Abstract
Purpose of Review
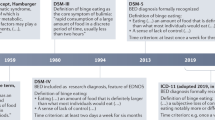
Binge eating disorder (BED) is characterized by recurrent binge eating episodes (i.e., eating an objectively large amount of food accompanied by a sense of loss of control while eating) in the absence of regular compensatory behavior. BED follows a chronic course marked by significant dysfunction and impairment. This review focuses on advances in the understanding of BED, including its diagnosis, correlates, risk factors, and treatment, with particular attention to the past 5 to 8 years.
Recent Findings
BED remains the most common eating disorder in the USA and globally. BED occurs across the lifespan and among diverse gender, racial, and ethnic groups. Risk for and maintenance of BED results from multiple psychological, biological, and sociocultural factors. First-line treatment for reducing binge eating is cognitive behavioral therapy, with efficacy for interpersonal psychotherapy as well. Lisdexamfetamine is an FDA-approved medication for moderate to severe cases of BED.
Summary
Even with advances in its diagnosis and treatment, better assessment and understanding of BED in diverse gender, racial, and ethnic populations is needed. Studies of shared risk factors underlying BED and comorbid disorders may lead to a greater understanding of mechanisms for intervention. Future research should prioritize evaluating the implementation of established treatments among populations in need, as well as establishing new interventions that can be scaled for delivery in real-world settings. Given overlap between BED and overweight/obesity, a continued focus on developing treatments that effectively address binge eating and weight management is warranted.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Claudino AM, Pike KM, Hay P, Keeley JW, Evans SC, Rebello TJ, et al. The classification of feeding and eating disorders in the ICD-11: results of a field study comparing proposed ICD-11 guidelines with existing ICD-10 guidelines. BMC Med. 2019;17(1):93. https://doi.org/10.1186/s12916-019-1327-4.
Forney KJ, Bodell LP, Haedt-Matt AA, Keel PK. Incremental validity of the episode size criterion in binge-eating definitions: an examination in women with purging syndromes. Int J Eat Disord. 2016;49(7):651–62. https://doi.org/10.1002/eat.22508.
Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. Int J Eat Disord. 2003;34(Suppl):S96–106. https://doi.org/10.1002/eat.10209.
Kornstein SG. Epidemiology and recognition of binge-eating disorder in psychiatry and primary care. J Clin Psychiatry. 2017;78(Suppl 1):3–8. https://doi.org/10.4088/JCP.sh16003su1c.01.
Lindvall Dahlgren C, Wisting L, Rø Ø. Feeding and eating disorders in the DSM-5 era: a systematic review of prevalence rates in non-clinical male and female samples. J Eat Disord. 2017;5:56. https://doi.org/10.1186/s40337-017-0186-7.
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73(9):904–14. https://doi.org/10.1016/j.biopsych.2012.11.020.
Micali N, Martini MG, Thomas JJ, Eddy KT, Kothari R, Russell E, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med. 2017;15(1):12. https://doi.org/10.1186/s12916-016-0766-4.
•• Udo T, Grilo CM. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. Adults. Biol Psychiatry. 2018;84(5):345–54. https://doi.org/10.1016/j.biopsych.2018.03.014This study examined the prevalence and psychological correlates of BED in a large U.S. sample with diverse representation in terms of race, ethnicity, gender, and age. They reported that BED occurs across the lifetime in all of the gender, race, and ethnicity groups, with few differences between groups. They found that BED was characterized by unique differences in age of onset, persistence and duration, rates of obesity, and psychosocial impairment compared to the other eating disorders, supporting its clinical significance and distinctiveness.
Hay P, Girosi F, Mond J. Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. J Eat Disord. 2015;3:19. https://doi.org/10.1186/s40337-015-0056-0.
Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol. 2017;126(1):38–51. https://doi.org/10.1037/abn0000219.
Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav Res Ther. 2011;49(10):622–7. https://doi.org/10.1016/j.brat.2011.06.009.
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–13. https://doi.org/10.1093/ajcn/nqy342.
Coelho JS, Suen J, Clark BA, Marshall SK, Geller J, Lam PY. Eating disorder diagnoses and symptom presentation in transgender youth: a scoping review. Curr Psychiatry Rep. 2019;21(11):107. https://doi.org/10.1007/s11920-019-1097-x.
Wildes JE, Forbush KT. Ethnicity as a risk factor for eating disorders. The Wiley Handbook of Eating Disorders. 2015;1:324–37. https://doi.org/10.1016/j.eatbeh.2018.11.004.
Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44(5):412–20. https://doi.org/10.1002/eat.20787.
Goode RW, Cowell MM, Mazzeo SE, Cooper-Lewter C, Forte A, Olayia OI, et al. Binge eating and binge-eating disorder in black women: a systematic review. Int J Eat Disord. 2020;53(4):491–507. https://doi.org/10.1002/eat.23217.
Yu KY, Pope SC, Perez M. Clinical treatment and practice recommendations for disordered eating in Asian Americans. Prof Psychol Res Pract. 2019;50(5):279–87. https://doi.org/10.1037/pro0000244.
Coffino JA, Udo T, Grilo CM. Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin Proc. 2019a;94(8):1415–26. https://doi.org/10.1016/j.mayocp.2019.02.030.
Lydecker JA, Grilo CM. Different yet similar: examining race and ethnicity in treatment-seeking adults with binge eating disorder. J Consult Clin Psychol. 2016;84(1):88–94. https://doi.org/10.1037/ccp0000048.
Bartlett BA, Mitchell KS. Eating disorders in military and veteran men and women: a systematic review. Int J Eat Disord. 2015;48(8):1057–69. https://doi.org/10.1002/eat.22454.
Lauder TD, Williams MV, Campbell CS, Davis G, Sherman R, Pulos E. The female athlete triad: prevalence in military women. Mil Med. 1999;164(9):630–5. https://doi.org/10.1097/00005768-199805001-00617.
Higgins DM, Dorflinger L, MacGregor KL, Heapy AA, Goulet JL, Ruser C. Binge eating behavior among a national sample of overweight and obese veterans. Obesity (Silver Spring). 2013;21(5):900–3. https://doi.org/10.1002/oby.20160.
Masheb RM, Kutz AM, Marsh AG, Min KM, Ruser CB, Dorflinger LM. "Making weight" during military service is related to binge eating and eating pathology for veterans later in life. Eat Weight Disord. 2019;24(6):1063–70. https://doi.org/10.1007/s40519-019-00766-w.
Blais RK, Brignone E, Maguen S, Carter ME, Fargo JD, Gundlapalli AV. Military sexual trauma is associated with post-deployment eating disorders among Afghanistan and Iraq veterans. Int J Eat Disord. 2017;50(7):808–16. https://doi.org/10.1002/eat.22705.
Cuthbert K, Hardin S, Zelkowitz R, Mitchell K. Eating disorders and overweight/obesity in veterans: prevalence, risk factors, and treatment considerations. Curr Obes Rep. 2020;9(2):98–108. https://doi.org/10.1007/s13679-020-00374-1.
Rasmusson G, Lydecker JA, Coffino JA, White MA, Grilo CM. Household food insecurity is associated with binge-eating disorder and obesity. Int J Eat Disord. 2018;52:28–35. https://doi.org/10.1002/eat.22990.
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. 2000. http://www.esourceresearch.org/Portals/0/Uploads/Documents/Public/fsguide.pdf.
Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health. 2012;37(1):253–64. https://doi.org/10.1007/s10900-011-9420-4.
Bruening M, MacLehose R, Loth K, Story M, Neumark-Sztainer D. Feeding a family in a recession: food insecurity among Minnesota parents. Am J Public Health. 2012;102(3):520–6. https://doi.org/10.2105/ajph.2011.300390.
Bove CF, Olson CM. Obesity in low-income rural women: qualitative insights about physical activity and eating patterns. Women Health. 2006;44(1):57–78. https://doi.org/10.1300/J013v44n01_04.
Becker CB, Middlemass KM, Gomez F, Martinez-Abrego A. Eating disorder pathology among individuals living with food insecurity: a replication study. Clin Psychol Sci. 2019;7(5):1144–58. https://doi.org/10.1177/2167702619851811.
Fairburn CG. Overcoming binge eating: The proven program to learn why you binge and how you can stop. Guilford Press; 2013.
Vanderlinden J, Schoevaerts K, Simons A, Van Den Eede U, Bruffaerts R, Serra R, et al. Sociodemographic and clinical characteristics of eating disorder patients treated in the specialized residential settings in Belgium. Eat Weight Disord. 2020. https://doi.org/10.1007/s40519-020-00867-x.
Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2013;122(2):445–57. https://doi.org/10.1037/a0030679.
Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord. 2005;38(2):112–22. https://doi.org/10.1002/eat.20158.
Schlüter N, Schmidt R, Kittel R, Tetzlaff A, Hilbert A. Loss of control eating in adolescents from the community. Int J Eat Disord. 2016;49(4):413–20. https://doi.org/10.1002/eat.22488.
Hilbert A, Hartmann AS, Czaja J, Schoebi D. Natural course of preadolescent loss of control eating. J Abnorm Psychol. 2013;122(3):684–93. https://doi.org/10.1037/a0033330.
Schaumberg K, Jangmo A, Thornton LM, Birgegård A, Almqvist C, Norring C, et al. Patterns of diagnostic transition in eating disorders: a longitudinal population study in Sweden. Psychol Med. 2019;49(5):819–27. https://doi.org/10.1017/s0033291718001472.
Brownley KA, Berkman ND, Peat CM, Lohr KN, Cullen KE, Bann CM, et al. Binge-eating disorder in adults: a systematic review and meta-analysis. Ann Intern Med. 2016;165(6):409–20. https://doi.org/10.7326/m15-2455.
Wilfley DE, Citrome L, Herman BK. Characteristics of binge eating disorder in relation to diagnostic criteria. Neuropsychiatr Dis Treat. 2016;12:2213–23. https://doi.org/10.2147/ndt.s107777.
Meany G, Conceicao E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22(2):87–91. https://doi.org/10.1002/erv.2273.
Perez M, Warren CS. The relationship between quality of life, binge-eating disorder, and obesity status in an ethnically diverse sample. Obesity (Silver Spring). 2012;20(4):879–85. https://doi.org/10.1038/oby.2011.89.
Mitchell JE. Medical comorbidity and medical complications associated with binge-eating disorder. Int J Eat Disord. 2016;49(3):319–23. https://doi.org/10.1002/eat.22452.
Welch E, Jangmo A, Thornton LM, Norring C, von Hausswolff-Juhlin Y, Herman BK, et al. Treatment-seeking patients with binge-eating disorder in the Swedish national registers: clinical course and psychiatric comorbidity. BMC Psychiatry. 2016;16:163. https://doi.org/10.1186/s12888-016-0840-7.
Karaca S, Saleh A, Canan F, Potenza MN. Comorbidity between behavioral addictions and attention deficit/hyperactivity disorder: a systematic review. Int J Mental Health Addict. 2017;15(3):701–24. https://doi.org/10.1007/s11469-016-9660-8.
Bogusz K, Kopera M, Jakubczyk A, Trucco EM, Kucharska K, Walenda A, Wojnar M. Prevalence of alcohol use disorder among individuals who binge eat: A systematic review and meta‐analysis. Addiction. 2020. https://doi.org/10.1111/add.15155.
Coffino JA, Udo T, Grilo CM. The significance of overvaluation of shape or weight in binge-eating disorder: results from a national sample of U.S. Adults. Obesity (Silver Spring). 2019b;27(8):1367–71. https://doi.org/10.1002/oby.22539.
Mond JM, Hay PJ. Dissatisfaction versus over-evaluation in a general population sample of women. Int J Eat Disord. 2011;44(8):721–6. https://doi.org/10.1002/eat.20878.
Grilo CM, White MA, Gueorguieva R, Wilson GT, Masheb RM. Predictive significance of the overvaluation of shape/weight in obese patients with binge eating disorder: findings from a randomized controlled trial with 12-month follow-up. Psychol Med. 2013;43(6):1335–44. https://doi.org/10.1017/s0033291712002097.
Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120(1):108–18. https://doi.org/10.1037/a0021406.
Balantekin KN, Birch LL, Savage JS. Eating in the absence of hunger during childhood predicts self-reported binge eating in adolescence. Eat Behav. 2017;24:7–10. https://doi.org/10.1016/j.eatbeh.2016.11.003.
Giel KE, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder-a systematic update of the evidence. Nutrients. 2017;9(11):1170. https://doi.org/10.3390/nu9111170.
Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14(2):155–70. https://doi.org/10.1177/1073191106295527.
Fischer S, Smith GT, Cyders MA. Another look at impulsivity: a meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clin Psychol Rev. 2008;28(8):1413–25. https://doi.org/10.1016/j.cpr.2008.09.001.
Berg JM, Latzman RD, Bliwise NG, Lilienfeld SO. Parsing the heterogeneity of impulsivity: a meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychol Assess. 2015;27(4):1129–46. https://doi.org/10.1037/pas0000111.
Davis HA, Smith GT. An integrative model of risk for high school disordered eating. J Abnorm Psychol. 2018;127(6):559–70. https://doi.org/10.1037/abn0000365.
Goldschmidt AB, Wall MM, Zhang J, Loth KA, Neumark-Sztainer D. Overeating and binge eating in emerging adulthood: 10-year stability and risk factors. Dev Psychol. 2016;52(3):475–83. https://doi.org/10.1037/dev0000086.
Kenny TE, Singleton C, Carter JC. An examination of emotion-related facets of impulsivity in binge eating disorder. Eat Behav. 2019;32:74–7. https://doi.org/10.1016/j.eatbeh.2018.12.006.
Wolz I, Granero R, Fernández-Aranda F. A comprehensive model of food addiction in patients with binge-eating symptomatology: the essential role of negative urgency. Compr Psychiatry. 2017;74:118–24. https://doi.org/10.1016/j.comppsych.2017.01.012.
Manasse SM, Espel HM, Schumacher LM, Kerrigan SG, Zhang F, Forman EM, et al. Does impulsivity predict outcome in treatment for binge eating disorder? A multimodal investigation. Appetite. 2016;105:172–9. https://doi.org/10.1016/j.appet.2016.05.026.
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity--a systematic review. Neurosci Biobehav Rev. 2015;49:125–34. https://doi.org/10.1016/j.neubiorev.2014.12.008.
Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137(4):660–81. https://doi.org/10.1037/a0023660.
Duchesne M, de Oliveira Falcone EM, de Freitas SR, D'Augustin JF, Marinho V, Appolinario JC. Assessment of interpersonal skills in obese women with binge eating disorder. J Health Psychol. 2012;17(7):1065–75. https://doi.org/10.1177/1359105311432326.
Ivanova IV, Tasca GA, Hammond N, Balfour L, Ritchie K, Koszycki D, et al. Negative affect mediates the relationship between interpersonal problems and binge-eating disorder symptoms and psychopathology in a clinical sample: a test of the interpersonal model. Eur Eat Disord Rev. 2015;23(2):133–8. https://doi.org/10.1002/erv.2344.
Ivanova IV, Tasca GA, Proulx G, Bissasda H. Contribution of interpersonal problems to eating disorder psychopathology via negative affect in treatment-seeking men and women: testing the validity of the interpersonal model in an understudied population. Clin Psychol Psychother. 2017;24(4):952–64. https://doi.org/10.1002/cpp.2060.
Meule A. Back by popular demand: a narrative review on the history of food addiction research. Yale J Biol Med. 2015;88(3):295–302. https://doi.org/10.5281/zenodo.48115.
Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL. The prevalence of food addiction as assessed by the Yale food addiction scale: a systematic review. Nutrients. 2014;6(10):4552–90. https://doi.org/10.3390/nu6104552.
Kittel R, Brauhardt A, Hilbert A. Cognitive and emotional functioning in binge-eating disorder: a systematic review. Int J Eat Disord. 2015;48(6):535–54. https://doi.org/10.1002/eat.22419.
Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016;44:125–39. https://doi.org/10.1016/j.cpr.2016.02.001.
Hilbert A. Binge-eating disorder. Psychiatr Clin North Am. 2019;42(1):33–43. https://doi.org/10.1016/j.psc.2018.10.011.
Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, et al. Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. Am J Clin Nutr. 2010;91(6):1568–73. https://doi.org/10.3945/ajcn.2010.29203.
Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr. 2013;167(2):149–55. https://doi.org/10.1001/2013.jamapediatrics.12.
Micali N, Solmi F, Horton NJ, Crosby RD, Eddy KT, Calzo JP, et al. Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. J Am Acad Child Adolesc Psychiatry. 2015;54(8):652–9.e1. https://doi.org/10.1016/j.jaac.2015.05.009.
McElroy SL. Pharmacologic treatments for binge-eating disorder. J Clin Psychiatry. 2017;78(Suppl 1):14–9. https://doi.org/10.4088/JCP.sh16003su1c.03.
Reas DL, Grilo CM. Pharmacological treatment of binge eating disorder: update review and synthesis. Expert Opin Pharmacother. 2015;16(10):1463–78. https://doi.org/10.1517/14656566.2015.1053465.
•• Hilbert A, Petroff D, Herpertz S, Pietrowsky R, Tuschen-Caffier B, Vocks S, et al. Meta-analysis of the efficacy of psychological and medical treatments for binge-eating disorder. J Consult Clin Psychol. 2019;87(1):91–105. https://doi.org/10.1037/ccp0000358This study presents results of a meta-analysis for treatments for BED, allowing for careful comparisons of the effectiveness between existing treatments and analysis of moderators.
Grilo CM, Reas DL, Mitchell JE. Combining pharmacological and psychological treatments for binge eating disorder: current status, limitations, and future directions. Curr Psychiatry Rep. 2016;18(6):55. https://doi.org/10.1007/s11920-016-0696-z.
Peat CM, Berkman ND, Lohr KN, Brownley KA, Bann CM, Cullen K, et al. Comparative effectiveness of treatments for binge-eating disorder: systematic review and network meta-analysis. Eur Eat Disord Rev. 2017;25(5):317–28. https://doi.org/10.1002/erv.2517.
Niego SH, Kofman MD, Weiss JJ, Geliebter A. Binge eating in the bariatric surgery population: a review of the literature. Int J Eat Disord. 2007;40(4):349–59. https://doi.org/10.1002/eat.20376.
Goldschmidt AB, Conceição EM, Thomas JG, Mitchell JE, Raynor HA, Bond DS. Conceptualizing and studying binge and loss of control eating in bariatric surgery patients-time for a paradigm shift? Surg Obes Relat Dis. 2016;12(8):1622–5. https://doi.org/10.1016/j.soard.2016.09.008.
Grilo CM. Psychological and behavioral treatments for binge-eating disorder. J Clin Psychiatry. 2017;78(Suppl 1):20–4. https://doi.org/10.4088/JCP.sh16003su1c.04.
Iacovino JM, Gredysa DM, Altman M, Wilfley DE. Psychological treatments for binge eating disorder. Curr Psychiatry Rep. 2012;14(4):432–46. https://doi.org/10.1007/s11920-012-0277-8.
Linardon J, Wade TD, de la Piedad Garcia X, Brennan L. The efficacy of cognitive-behavioral therapy for eating disorders: a systematic review and meta-analysis. J Consult Clin Psychol. 2017;85(11):1080–94. https://doi.org/10.1037/ccp0000245.
Linardon J, Messer M, Fuller-Tyszkiewicz M. Meta-analysis of the effects of cognitive-behavioral therapy for binge-eating-type disorders on abstinence rates in nonrandomized effectiveness studies: comparable outcomes to randomized, controlled trials? Int J Eat Disord. 2018;51(12):1303–11. https://doi.org/10.1002/eat.22986.
Peterson CB, Engel SG, Crosby RD, Strauman T, Smith TL, Klein M, et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: a randomized controlled trial. Int J Eat Disord. 2020;53:1418–27. https://doi.org/10.1002/eat.23324.
Fitzsimmons-Craft EE, Taylor CB, Graham AK, Sadeh-Sharvit S, Balantekin KN, Eichen DM, et al. Effectiveness of a digital cognitive-behavior therapy guided self-help intervention for eating disorders in college women: a cluster randomized clinical trial. JAMA Network Open. 2020;3(8):e2015633. https://doi.org/10.1001/jamanetworkopen.2020.15633.
Hildebrandt T, Michaelides A, Mackinnon D, Greif R, DeBar L, Sysko R. Randomized controlled trial comparing smartphone assisted versus traditional guided self-help for adults with binge eating. Int J Eat Disord. 2017;50(11):1313–22. https://doi.org/10.1002/eat.22781.
Wagner B, Nagl M, Dölemeyer R, Klinitzke G, Steinig J, Hilbert A, et al. Randomized controlled trial of an internet-based cognitive-behavioral treatment program for binge-eating disorder. Behav Ther. 2016;47(4):500–14. https://doi.org/10.1016/j.beth.2016.01.006.
Hildebrandt T, Michaeledes A, Mayhew M, Greif R, Sysko R, Toro-Ramos T, et al. Randomized controlled trial comparing health coach-delivered smartphone-guided self-help with standard care for adults with binge eating. Am J Psychiatry. 2020;177(2):134–42. https://doi.org/10.1176/appi.ajp.2019.19020184.
de Zwaan M, Herpertz S, Zipfel S, Svaldi J, Friederich HC, Schmidt F, et al. Effect of internet-based guided self-help vs individual face-to-face treatment on full or subsyndromal binge eating disorder in overweight or obese patients: the INTERBED randomized clinical trial. JAMA Psychiatry. 2017;74(10):987–95. https://doi.org/10.1001/jamapsychiatry.2017.2150.
Linardon J. Rates of abstinence following psychological or behavioral treatments for binge-eating disorder: meta-analysis. Int J Eat Disord. 2018;51(8):785–97. https://doi.org/10.1002/eat.22897.
•• Kazdin AE, Fitzsimmons-Craft EE, Wilfley DE. Addressing critical gaps in the treatment of eating disorders. Int J Eat Disord. 2017;50(3):170–89. https://doi.org/10.1002/eat.22670This paper outlines ways to address two critical research priorities for eating disorders treatment, namely, improving the translation of evidence-based treatments from research trials to real-world settings, and extending treatments to people who do not currently receive care.
Wilfley DE, Agras WS, Fitzsimmons-Craft EE, Bohon C, Eichen DM, Welch RR, et al. Training models for implementing evidence-based psychological treatment: a cluster-randomized trial in college counseling centers. JAMA Psychiatry. 2019;77:139. https://doi.org/10.1001/jamapsychiatry.2019.3483.
Linardon J, Fairburn CG, Fitzsimmons-Craft EE, Wilfley DE, Brennan L. The empirical status of the third-wave behaviour therapies for the treatment of eating disorders: a systematic review. Clin Psychol Rev. 2017;58:125–40. https://doi.org/10.1016/j.cpr.2017.10.005.
Linardon J, Gleeson J, Yap K, Murphy K, Brennan L. Meta-analysis of the effects of third-wave behavioural interventions on disordered eating and body image concerns: implications for eating disorder prevention. Cogn Behav Ther. 2019;48(1):15–38. https://doi.org/10.1080/16506073.2018.1517389.
Kenny TE, Carter JC, Safer DL. Dialectical behavior therapy guided self-help for binge-eating disorder. Eat Disord. 2020;28(2):202–11. https://doi.org/10.1080/10640266.2019.1678982.
Carter JC, Kenny TE, Singleton C, Van Wijk M, Heath O. Dialectical behavior therapy self-help for binge-eating disorder: a randomized controlled study. Int J Eat Disord. 2020;53(3):451–60. https://doi.org/10.1002/eat.23208.
Grilo CM, White MA, Masheb RM, Ivezaj V, Morgan PT, Gueorguieva R. Randomized controlled trial testing the effectiveness of adaptive "SMART" stepped-care treatment for adults with binge-eating disorder comorbid with obesity. Am Psychol. 2020;75(2):204–18. https://doi.org/10.1037/amp0000534.
Funding
This work was supported by grants from the National Institutes of Health (T32 MH082761 and K01 DK116925).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obesity and Diet
Rights and permissions
About this article
Cite this article
Davis, H.A., Graham, A.K. & Wildes, J.E. Overview of Binge Eating Disorder. Curr Cardiovasc Risk Rep 14, 26 (2020). https://doi.org/10.1007/s12170-020-00664-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12170-020-00664-2