Abstract
Purpose of Review
We reviewed the recent literature to identify and summarize new research surrounding anterior cruciate ligament reconstruction (ACLR) with augmentation in the form of additional soft tissue procedures or biologic augmentation. Specifically, we wanted to review the failure rates of these procedures in both the primary and revision settings.
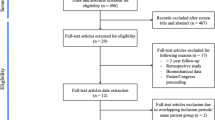
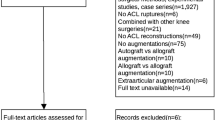
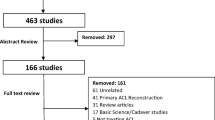
Methods
The databases Embase, PubMed, and Medline were searched on August 13, 2018, for English-language studies that reported on the use of anterior cruciate ligament reconstruction (primary and revision) in conjunction with either soft tissue or biologic augmentation. The studies were systematically screened and data abstracted in duplicates.
Recent Findings
Advancements in ACLR surgery, including soft tissue augmentation, may decrease primary and revision surgery failure rates for high-risk patients. The use of biological augmentation has shown histologic and radiographic improvements. These differences, however, have failed to be statistically significant and have not resulted in clinically significant improvements in outcome.
Summary
The limited body of evidence has shown that the addition of soft tissue procedures may in fact lower the risk of graft re-rupture rates particularly in revision or in patients wishing to return to high-risk sports and activities. The use of biologic augmentation although promising in laboratory studies has yet to show any significant clinical results and therefore will require further studies to prove any efficacy.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1):1–8.
Grassi A, Kim C, Marcheggiani Muccioli GM, Zaffagnini S, Amendola A. What is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop. 2017;475(10):2484–99.
LaPrade RF, Dragoo JL, Koh JL, Murray IR, Geeslin AG, Chu CR. AAOS research symposium updates and consensus: biologic treatment of orthopaedic injuries. J Am Acad Orthop Surg. 2016;24(7):17.
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–8.
Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ, et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):870–7.
Cerciello S, Batailler C, Darwich N, Neyret P. Extra-articular tenodesis in combination with anterior cruciate ligament reconstruction. Clin Sports Med. 2018;37(1):87–100.
• Ibrahim SA, Shohdy EM, Marwan Y, Ramadan SA, Almisfer AK, Mohammad MW, et al. Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: a randomized clinical trial. Am J Sports Med. 2017;45(7):1558–66 Randomized control trial examining outcomes of ACL vs ACL + ALL reconstruction directly. Authors found no difference in outcomes over 2-year follow-up period. Largest RCT identified for ACL + ALL reconstruction identified for this review.
Thaunat M, Clowez G, Saithna A, Cavalier M, Choudja E, Vieira TD, et al. Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: a series of 548 patients from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med. 2017;45(11):2569–77.
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med. 2017;45(7):1547–57.
Louis M-L, D’ingrado P, Ehkirch FP, Bertiaux S, Colombet P, Sonnery-Cottet B, et al. Combined intra- and extra-articular grafting for revision ACL reconstruction: a multicentre study by the French Arthroscopy Society (SFA). Orthop Traumatol Surg Res. 2017;103(8):S223–9.
Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, Roberti di Sarsina T, Raggi F, Signorelli C, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45(14):3233–42.
Imbert P, Lustig S, Steltzlen C, Batailler C, Colombet P, Dalmay F, et al. Midterm results of combined intra- and extra-articular ACL reconstruction compared to historical ACL reconstruction data. Multicenter study of the French Arthroscopy Society. Orthop Traumatol Surg Res. 2017;103(8):S215–21.
Imbert P, Belvedere C, Leardini A. Knee laxity modifications after ACL rupture and surgical intra- and extra-articular reconstructions: intra-operative measures in reconstructed and healthy knees. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2725–35.
Panisset JC, Pailhé R, Schlatterer B, Sigwalt L, Sonnery-Cottet B, Lutz C, et al. Short-term complications in intra- and extra-articular anterior cruciate ligament reconstruction. Comparison with the literature on isolated intra-articular reconstruction. A multicenter study by the French Arthroscopy Society. Orthop Traumatol Surg Res. 2017;103(8):S231–6.
Alessio-Mazzola M, Formica M, Russo A, Sanguineti F, Capello A, Lovisolo S, et al. Outcome after combined lateral extra-articular tenodesis and anterior cruciate ligament revision in professional soccer players. J Knee Surg [Internet]. 2018 Sep 18 [cited 2018 Dec 5]; Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0038-1672120.
Walters BL, Porter DA, Hobart SJ, Bedford BB, Hogan DE, McHugh MM, et al. Effect of intraoperative platelet-rich plasma treatment on postoperative donor site knee pain in patellar tendon autograft anterior cruciate ligament reconstruction: a double-blind randomized controlled trial. Am J Sports Med. 2018;46(8):1827–35.
Valentí Nin JR, Mora Gasque G, Valentí Azcárate A, Aquerreta Beola JD, Hernandez Gonzalez M. Has platelet-rich plasma any role in anterior cruciate ligament allograft healing? Arthrosc J Arthrosc Relat Surg. 2009;25(11):1206–13.
Seijas R, Rius M, Ares O, García-Balletbó M, Serra I, Cugat R. Healing of donor site in bone-tendon-bone ACL reconstruction accelerated with plasma rich in growth factors: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):991–7.
Gaunder CL, Bastrom T, Pennock AT. Segond fractures are not a risk factor for anterior cruciate ligament reconstruction failure. Am J Sports Med. 2017;45(14):3210–5.
Neyret P, Palomo JR, Donell ST, Dejour H. Extra-articular tenodesis for anterior cruciate ligament rupture in amateur skiers. Br J Sports Med. 1994;28(1):31–4.
Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169–76.
Guzzini M, Mazza D, Fabbri M, Lanzetti R, Redler A, Iorio C, et al. Extra-articular tenodesis combined with an anterior cruciate ligament reconstruction in acute anterior cruciate ligament tear in elite female football players. Int Orthop. 2016;40(10):2091–6.
•• Hexter AT, Thangarajah T, Blunn G, Haddad FS. Biological augmentation of graft healing in anterior cruciate ligament reconstruction: a systematic review. Bone Jt J. 2018;100-B(3):271–84 Excellent systemic review examining all of the studies involving biological augmentation of ACL surgery including basic science and animal models which for the purpose of this article were only mentioned briefly as they were not in clinical trials yet.
Andriolo L, Di Matteo B, Kon E, Filardo G, Venieri G, Marcacci M. PRP augmentation for ACL reconstruction. Biomed Res Int. 2015;2015:1–15.
Eriksson K, Kindblom L-G, Wredmark T. Semitendinosus tendon graft ingrowth in tibial tunnel following ACL reconstruction: a histological study of 2 patients with different types of early graft failure. Acta Orthop Scand. 2000;71(3):275–9.
Lu H, Chen C, Xie S, Tang Y, Qu J. Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: a systematic review of histological results. J Knee Surg [Internet]. 2018 May 21 [cited 2018 Dec 17]; Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0038-1653964.
Radice F, Yánez R, Gutiérrez V, Rosales J, Pinedo M, Coda S. Comparison of magnetic resonance imaging findings in anterior cruciate ligament grafts with and without autologous platelet-derived growth factors. Arthrosc J Arthrosc Relat Surg. 2010;26(1):50–7.
Sánchez M, Anitua E, Azofra J, Prado R, Muruzabal F, Andia I. Ligamentization of tendon grafts treated with an endogenous preparation rich in growth factors: gross morphology and histology. Arthrosc J Arthrosc Relat Surg. 2010;26(4):470–80.
Vadalà A, Iorio R, De Carli A, Ferretti M, Paravani D, Caperna L, et al. Platelet-rich plasma: does it help reduce tunnel widening after ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2013;21(4):824–9.
de Almeida AM, Demange MK, Sobrado MF, Rodrigues MB, Pedrinelli A, Hernandez AJ. Patellar tendon healing with platelet-rich plasma: a prospective randomized controlled trial. Am J Sports Med. 2012;40(6):1282–8.
Cervellin M, de Girolamo L, Bait C, Denti M, Volpi P. Autologous platelet-rich plasma gel to reduce donor-site morbidity after patellar tendon graft harvesting for anterior cruciate ligament reconstruction: a randomized, controlled clinical study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):114–20.
Figueroa D, Figueroa F, Calvo R, Vaisman A, Ahumada X, Arellano S. Platelet-rich plasma use in anterior cruciate ligament surgery: systematic review of the literature. Arthrosc J Arthrosc Relat Surg. 2015;31(5):981–8.
Magnussen RA, Flanigan DC, Pedroza AD, Heinlein KA, Kaeding CC. Platelet rich plasma use in allograft ACL reconstructions: two-year clinical results of a MOON cohort study. Knee. 2013;20(4):277–80.
Kawai T, Yamada T, Yasukawa A, Koyama Y, Muneta T, Takakuda K. Anterior cruciate ligament reconstruction using chitin-coated fabrics in a rabbit model. Artif Organs. 2010;34(1):55–64.
Li H, Chen S, Wu Y, Jiang J, Ge Y, Gao K, et al. Enhancement of the osseointegration of a polyethylene terephthalate artificial ligament graft in a bone tunnel using 58S bioglass. Int Orthop. 2012;36(1):191–7.
Cho S, Li H, Chen C, Jiang J, Tao H, Chen S. Cationised gelatin and hyaluronic acid coating enhances polyethylene terephthalate artificial ligament graft osseointegration in porcine bone tunnels. Int Orthop. 2013;37(3):507–13.
Vaquette C, Viateau V, Guérard S, Anagnostou F, Manassero M, Castner DG, et al. The effect of polystyrene sodium sulfonate grafting on polyethylene terephthalate artificial ligaments on in vitro mineralisation and in vivo bone tissue integration. Biomaterials. 2013;34(29):7048–63.
Bi F, Shi Z, Liu A, Guo P, Yan S. Anterior cruciate ligament reconstruction in a rabbit model using silk-collagen scaffold and comparison with autograft. Liu X, editor PLOS ONE 2015;10(5):e0125900.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Michael D. Riediger, Devon Stride, Sarah E. Coke, Adrian Z. Kurz, and Andrew Duong each declare no potential conflicts of interest.
Olufemi R. Ayeni is on the speaker’s bureau for Conmed and Smith & Nephew and is a section editor for Current Reviews in Musculoskeletal Medicine.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Rights and permissions
About this article
Cite this article
Riediger, M.D., Stride, D., Coke, S.E. et al. ACL Reconstruction with Augmentation: a Scoping Review. Curr Rev Musculoskelet Med 12, 166–172 (2019). https://doi.org/10.1007/s12178-019-09548-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-019-09548-4