin Oncol. 2012;42:970–3.
Badwe R, Hawaldar R, Nair N, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol. 2015;16:1380–8.
Fitzal F, Bjelic-Radisic V, Knauer M, et al. Impact of breast surgery in primary metastasized breast cancer: outcomes of the prospective randomized phase III ABCSG-28 POSYTIVE trial. Ann Surg. 2019;269:1163–9.
Khan SA, Zhao F, Goldstein LJ, et al. Early local therapy for the primary site in de novo stage IV breast cancer: results of a randomized clinical trial (EA2108). J Clin Oncol. 2022;40:978–87.
Reinhorn D, Mutai R, Yerushalmi R, et al. Locoregional therapy in de novo metastatic breast cancer: systemic review and meta-analysis. Breast. 2021;58:173–81.
Acknowledgements
The authors are grateful to Ms. Natsue Uehiro, Ms. Mai Ohnishi, Ms. Yuri Ozaki, Mr. Hiroaki Shima, Ms. Eriko Takahashi, Ms. Mifue Taminato, Mr. Takahiro Tsukioki, Ms. Ai Tsuchiya, Ms. Aya Noro and Ms. Michi Morita for their important help with the systematic review. The authors would also like to thank Ms. Fujimi Kawai and Ms. Natsuki Narita of the Japanese Medical Library Society; Prof. Masahiro Yoshida of the International University of Health and Welfare; and Hitomi Sasaki and Kazuyo Uno at Kanehara Publishing Co., Ltd. for their generous assistance and advice.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T Sakai received honoraria from Astra Zeneca, Chugai, Kyowa-Kirin, Pfizer, Daiichi-Sankyo, Exact Science, Canon, and Ethicon. GK received honoraria from Lilly, Kyowa Kirin, Daiichi Sankyo, AstraZeneca Pfizer, and Chugai. T Shien received honoraria from Daiichi-Sankyo, Pfizer, Chugai, and Lilly. SA received honoraria from Astra Zeneca, Chugai, Daiichi Sankyo, Eli Lilly, and Pfizer. TA received honoraria from Pfizer, Chugai, Eli Lilly, Astra Zeneca and Kyowa Kirin. MI received honoraria from Astra Zeneca, Chugai, Pfizer, Taiho, Novartis and Nihon Kayaku. SK received honoraria from Pfizer, Daiichi-Sankyo, Chugai, Astra Zeneca and Kyowa Kirin. MS received honoraria from Chugai, Kyowa Kirin, Pfizer, Astra Zeneca and Eli Lilly. Kaori Terata received honoraria and payment for expert testimony from Astra Zeneka, Daiichi-Sankyo, Chugai, Pfizer, Eli Lilly and Taiho. Koichi Tomita received honoraria from Ethicon. CY does not have any Disclosure. YY received research funding and honoraria from Chugai, Kyowa-Kirin, Eisai, Daiichi-Sankyo, Nippon-Kayaku, Taiho, Takeda, Lilly, Pfizer, Novartis and Takeda, MSD, Sysmex and Exact Science. YU, and he also a member of the Board of Directors in Japanese Breast Cancer Society and Japan Breast Cancer Research Group. HI received Grants and consultant fees from Chugai, Daiichi Sankyo, Astra Zeneca, Lilly, MSD, Pfizer and Gilead and honoraria from Daiichi-Sankyo, Chugai, Astra, Lilly, MSD, Pfizer, Taiho, and Kyowa Kirin. SS received Grants and honoraria from Taiho, Eisai, Chugai, Takeda, MSD, AstraZeneca, Daiichi-Sankyo, Novartis, Takeda, Daiichi Sankyo Eli Lilly, Pfizer, Taiho, Ono and Nippon Kayaku. He is also an advisory Board of Chugai, Astra Zeneca, Eli Lilly, Pfizer, Kyowa Kirin Daiichi Sankyo and MSD and the executive board member of JBCRG, JBCS JSMO, and BIG. The other authors declare no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sakai, T., Kutomi, G., Shien, T. et al. The Japanese Breast Cancer Society Clinical Practice Guidelines for surgical treatment of breast cancer, 2022 edition. Breast Cancer 31, 1–7 (2024). https://doi.org/10.1007/s12282-023-01510-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01510-0