Abstract
Purpose
Pain is a leading cause of disability worldwide and is highly prevalent among breast cancer survivors. Pain and quality of life (QOL) are associated in breast cancer patients undergoing active treatment, but little is known about the relationship between the two in long-term survivors.
Methods
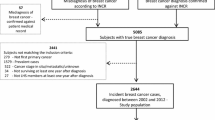
We evaluated associations between pain information collected during a 5-year post-diagnosis follow-up survey and QOL assessed by the SF-36 during a 10-year post-diagnosis survey for 2828 participants in the Shanghai Breast Cancer Survival Study.
Results
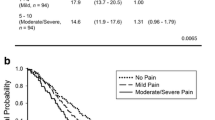
The mean overall QOL score was 78.7 for the entire study population and decreased as pain severity and frequency measured at the 5-year timepoint increased (none: 81.9, mild: 75.9, moderate/severe: 70.4, infrequent: 76.7, frequent: 72.3; P < 0.001). Significant inverse associations were found between pain and all QOL domains, including pain at 10-years post-diagnosis after multivariate adjustments. Concurrent pain was significantly and strongly associated with QOL. Most of the associations between 5-years post-diagnosis pain and QOL at 10-years post-diagnosis persisted after further adjustment for concurrent pain.
Conclusions
Pain is associated prospectively and concurrently with poor QOL among long-term breast cancer survivors. Programs to manage pain are needed to improve QOL among breast cancer survivors.

Similar content being viewed by others
Data availability
All data supporting this study's findings are present in the text or Appendix.
References
Pham T-M, et al. Average lifespan shortened due to breast cancer in Australia, 1990–2015. Breast Cancer. 2021;28(6):1389–91.
DeSantis C, et al. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64(1):52–62.
Myers ER, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA. 2015;314(15):1615–34.
Chen Z, et al. Trends of female and male breast cancer incidence at the global, regional, and national levels, 1990–2017. Breast Cancer Res Treat. 2020;180(2):481–90.
Hurwitz EL, et al. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. 2018;27(6):796–801.
Smith D, et al. Chronic pain and mortality: a systematic review. PLoS ONE. 2014;9(6): e99048.
Leadley RM, et al. Healthy aging in relation to chronic pain and quality of life in Europe. Pain Pract. 2014;14(6):547–58.
Cooney MA, et al. Current knowledge of pain after breast cancer treatment: a systematic review. Pain Manag Nurs. 2013;14(2):110–23.
Hamood R, et al. Chronic pain and other symptoms among breast cancer survivors: prevalence, predictors, and effects on quality of life. Breast Cancer Res Treat. 2018;167(1):157–69.
Bredal IS, et al. Chronic pain in breast cancer survivors: comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J Pain Sympt Manag. 2014;48(5):852–62.
Jung BF, et al. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain. 2005;118(2):10–4.
Farrar JT, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58.
Jensen MP, et al. Pain in long-term breast cancer survivors: frequency, severity, and impact. Pain Med. 2010;11(7):1099–106.
Z B, et al. Reliability and validity of a Short-Form Health Survey Scale (SF-36), Chinese version used in an elderly population of Zhejiang province in China. Zhonghua liu xing bing xue za zhi= Zhonghua liuxingbingxue zazhi. 2008;29(12):1193–8.
Zhou K, et al. Reliability, validity, and sensitivity of the Chinese Short-Form 36 Health Survey version 2 (SF-36v2) in women with breast cancer. J Eval Clin Pract. 2019;25(5):864–72.
Cella D, Fallowfield LJ. Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res Treat. 2008;107(2):167–80.
Schmitz KH, et al. Prospective surveillance and management of cardiac toxicity and health in breast cancer survivors. Cancer. 2012;118(S8):2270–6.
Gold M, et al. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97–105.
So WKW, et al. Anxiety, depression and quality of life among Chinese breast cancer patients during adjuvant therapy. Eur J Oncol Nurs. 2010;14(1):17–22.
Leung J, Pachana NA, McLaughlin D. Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology. 2014;23(9):1014–20.
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58(1):M82–91.
Sun Y, Shigaki CL, Armer JM. Return to work among breast cancer survivors: a literature review. Support Care Cancer. 2017;25(3):709–18.
Bower JE, et al. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29(26):3517–22.
Miaskowski CA. Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Onclo Nurs Forum. 1969;33(5):E79–89.
Cheng KKF, Lee DTF. Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol. 2011;78(2):127–37.
McBeth J, et al. Chronic widespread pain predicts physical inactivity: results from the prospective EPIFUND study. Eur J Pain. 2010;14(9):972–9.
Grasdalsmoen M, et al. Physical exercise and chronic pain in university students. PLoS One. 2020;15(6): e0235419.
Forsythe LP, et al. Pain in long-term breast cancer survivors: the role of body mass index, physical activity, and sedentary behavior. Breast Cancer Res Treat. 2013;137(2):617–30.
Yin M, et al. Chronic pain and its correlates among long-term breast cancer survivors. J Cancer Surviv. 2022;17:460–7.
Chou C-H, Hwang C-L, Ying-Tai Wu. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil. 2012;93(2):237–44.
Liberman K, et al. The effects of exercise on muscle strength, body composition, physical functioning and the inflammatory profile of older adults: a systematic review. Curr Opin Clin Nutr Metab Care. 2017;20(1):30–53.
Sebba A. Pain: a review of interleukin-6 and its roles in the pain of rheumatoid arthritis. Open Access Rheumatol. 2021;13:31.
Liu L, et al. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun. 2012;26(5):706–13.
Bower JE. Cancer-related fatigue: links with inflammation in cancer patients and survivors. Brain Behav Immun. 2007;21(7):863–71.
Hajj J, et al. Sleep quality, fatigue, and quality of life in individuals with heart failure. J Nurse Pract. 2020;16(6):461–5.
Sherry HY, et al. Burden of sleep and fatigue in US adults with atopic dermatitis. Dermatitis®. 2016;27(2):50–8.
Veauthier C, Paul F. Sleep disorders in multiple sclerosis and their relationship to fatigue. Sleep Med. 2014;15(1):5–14.
Ancoli-Israel S, et al. Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer. 2014;22(9):2535–45.
Fortner BV, et al. Sleep and quality of life in breast cancer patients. J Pain Sympt Manag. 2002;24(5):471–80.
Choy EHS. The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 2015;11(9):513–20.
Chen P, et al. Sleep deprivation worsened oral ulcers and delayed healing process in an experimental rat model. Life Sci. 2019;232: 116594.
Pilevarzadeh M, et al. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. 2019;176(3):519–33.
Reyes-Gibby CC, et al. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health. 2012;21(3):311–8.
Chen X, et al. Exercise, tea consumption, and depression among breast cancer survivors. J Clin Oncol. 2010;28(6):991.
Berna C, et al. Induction of depressed mood disrupts emotion regulation neurocircuitry and enhances pain unpleasantness. Biol Psychiatry. 2010;67(11):1083–90.
Hughes S, et al. Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinology. 2014;42:38–44.
Green CR, Hart-Johnson T, Loeffler DR. Cancer-related chronic pain: examining quality of life in diverse cancer survivors. Cancer. 2011;117(9):1994–2003.
Rodriguez C, et al. Cancer pain and quality of life. J Hosp Palliat Nurs. 2019;21(2):116–23.
Cramer JD, Johnson JT, Nilsen ML. Pain in head and neck cancer survivors: prevalence, predictors, and quality-of-life impact. Otolaryngol Head Neck Surg. 2018;159(5):853–8.
Esnaola NF, et al. Pain and quality of life after treatment in patients with locally recurrent rectal cancer. J Clin Oncol. 2002;20(21):4361–7.
Mystakidou K, et al. The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep. 2007;30(6):737–42.
Berg T, Maarten J, et al. Quality of life of patients with irritable bowel syndrome is low compared to others with chronic diseases. Eur J Gastroenterol Hepatol. 2006;18(5):475–81.
Dobrota D, Vesna, et al. The impact of neuropathic pain and other comorbidities on the quality of life in patients with diabetes. Health Qual Life Outcomes. 2014;12:1–8.
Wahl AK, et al. The complexity of the relationship between chronic pain and quality of life: a study of the general Norwegian population. Qual Life Res. 2009;18:971–80.
Gärtner R, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–92.
Bruce J, et al. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer. 2012;107(6):937–46.
Peuckmann V, et al. Chronic pain and other sequelae in long-term breast cancer survivors: nationwide survey in Denmark. Eur J Pain. 2009;13(5):478–85.
Grisold W, Cavaletti G, Windebank AJ. Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol. 2012;14(suppl_4):iv45–54.
Andersen KG, et al. Predictive factors for the development of persistent pain after breast cancer surgery. Pain. 2015;156(12):2413–22.
Leysen L, et al. Risk factors of pain in breast cancer survivors: a systematic review and meta-analysis. Support Care Cancer. 2017;25:3607–43.
Juhl AA, Christiansen P, Damsgaard TE. Persistent pain after breast cancer treatment: a questionnaire-based study on the prevalence, associated treatment variables, and pain type. J Breast Cancer. 2016;19(4):447–54.
Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37:29–42.
Syrjala KL, et al. Psychological and behavioral approaches to cancer pain management. J Clin Oncol. 2014;32(16):1703.
Eccleston C, Morley SJ, Williams ACDC. Psychological approaches to chronic pain management: evidence and challenges. Br J Anaesth. 2013;111(1):59–63.
Van Dartel SAA, et al. Association between fatigue and pain in rheumatoid arthritis: does pain precede fatigue or does fatigue precede pain? Arthritis Care Res. 2013;65(6):862–9.
Acknowledgements
Research reported in this publication was supported by the U.S. Department of Defense Breast Cancer Research Program (DAMD 17-02-1-0607 to Xiao-Ou Shu) and the National Cancer Institute of the National Institutes of Health under Award Number (R01 CA118229 to Xiao-Ou Shu). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The authors want to thank the study participants and research team members for their dedication to the study.
Funding
Research reported in this publication was supported by the U.S. Department of Defense Breast Cancer Research Program (DAMD 17-02-1-0607 to Xiao-Ou Shu) and the National Cancer Institute of the National Institutes of Health under Award Number (R01 CA118229 to Xiao-Ou Shu).
Author information
Authors and Affiliations
Contributions
All authors contributed to study design and conception. Data collection and assembly were performed by KG and XS. Data analysis was performed by MY and HC. The first draft of the manuscript was written by MY. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Institutional review board
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Vanderbilt University Medical Center.
Informed consent
Patient consent was waived. This study exclusively utilized de-identified information extracted from medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
About this article
Cite this article
Yin, M., Gu, K., Cai, H. et al. Association between chronic pain and quality of life in long-term breast cancer survivors: a prospective analysis. Breast Cancer 30, 785–795 (2023). https://doi.org/10.1007/s12282-023-01472-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01472-3