Abstract
Purpose
Chronic pain is a common symptom affecting quality of life for breast cancer survivors. However, its prevalence and correlate factors in long-term breast cancer survivors, particularly Asian women, are understudied. The reported study is to address these knowledge gaps.
Methods
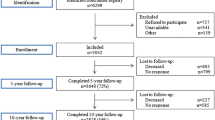
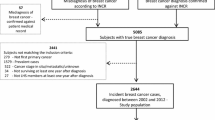
We evaluated pain severity and frequency, and their associations with clinical features and lifestyle factors among 3640 5-year breast cancer survivors who participated in the Shanghai Breast Cancer Survival Study. Demographic, clinical, and lifestyle information was collected at study enrollment, which occurred 6 months post-diagnosis, and pain was assessed at the 5-year post-diagnosis follow-up survey.
Results
In total, 42% of participants reported experiencing pain. Pain is more prevalent among survivors with low educational attainment or low income. Multivariable polytomous regression analyses showed that pain was positively associated with metastasis or recurrence (moderate pain OR: 2.17, 95% CI: 1.45, 3.26, frequent pain OR: 1.92, 95% CI: 1.37, 2.70), triple negative status (infrequent pain OR: 1.36, 95% CI: 1.04, 1.78), obesity (frequent pain OR: 1.80, 95% CI: 1.41, 2.31), and multiple comorbidities. Exercise (OR: 0.65, 95%: 0.49, 0.88), chemotherapy (OR: 0.59, 95% CI: 0.41, 0.849), and HER2-positive and ER/PR-negative status (OR: 0.64, 95% CI: 0.43, 0.97) were inversely associated with moderate pain.
Conclusions
Chronic pain is highly prevalent among long-term breast cancer survivors in China and was associated with obesity, physical inactivity, and several clinical factors.
Implications for Cancer Survivors
This study highlights the importance of promoting weight control and exercise to alleviate chronic pain.
Similar content being viewed by others
References
Siegel RL, et al. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21654.
Cao W, et al. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. 2021;134(7):783–91. https://doi.org/10.1097/CM9.0000000000001474.
Zeng H, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6(5):e555–67.
Mokhatri-Hesari P, Montazeri A. Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual life Outcomes. 2020;18(1):338. https://doi.org/10.1186/s12955-020-01591-x.
Cooney MA, et al. Current knowledge of pain after breast cancer treatment: a systematic review. Pain Manage Nurs : Off J Am Soc Pain Manage Nurses. 2013;14(2):110–23. https://doi.org/10.1016/j.pmn.2010.09.002.
Hamood R, et al. Chronic pain and other symptoms among breast cancer survivors: prevalence, predictors, and effects on quality of life. Breast Cancer Res Treat. 2018;167(1):157–69. https://doi.org/10.1007/s10549-017-4485-0.
Li J-X. Pain and depression comorbidity: a preclinical perspective. Behav Brain Res. 2015;276:92–8.
Buscemi V, et al. The role of perceived stress and life stressors in the development of chronic musculoskeletal pain disorders: a systematic review. J Pain. 2019;20.10:1127–39.
Hurwitz EL, et al. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. 2018;27.6:796–801.
Leysen L, et al. Risk factors of pain in breast cancer survivors: a systematic review and meta-analysis. Support Care Cancer : Off J Multinational Assoc Support Care Cancer. 2017;25(12):3607–43. https://doi.org/10.1007/s00520-017-3824-3.
Gärtner R, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–92. https://doi.org/10.1001/jama.2009.1568.
Bredal S, Inger, et al. Chronic pain in breast cancer survivors: comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J Pain Symptom Manage. 2014;48(5):852–62. https://doi.org/10.1016/j.jpainsymman.2013.12.239.
Reis, Andréa Dias et al. Effect of exercise on pain and functional capacity in breast cancer patients. Health and quality of life outcomes 2018 16,1 58. https://doi.org/10.1186/s12955-018-0882-2
Hughes S, et al. Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinology. 2014;42:38–44. https://doi.org/10.1016/j.psyneuen.2013.12.016.
Wang F, Cai H, Gu K, et al. Adherence to dietary recommendations among long-term breast cancer survivors and cancer outcome associations. Cancer Epidemiol Biomarkers Prev. 2020;29(2):386–95.
Shu XO, et al. Soy food intake and breast cancer survival. JAMA. 2009;302(22):2437–43. https://doi.org/10.1001/jama.2009.1783.
Rief W, et al. Long-term course of pain in breast cancer survivors: a 4-year longitudinal study. Breast Cancer Res treat. 2011;130(2):579–86. https://doi.org/10.1007/s10549-011-1614-zA.
Cramer JD, et al. Pain in head and neck cancer survivors: prevalence, predictors, and quality-of-life impact. Otolaryngol Head Neck Surg Off J Am Acad Otolaryngol Head Neck Surg. 2018;159(5):853–8. https://doi.org/10.1177/0194599818783964.
Mols F, et al. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41(17):2613–9.
Delanian S, Lefaix J-L, Pradat P-F. Radiation-induced neuropathy in cancer survivors. Radiother Oncol. 2012;105(3):273–82.
Grisold W, Cavaletti G, Anthony J. Windebank. Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro-oncology. 2012;14(suppl_4):iv45–54.
Bhagra A, Rao RD. Chemotherapy-induced neuropathy Current oncology reports. 2007;9(4):290–9.
Sisignano M, et al. Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nature Rev Neurol. 2014;10(12):694–707.
Brandolini L, et al. Chemokine signaling in chemotherapy-induced neuropathic pain. Int J Mol Sci. 2019;20.12:2904.
Alfano CM, et al. Inflammatory cytokines and comorbidity development in breast cancer survivors versus noncancer controls: evidence for accelerated aging? J Clin Oncol : Off J Am Soc Clin Oncol. 2017;35(2):149–56. https://doi.org/10.1200/JCO.2016.67.1883.
Davison SN, et al. The prevalence and severity of chronic pain in patients with chronic kidney disease: a systematic review and meta-analysis. Can J Kidney Health Dis. 2021;8:2054358121993995. https://doi.org/10.1177/2054358121993995.
Noormohammadpour P, et al. Prevalence of chronic neck pain, low back pain, and knee pain and their related factors in community-dwelling adults in Iran: a population-based national study. Clin J Pain. 2017;33(2):181–7. https://doi.org/10.1097/AJP.0000000000000396.
Parsons S, et al. Self-reported pain severity is associated with a history of coronary heart disease. Eur J Pain (London, England). 2015;19(2):167–75. https://doi.org/10.1002/ejp.533.
Bondesson E, Larrosa Pardo F, Stigmar K, Ringqvist Å, Petersson IF, Jöud A, Schelin MEC. Comorbidity between pain and mental illness - evidence of a bidirectional relationship. Eur J Pain. 2018;22(7):1304–11. https://doi.org/10.1002/ejp.1218.
Church D. Reductions in pain, depression, and anxiety symptoms after PTSD remediation in veterans. Explore (NY). 2014;10(3):162–9. https://doi.org/10.1016/j.explore.2014.02.005.
Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res. 2015;8:399–408. https://doi.org/10.2147/JPR.S55598.
Arranz L-I, et al. Effects of obesity on function and quality of life in chronic pain conditions. Curr Rheumatol Rep. 2014;16(1):390. https://doi.org/10.1007/s11926-013-0390-7.
Landmark T, et al. Longitudinal associations between exercise and pain in the general population-the HUNT pain study. PloS one. 2013;8.6:e65279.
Sluka KA, Law LF, Bement MH. Exercise-induced pain and analgesia? Underlying Mech Clin Transl Pain. 2018;159(Suppl 1):S91.
Daenen L, et al. Exercise, not to exercise, or how to exercise in patients with chronic pain? Applying science to practice. Clin J Pain. 2015;31.2:108–14.
Andersen KG, et al. Predictive factors for the development of persistent pain after breast cancer surgery. Pain. 2015;156(12):2413–22. https://doi.org/10.1097/j.pain.0000000000000298.
Bruce J, et al. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer. 2012;107(6):937–46. https://doi.org/10.1038/bjc.2012.341.
Macdonald L, Bruce J, Scott NW, Smith WC, Chambers WA. Long-term follow-up of breast cancer survivors with post-mastectomy pain syndrome. Br J Cancer. 2005;92(2):225–30. https://doi.org/10.1038/sj.bjc.6602304.
Khan QJ, O’Dea AP, Sharma P. Musculoskeletal adverse events associated with adjuvant aromatase inhibitors. J Oncol. 2010;2010:654348. https://doi.org/10.1155/2010/654348.
Andersen Hammond E, Pitz M, Shay B. Neuropathic pain in taxane-induced peripheral neuropathy: evidence for exercise in treatment. Neurorehabil Neural Repair. 2019;33(10):792–9. https://doi.org/10.1177/1545968319860486.
Acknowledgements
The authors want to thank the study participants and research team members for their dedication to the study.
Funding
Research reported in this publication was supported by the U.S. Department of Defense Breast Cancer Research Program (DAMD 17–02-1–0607 to Xiao-Ou Shu); the National Cancer Institute of the National Institutes of Health under Award Number (R01 CA118229 to Xiao-Ou Shu), and National Natural Science Foundation of China (81402734 to Pingping Bao). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yin, M., Wang, C., Gu, K. et al. Chronic pain and its correlates among long-term breast cancer survivors. J Cancer Surviv 17, 460–467 (2023). https://doi.org/10.1007/s11764-022-01241-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01241-9