Abstract
Purpose
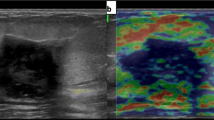
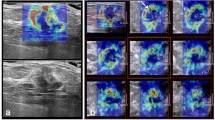
To compare the addition of diagnostic strain elastography (SE) and shear wave elastography (SWE) values to the conventional B-mode ultrasonography in differentiating between benign and malignant breast masses by qualitative and quantitative assessments.
Materials and methods
B-mode ultrasound, SE, and SWE were simultaneously performed using one ultrasound system in 148 breast masses; 88 of them were malignant. The breast imaging reporting and data system category in the B-mode, Tsukuba score (SETsu), Fat-Lesion-Ratio (SEFLR) in SE, and five-point color assessment (SWEcol) and elasticity values (SWEela) in SWE were assessed. The results were compared using the area under the receiver-operating characteristic curve (AUC).
Result
The AUC for B-mode and each elastography were similar (B-mode, 0.889; SETsu, 0.885; SEFLR, 0.875; SWEcol, 0.881; SWEela, 0.885; P > 0.05). The combined sets between B-mode and either of the elastography technique showed good diagnostic performance (B-mode + SETsu, 0.903; B-mode + SEFLR, 0.909; B-mode + SWEcol, 0.919; B-mode + SWEela, 0.914). B-mode + SWEcol and B-mode + SWEela showed a higher AUC than B-mode alone (P = 0.026 and 0.029), and B-mode + SETsu and B-mode + SEFLR showed comparable AUC to B-mode alone (P = 0.196 and 0.085). There was no significant difference between qualitative and quantitative assessments for the combined sets of B-mode and elastography (P > 0.05).
Conclusion
The addition of both SE and SWE to B-mode ultrasound improved the diagnostic performance with increased AUC, and especially SWE was more useful than SE, and no significant difference was found between qualitative and quantitative assessments.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Kornecki A. Current status of breast ultrasound. Can Assoc Radiol J. 2011;62:31–40.
Hooley RJ, Scoutt LM, Philpotts LE. Breast ultrasonography: state of the art. Radiology. 2013;268:642–59.
D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA. ACR BI-RADS atlas, breast imaging reporting and data system. Reston, VA: American College of Radiology; 2013.
Rao AA, Feneis J, Lalonde C, Ojeda-Fournier H. A pictorial review of changes in the BI-RADS fifth edition. Radiographics. 2016;36:623–39.
Choi EJ, Lee EH, Kim YM, Chang YW, Lee JH, Park YM, et al. Interobserver agreement in breast ultrasound categorization in the mammography and ultrasonography study for breast cancer screening effectiveness (MUST-BE) trial: results of a preliminary study. Ultrasonography. 2018;38:172–80.
Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, Barr RG, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography, part 1: basic principles and terminology. Ultrasound Med Biol. 2015;41:1126–47.
Garra BS, Cespedes EI, Ophir J, Spratt SR, Zuurbier RA, Magnant CM, et al. Elastography of breast lesions: initial clinical results. Radiology. 1997;202:79–86.
Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50.
Sadigh G, Carlos RC, Neal CH. Dwamena BA. Ultrasonographic differentiation of malignant from benign breast lesions: a meta-analytic comparison of elasticity and BIRADS scoring. Breast Cancer Res Treat. 2012;133:23–35.
Athanasiou A, Tardivon A, Tanter M, Sigal-Zafrani B, Bercoff J, Deffieux T, et al. Breast lesions: quantitative elastography with supersonic shear imaging–preliminary results. Radiology. 2010;256:297–303.
Xu H, Rao M, Varghese T, Sommer A, Baker S, Hall TJ, et al. Axial-shear strain imaging for differentiating benign and malignant breast masses. Ultrasound Med Biol. 2010;36:1813–24.
Berg WA, Cosgrove DO, Doré CJ, Schäfer FK, Svensson WE, Hooley RJ, et al. Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology. 2012;262:435–49.
Evans A, Whelehan P, Thomson K, Brauer K, Jordan L, Purdie C, et al. Differentiating benign from malignant solid breast masses: value of shear wave elastography according to lesion stiffness combined with greyscale ultrasound according to BI-RADS classification. Br J Cancer. 2012;107:224–9.
Song EJ, Sohn YM, Seo M. Diagnostic performances of shear-wave elastography and B-mode ultrasound to differentiate benign and malignant breast lesions: the emphasis on the cutoff value of qualitative and quantitative parameters. Clin Imaging. 2018;50:302–7.
Chang JM, Won JK, Lee KB, Park IA, Yi A, Moon WK. Comparison of shear-wave and strain ultrasound elastography in the differentiation of benign and malignant breast lesions. AJR Am J Roentgenol. 2013;201:347–56.
Youk JH, Son EJ, Gweon HM, Kim H, Park YJ, Kim JA. Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol. 2014;40:2336–44.
Seo M, Ahn HS, Park SH, Lee JB, Choi BI, Sohn YM, et al. Comparison and combination of strain and shear wave elastography of breast masses for differentiation of benign and malignant lesions by quantitative assessment: preliminary study. J Ultrasound Med. 2018;37:99–109.
Kim HJ, Kim SM, Kim B, La Yun B, Jang M, Ko Y, et al. Comparison of strain and shear wave elastography for qualitative and quantitative assessment of breast masses in the same population. Sci Rep. 2018;8:6197.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;25(139):891–906.
Desmedt C, Haibe-Kains B, Wirapati P, Buyse M, Larsimont D, Bontempi G, et al. Biological processes associated with breast cancer clinical outcome depend on the molecular subtypes. Clin Cancer Res. 2008;14:5158–65.
Fujioka T, Kubota K, Kikuchi Y, Tsuchiya J, Tateishi U, Kasaharak M, et al. The feasibility of using 18F-FDG-PET/CT in patients with mucinous breast carcinoma. Nucl Med Commun. 2018;39:1033–8.
Fujioka T, Kubota K, Toriihara A, Machida Y, Okazawa K, Nakagawa T, et al. Tumor characteristics of ductal carcinoma in situ of breast visualized on [F-18] fluorodeoxyglucose-positron emission tomography/computed tomography: results from a retrospective study. World J Radiol. 2016;28(8):743–9.
Chang JM, Park IA, Lee SH, Kim WH, Bae MS, Koo HR, et al. Stiffness of tumours measured by shear-wave elastography correlated with subtypes of breast cancer. Eur Radiol. 2013;23:2450–8.
Youk JH, Gweon HM, Son EJ, Kim JA, Jeong J. Shear-wave elastography of invasive breast cancer: correlation between quantitative mean elasticity value and immunohistochemical profile. Breast Cancer Res Treat. 2013;138:119–26.
Evans A, Whelehan P, Thomson K, McLean D, Brauer K, Purdie C, et al. Invasive breast cancer: relationship between shear-wave elastographic findings and histologic prognostic factors. Radiology. 2012;263:673–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This manuscript has not been published and is not under consideration for publication elsewhere. All the authors have read the manuscript and have approved this submission. All the authors and their institution have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fujioka, T., Mori, M., Kubota, K. et al. Simultaneous comparison between strain and shear wave elastography of breast masses for the differentiation of benign and malignant lesions by qualitative and quantitative assessments. Breast Cancer 26, 792–798 (2019). https://doi.org/10.1007/s12282-019-00985-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-019-00985-0