Abstract
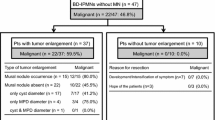
Aim of our update is to present the “state of art” about pancreatic intraductal papillary mucinous neoplasms (IPMN) and underline some significant notions that can be helpful in clinical practice. IPMN of the pancreas can be defined as neoplasms derived from pancreatic ductal system that produce mucin. The real incidence and prevalence of IPMN are not well defined. The radiological classification subdivides IPMN in three categories, in according to ductal involvement. One of the most confounding factors about pancreatic IPMN regards the high heterogeneity of these lesions, from which derives a different biological behavior and a different management. Although there are no clinical signs related to pancreatic IPMN, patient’s medical history and clinical examination are relevant. The differential diagnosis is relevant in order to detect potentially malignant lesions. Preoperative imaging should confirm the diagnosis of IPMN, indicate the risk of malignant cystic neoplasia, and define resectability. Data from literature showed that surgical treatment is indicated in case of main duct-IPMN, in concordance with the international consensus guidelines for management of IPMNs. Surgery is not mandatory in all patients with branch duct-IPMN, but only in 20% of cases or less; furthermore, in the absence of malignancy-related signs, careful non-operative management seems to be safe and effective in asymptomatic patients.



Similar content being viewed by others
References
Gaujoux S, Brennan MF, Gonen M, D’Angelica MI, DeMatteo R, Fong Y, Schattner M, DiMaio C, Janakos M, Jarnagin WR, Allen PJ (2011) Cystic lesions of the pancreas: changes in the presentation and management of 1,424 patients at a single institution over a 15-year time period. J Am Coll Surg. 212(4):590–600. discussion 600-3
Del Chiaro M, Segersvärd R, Pozzi Mucelli R, Rangelova E, Kartalis N, Ansorge C, Arnelo U, Blomberg J, Löhr M, Verbeke C (2014) Comparison of preoperative conference-based diagnosis with histology of cystic tumors of the pancreas. Ann Surg Oncol 21(5):1539–1544
Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL (2017) Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 17(5):738–753
Schietroma M, Pessia B, Mattei A, Romano L, Giuliani A, Carlei F (2020) Temperature-neutrophils-multiple organ failure grading for complicated intra-abdominal infections. Surg Infect (Larchmt) 21(1):69–74. https://doi.org/10.1089/sur.2019.092
Vege SS, Ziring B, Jain R, Moayyedi P, Clinical Guidelines Committee; American Gastroenterology Association (2015) American Gastroenterological Association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 148(4):819–22
Giuliani A, Lazzarin G, Romano L, Coletti G, Vicentini V, Fatayer MWA, Schietroma M, Valiyeva S, Carlei F (2019) A case report of three synchronous tumors in the same pancreatic specimen. Ann Med Surg (Lond) 44:79–82
Marchegiani G, Mino-Kenudson M, Sahora K, Morales-Oyarvide V, Thayer S, Ferrone C, Warshaw AL, Lillemoe KD, Fernández-Del CC (2015) IPMN involving the main pancreatic duct: biology, epidemiology, and long-term outcomes following resection. Ann Surg 261(5):976–983
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, Yamaguchi K, Yamao K, Matsuno S, International Association of Pancreatology (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 6(1–2):17–32
Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K, International Association of Pancreatology (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 12(3):183–97
McDonald JM, Williard W, Mais D, Beitler A (2000) The incidence of intraductal papillary mucinous tumors of the pancreas. Curr Surg 57(6):610–614
Reid-Lombardo KM, St Sauver J, Li Z, Ahrens WA, Unni KK, Que FG (2008) Incidence, prevalence, and management of intraductal papillary mucinous neoplasm in Olmsted County, Minnesota, 1984–2005: a population study. Pancreas 37(2):139–144
Klibansky DA, Reid-Lombardo KM, Gordon SR, Gardner TB (2012) The clinical relevance of the increasing incidence of intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol 10(5):555–558
Chang YR, Park JK, Jang JY, Kwon W, Yoon JH, Kim SW (2016) Incidental pancreatic cystic neoplasms in an asymptomatic healthy population of 21,745 individuals: large-scale, single-center cohort study. Medicine (Baltimore). 95(51):e5535
Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, Johnson PT, Fishman EK, Hruban RH (2008) Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol 191(3):802–807
Lee KS, Sekhar A, Rofsky NM, Pedrosa I (2010) Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol 105(9):2079–2084
De Oliveira PB, Puchnick A, Szejnfeld J, Goldman SM (2015) Prevalence of incidental pancreatic cysts on 3 tesla magnetic resonance. PLoS One. 10(3):e0121317
Sey MS, Teagarden S, Settles D, McGreevy K, Coté GA, Sherman S, McHenry L, LeBlanc JK, Al-Haddad M, DeWitt JM (2015) Prospective cross-sectional study of the prevalence of incidental pancreatic cysts during routine outpatient endoscopic ultrasound. Pancreas 44(7):1130–1133
Ferrone CR, Correa-Gallego C, Warshaw AL, Brugge WR, Forcione DG, Thayer SP, Fernández-del CC (2009) Current trends in pancreatic cystic neoplasms. Arch Surg 144(5):448–454
Kimura W, Nagai H, Kuroda A, Muto T, Esaki Y (1995) Analysis of small cystic lesions of the pancreas. Int J Pancreatol 18(3):197–206
Yoon WJ, Lee JK, Lee KH, Ryu JK, Kim YT, Yoon YB (2008) Cystic neoplasms of the exocrine pancreas: an update of a nationwide survey in Korea. Pancreas 37(3):254–258
Ingkakul T, Warshaw AL, Fernández-Del CC (2011) Epidemiology of intraductal papillary mucinous neoplasms of the pancreas: sex differences between 3 geographic regions. Pancreas 40(5):779–780
Aronsson L, Andersson R, Ansari D (2017) Intraductal papillary mucinous neoplasm of the pancreas - epidemiology, risk factors, diagnosis, and management. Scand J Gastroenterol 52(8):803–815
Wada K, Takaori K, Traverso LW (2015) Screening for pancreatic cancer. Surg Clin North Am 95(5):1041–1052
Canto MI, Hruban RH, Fishman EK, Kamel IR, Schulick R, Zhang Z, Topazian M, Takahashi N, Fletcher J, Petersen G, Klein AP, Axilbund J, Griffin C, Syngal S, Saltzman JR, Mortele KJ, Lee J, Tamm E, Vikram R, Bhosale P, Margolis D, Farrell J, Goggins M, American Cancer of the Pancreas Screening (CAPS) Consortium (2012) Frequent detection of pancreatic lesions in asymptomatic high-risk individuals. Gastroenterology. 142(4):796–804
Shoda J, Kano M, Asano T, Irimura T, Ueda T, Iwasaki R, Furukawa M, Kamiya J, Nimura Y, Todoroki T, Matsuzaki Y, Tanaka N (1999) Secretory low-molecular-weight phospholipases A2 and their specific receptor in bile ducts of patients with intrahepatic calculi: factors of chronic proliferative cholangitis. Hepatology 29(4):1026–1036
Lazzarin G, Romano L, Coletti G, Di Sibio A, Vicentini V, Fatayer MWA, Schietroma M, Pessia B, Leone M, Carlei F, Giuliani A (2020) Branch duct - IPMN and PanIN, in IgG4-autoimmune pancreatitis: a case report. Clin Case Rep 8(11):2111–2115. https://doi.org/10.1002/ccr3.2641
Le’clerc Nicolas J, Romano L, Giuliani A (2020) Acute pancreatitis: an overview. Minerva Gastroenterol Dietol 66(3):290–291. https://doi.org/10.23736/S1121-421X.20.02681-1
Grützmann R, Post S, Saeger HD, Niedergethmann M (2011) Intraductal papillary mucinous neoplasia (IPMN) of the pancreas: its diagnosis, treatment, and prognosis. Dtsch Arztebl Int 108(46):788–794
Mirarchi M, De Raffele E, Santini D, Calculli L, Cuicchi D, Lecce F, Cola B (2016) Multifocal intraductal papillary mucinous neoplasm of the pancreas from mild dysplasia to invasive carcinoma a case report. Ann Ital Chir 87:97–102
Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, Benson AB 3rd, Binder E, Cardin DB, Cha C, Chiorean EG, Chung V, Czito B, Dillhoff M, Dotan E, Ferrone CR, Hardacre J, Hawkins WG, Herman J, Ko AH, Komanduri S, Koong A, LoConte N, Lowy AM, Moravek C, Nakakura EK, O’Reilly EM, Obando J, Reddy S, Scaife C, Thayer S, Weekes CD, Wolff RA, Wolpin BM, Burns J, Darlow S (2017) Pancreatic adenocarcinoma, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 15(8):1028–1061
Sahora K, Fernández-del Castillo C, Dong F, Marchegiani G, Thayer SP, Ferrone CR, Sahani DV, Brugge WR, Warshaw AL, Lillemoe KD, Mino-Kenudson M (2014) Not all mixed-type intraductal papillary mucinous neoplasms behave like main-duct lesions: implications of minimal involvement of the main pancreatic duct. Surgery 156(3):611–621
Salvia R, Crippa S, Falconi M, Bassi C, Guarise A, Scarpa A, Pederzoli P (2007) Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut 56(8):1086–1090
Del Chiaro M, Beckman R, Ateeb Z, Orsini N, Rezaee N, Manos L, Valente R, Yuan C, Ding D, Margonis GA, Yin L, Cameron JL, Makary MA, Burkhart RA, Weiss MJ, He J, Arnelo U, Yu J, Wolfgang CL (2019) Main duct dilatation is the best predictor of high-grade dysplasia or invasion in intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. https://doi.org/10.1097/SLA.0000000000003174
Maguchi H, Tanno S, Mizuno N, Hanada K, Kobayashi G, Hatori T, Sadakari Y, Yamaguchi T, Tobita K, Doi R, Yanagisawa A, Tanaka M (2011) Natural history of branch duct intraductal papillary mucinous neoplasms of the pancreas: a multicenter study in Japan. Pancreas. 40(3):364–70
Sadakari Y, Ienaga J, Kobayashi K, Miyasaka Y, Takahata S, Nakamura M, Mizumoto K, Tanaka M (2010) Cyst size indicates malignant transformation in branch duct intraductal papillary mucinous neoplasm of the pancreas without mural nodules. Pancreas 39(2):232–236
Shin SH, Han DJ, Park KT, Kim YH, Park JB, Kim SC (2010) Validating a simple scoring system to predict malignancy and invasiveness of intraductal papillary mucinous neoplasms of the pancreas. World J Surg 34(4):776–783
Adsay V, Mino-Kenudson M, Furukawa T, Basturk O, Zamboni G, Marchegiani G, Bassi C, Salvia R, Malleo G, Paiella S, Wolfgang CL, Matthaei H, Offerhaus GJ, Adham M, Bruno MJ, Reid MD, Krasinskas A, Klöppel G, Ohike N, Tajiri T, Jang KT, Roa JC, Allen P, Fernández-del Castillo C, Jang JY, Klimstra DS, Hruban RH, Members of Verona Consensus Meeting, 2013 (2016) Pathologic evaluation and reporting of intraductal papillary mucinous neoplasms of the pancreas and other tumoral intraepithelial neoplasms of pancreatobiliary tract: recommendations of Verona consensus meeting. Ann Surg. 263(1):162–77
Uehara H, Ishikawa O, Katayama K, Kawada N, Ikezawa K, Fukutake N, Takakura R, Takano Y, Tanaka S, Takenaka A (2011) Size of mural nodule as an indicator of surgery for branch duct intraductal papillary mucinous neoplasm of the pancreas during follow-up. J Gastroenterol 46(5):657–663
Hirono S, Tani M, Kawai M, Okada K, Miyazawa M, Shimizu A, Kitahata Y, Yamaue H (2012) The carcinoembryonic antigen level in pancreatic juice and mural nodule size are predictors of malignancy for branch duct type intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 255(3):517–522
Jang JY, Kim SW, Lee SE, Yang SH, Lee KU, Lee YJ, Kim SC, Han DJ, Choi DW, Choi SH, Heo JS, Cho BH, Yu HC, Yoon DS, Lee WJ, Lee HE, Kang GH, Lee JM (2008) Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: when can we operate or observe? Ann Surg Oncol 15(1):199–205
Kim KW, Park SH, Pyo J, Yoon SH, Byun JH, Lee MG, Krajewski KM, Ramaiya NH (2014) Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Ann Surg 259(1):72–81
Kalluri R, Zeisberg M (2006) Fibroblasts in cancer. Nat Rev Cancer 6(5):392–401
Polanska UM, Orimo A (2013) Carcinoma-associated fibroblasts: non-neoplastic tumour-promoting mesenchymal cells. J Cell Physiol 228(8):1651–1657
Shindo K, Aishima S, Ohuchida K, Fujino M, Mizuuchi Y, Hattori M, Ohtsuka T, Tokunaga S, Mizumoto K, Tanaka M, Oda Y (2014) Podoplanin expression in the cyst wall correlates with the progression of intraductal papillary mucinous neoplasm. Virchows Arch 465(3):265–273
Salvia R, Fernández-del Castillo C, Bassi C, Thayer SP, Falconi M, Mantovani W, Pederzoli P, Warshaw AL (2004) Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 239(5):678–85. discussion 685-7
Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N, Campbell KA, Lillemoe KD (2004) Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 239(6):788–97. discussion 797-9
Crippa S, Bassi C, Salvia R, Malleo G, Marchegiani G, Rebours V, Levy P, Partelli S, Suleiman SL, Banks PA, Ahmed N, Chari ST, Fernández-Del Castillo C, Falconi M (2017) Low progression of intraductal papillary mucinous neoplasms with worrisome features and high-risk stigmata undergoing non-operative management: a mid-term follow-up analysis. Gut 66(3):495–506
Romano L, Giuliani A, Vicentini V, Schietroma M, Carlei F (2021) Basics for surgeons about the immunohistochemistry role in pancreatic NETs diagnosis. Eur Rev Med Pharmacol Sci 25(6):2548–2553. https://doi.org/10.26355/eurrev_202103_25418
Valiyeva S, Romano L, Schietroma M, Carlei F, Giuliani A. Partial agenesis of dorsal pancreas. Report of two cases. Int J Surg Case Rep. 2020 Oct 10:S2210–2612(20)30907-X. https://doi.org/10.1016/j.ijscr.2020.10.029.
Pessia B, Giuliani A, Romano L, Bruno F, Carlei F, Vicentini V, Schietroma M (2021) The role of sarcopenia in the pancreatic adenocarcinoma. Eur Rev Med Pharmacol Sci 25(10):3670–3678. https://doi.org/10.26355/eurrev_202105_25933
Acknowledgements
The authors acknowledge Dr Walid Mohammad Fatayer, Dr Beatrice Pessia, Dr Alessandra Di Sibio, and Dr Vincenzo Vicentini for their contribution in literature search and in providing the images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lazzarin, G., Romano, L., Schietroma, M. et al. Intraductal Papillary Mucinous Neoplasms (IPMN) of the Pancreas: an Update in Definition, Time to Progression, and Surgical Management. Indian J Surg 84 (Suppl 2), 448–457 (2022). https://doi.org/10.1007/s12262-022-03394-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03394-4