Abstract
Purpose of Review
Eating disorders (EDs) and overweight/obesity (OW/OB) have a significant impact on veterans. This review highlights current research on EDs and OW/OB in this population.
Recent Findings
Prevalence estimates for both EDs and OW/OB among veterans remain consistent with and possibly higher than those in the general population. Both diagnoses share multiple risk factors, including trauma history, and mental health comorbidities. Although weight loss treatments have been fairly well studied among veteran samples, there are no published investigations on psychotherapies for EDs in this population. The Veterans Healthcare Administration is working to train providers in ED treatments. VHA treatments for OW/OB show some benefits and areas for improvement.
Summary
Areas for future research include structured assessments for EDs and disordered eating behaviors in veterans to clarify prevalence estimates. There is a need for interventions that consider common mechanisms for ED and OW/OB, and there is a need for more research on the associations between different types of trauma and ED/OW/OB in veterans.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bartlett BA, Mitchell KS. Eating disorders in military and veteran men and women: a systematic review. Int J Eat Disord. 2015;48(8):1057–69. https://doi.org/10.1002/eat.22454.
Livingston WS, Brignone E, Fargo JD, Gundlapalli AV, Maguen S, Blais RK. VHA-enrolled homeless veterans are at increased risk for eating disorder diagnoses. Mil Med. 2019;184(1–2):e71–e5. https://doi.org/10.1093/milmed/usy175.
Blais RK, Brignone E, Maguen S, Carter ME, Fargo JD, Gundlapalli AV. Military sexual trauma is associated with post-deployment eating disorders among Afghanistan and Iraq veterans. Int J Eat Disord. 2017;50(7):808–16. https://doi.org/10.1002/eat.22705.
Diagnostic and statistical manual of mental disorders: DSM-5. Fifth edition. Arlington, VA: American Psychiatric Association; 2013.
Arditte Hall KA, Bartlett BA, Iverson KM, Mitchell KS. Military-related trauma is associated with eating disorder symptoms in male veterans. Int J Eat Disord. 2017;50(11):1328–31. https://doi.org/10.1002/eat.22782.
Bankoff SM, Richards LK, Bartlett B, Wolf EJ, Mitchell KS. Examining weight and eating behavior by sexual orientation in a sample of male veterans. Compr Psychiatry. 2016;68:134–9. https://doi.org/10.1016/j.comppsych.2016.03.007.
• Huston JC, Grillo AR, Iverson KM, Mitchell KS, System VABH. Associations between disordered eating and intimate partner violence mediated by depression and posttraumatic stress disorder symptoms in a female veteran sample. Gen Hosp Psychiatry. 2019;58:77–82. https://doi.org/10.1016/j.genhosppsych.2019.03.007Depressive and PTSD symptoms mediated the relation between a specific trauma exposure and ED symptoms in a longitudinal study using a nationally representative sample of female veterans.
Mitchell KS, Wolf EJ. PTSD, food addiction, and disordered eating in a sample of primarily older veterans: the mediating role of emotion regulation. Psychiatry Res. 2016;243:23–9. https://doi.org/10.1016/j.psychres.2016.06.013.
Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–70. https://doi.org/10.1002/1098-108X(199412)16:4<363::AID-EAT2260160405>3.0.CO;2-%23.
Curry JF, Aubuchon-Endsley N, Brancu M, Runnals JJ, Workgroup VAM-AMWVR, Workgroup VAM-AMR, et al. Lifetime major depression and comorbid disorders among current-era women veterans. J Affect Disord. 2014;152–154:434–40. https://doi.org/10.1016/j.jad.2013.10.012.
Forman-Hoffman VL, Mengeling M, Booth BM, Torner J, Sadler AG. Eating disorders, post-traumatic stress, and sexual trauma in women veterans. Mil Med. 2012;177(10):1161–8. https://doi.org/10.7205/milmed-d-12-00041.
Litwack SD, Mitchell KS, Sloan DM, Reardon AF, Miller MW. Eating disorder symptoms and comorbid psychopathology among male and female veterans. Gen Hosp Psychiatry. 2014;36(4):406–10. https://doi.org/10.1016/j.genhosppsych.2014.03.013.
Udo T, Grilo CM. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol Psychiatry. 2018;84(5):345–54. https://doi.org/10.1016/j.biopsych.2018.03.014.
Rosenbaum DL, Kimerling R, Pomernacki A, Goldstein KM, Yano EM, Sadler AG, et al. Binge eating among women veterans in primary care: comorbidities and treatment priorities. Womens Health Issues. 2016;26(4):420–8. https://doi.org/10.1016/j.whi.2016.02.004.
Breland JY, Donalson R, Li Y, Hebenstreit CL, Goldstein LA, Maguen S. Military sexual trauma is associated with eating disorders, while combat exposure is not. Psychol Trauma. 2018;10(3):276–81. https://doi.org/10.1037/tra0000276.
Arditte Hall KA, Bartlett BA, Iverson KM, Mitchell KS. Eating disorder symptoms in female veterans: the role of childhood, adult, and military trauma exposure. Psychol Trauma. 2018;10(3):345–51. https://doi.org/10.1037/tra0000301.
Maguen S, Cohen B, Ren L, Bosch J, Kimerling R, Seal K. Gender differences in military sexual trauma and mental health diagnoses among Iraq and Afghanistan veterans with posttraumatic stress disorder. Womens Health Issues. 2012;22(1):e61–6. https://doi.org/10.1016/j.whi.2011.07.010.
Bartlett BA, Iverson KM, Mitchell KS. Intimate partner violence and disordered eating among male and female veterans. Psychiatry Res. 2018;260:98–104. https://doi.org/10.1016/j.psychres.2017.11.056.
Zinzow HM, Grubaugh AL, Monnier J, Suffoletta-Maierle S, Frueh BC. Trauma among female veterans: a critical review. Trauma Violence Abuse. 2007;8(4):384–400. https://doi.org/10.1177/1524838007307295.
Breland JY, Donalson R, Dinh JV, Maguen S. Trauma exposure and disordered eating: a qualitative study. Women Health. 2018;58(2):160–74. https://doi.org/10.1080/03630242.2017.1282398.
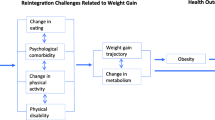
Mitchell KS, Porter B, Boyko EJ, Field AE. Longitudinal associations among posttraumatic stress disorder, disordered eating, and weight gain in military men and women. Am J Epidemiol. 2016;184(1):33–47. https://doi.org/10.1093/aje/kwv291.
Jacobson IG, Smith TC, Smith B, Keel PK, Amoroso PJ, Wells TS, et al. Disordered eating and weight changes after deployment: longitudinal assessment of a large US military cohort. Am J Epidemiol. 2009;169(4):415–27. https://doi.org/10.1093/aje/kwn366.
Warner C, Warner C, Matuszak T, Rachal J, Flynn J, Grieger TA. Disordered eating in entry-level military personnel. Mil Med. 2007;172(2):147–51. https://doi.org/10.7205/milmed.172.2.147.
Breland JY, Donalson R, Nevedal A, Dinh JV, Maguen S. Military experience can influence women’s eating habits. Appetite. 2017;118:161–7. https://doi.org/10.1016/j.appet.2017.08.009.
Bellows BK, DuVall SL, Kamauu AW, Supina D, Babcock T, LaFleur J. Healthcare costs and resource utilization of patients with binge-eating disorder and eating disorder not otherwise specified in the Department of Veterans Affairs. Int J Eat Disord. 2015;48(8):1082–91. https://doi.org/10.1002/eat.22427.
Bellows BK, DuVall SL, Kamauu AW, Supina D, Pawaskar M, Babcock T, et al. Characteristics and use of treatment modalities of patients with binge-eating disorder in the Department of Veterans Affairs. Eat Behav. 2016;21:161–7. https://doi.org/10.1016/j.eatbeh.2016.03.013.
Huston JC, Iverson KM, Mitchell KS. Associations between healthcare use and disordered eating among female veterans. Int J Eat Disord. 2018;51(8):978–83. https://doi.org/10.1002/eat.22885.
Trottier K, MacDonald DE. Update on psychological trauma, other severe adverse experiences and eating disorders: state of the research and future research directions. Curr Psychiatry Rep. 2017;19(8):45. https://doi.org/10.1007/s11920-017-0806-6.
• Breland JY, Phibbs CS, Hoggatt KJ, Washington DL, Lee J, Haskell S, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(Suppl 1):11–7. https://doi.org/10.1007/s11606-016-3962-1Using cross-sectional VHA administrative and clinical data, overweight prevalence was 37%, and obesity prevalence was 41%. Obesity prevalence estimates were notably high among black women (51%), women with schizophrenia (56%), Native Hawaiian/Pacific Islander veterans (46%), and American Indian/Alaska Native veterans (47%).
Stefanovics EA, Potenza MN, Pietrzak RH. The physical and mental health burden of obesity in U.S. veterans: results from the National Health and Resilience in Veterans Study. J Psychiatr Res. 2018;103:112–9. https://doi.org/10.1016/j.jpsychires.2018.05.016.
Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. https://doi.org/10.1001/jama.2009.2014.
• Rush T, CA LM, Crum-Cianflone NF. Obesity and associated adverse health outcomes among US military members and veterans: Findings from the millennium cohort study. Obesity (Silver Spring). 2016;24(7):1582–9. https://doi.org/10.1002/oby.21513Longitudinal data from the Millennium Cohort Study, which sampled service members and veterans across all service branches, highlights the period after separation from the military as one of acute risk for weight gain. In 2007, 51% of the sampled population had overweight, and 23% had obesity.
McDaniel JT, Thomas KH, Angel CM, Erwin MS, Nemec LP, Young BB, et al. Regional differences in BMI, obesity, and exercise frequency in a large veteran service organization: a secondary analysis of new veteran member surveys from Team Red. White & Blue Prev Med Rep. 2018;12:116–21. https://doi.org/10.1016/j.pmedr.2018.09.001.
Tarlov E, Zenk SN, Matthews SA, Powell LM, Jones KK, Slater S, et al. Neighborhood resources to support healthy diets and physical activity among US military veterans. Prev Chronic Dis. 2017;14:E111. https://doi.org/10.5888/pcd14.160590.
Pandey N, Ashfaq SN, Dauterive EW 3rd, MacCarthy AA, Copeland LA. Military sexual trauma and obesity among women veterans. J Womens Health (Larchmt). 2018;27(3):305–10. https://doi.org/10.1089/jwh.2016.6105.
Mitchell KS, Wolf EJ, Lyons MJ, Goldberg J, Magruder KM. A co-twin control study of the association between combat exposure, PTSD and obesity in male veterans. Psychol Med. 2018;48(14):2449–52. https://doi.org/10.1017/S0033291718001514.
Smith BN, Tyzik AL, Neylan TC, Cohen BE. PTSD and obesity in younger and older veterans: results from the mind your heart study. Psychiatry Res. 2015;229(3):895–900. https://doi.org/10.1016/j.psychres.2015.07.044.
LeardMann CA, Woodall KA, Littman AJ, Jacobson IG, Boyko EJ, Smith B, et al. Post-traumatic stress disorder predicts future weight change in the millennium cohort study. Obesity (Silver Spring). 2015;23(4):886–92. https://doi.org/10.1002/oby.21025.
• Buta E, Masheb R, Gueorguieva R, Bathulapalli H, Brandt CA, Goulet JL. Posttraumatic stress disorder diagnosis and gender are associated with accelerated weight gain trajectories in veterans during the post-deployment period. Eat Behav. 2018;29:8–13. https://doi.org/10.1016/j.eatbeh.2018.01.002A large longitudinal study of post-9/11 veterans found that PTSD diagnosis was associated with post-deployment weight gain for both men and women, with a stronger relation for female veterans.
Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Ann Behav Med. 2010;39(1):61–78. https://doi.org/10.1007/s12160-010-9165-9.
Farr OM, Sloan DM, Keane TM, Mantzoros CS. Stress- and PTSD-associated obesity and metabolic dysfunction: a growing problem requiring further research and novel treatments. Metabolism. 2014;63(12):1463–8. https://doi.org/10.1016/j.metabol.2014.08.009.
Hoerster KD, Campbell S, Dolan M, Stappenbeck CA, Yard S, Simpson T, et al. PTSD is associated with poor health behavior and greater body mass index through depression, increasing cardiovascular disease and diabetes risk among U.S. veterans. Prev Med Rep. 2019;15:100930. https://doi.org/10.1016/j.pmedr.2019.100930.
• Maciejewski ML, Shepherd-Banigan M, Raffa SD, Weidenbacher HJ. Systematic review of behavioral weight management program MOVE! for veterans. Am J Prev Med. 2018;54(5):704–14. https://doi.org/10.1016/j.amepre.2018.01.029This systematic review of the MOVE! weight loss program for veterans reported 12-month weight loss ranging from − 0.13 to − 3.3 kg, with < 15% of MOVE! participants achieving clinically significant weight loss. Despite greater attendance being associated with greater weight loss, no more than 25% of MOVE! enrolled veterans completed 8 or more sessions within 6 months.
Garvin JT, Marion LN, Narsavage GL, Finnegan L. Characteristics influencing weight reduction among veterans in the MOVE!(R) program. West J Nurs Res. 2015;37(1):50–65. https://doi.org/10.1177/0193945914534323.
Jackson SL, Long Q, Rhee MK, Olson DE, Tomolo AM, Cunningham SA, et al. Weight loss and incidence of diabetes with the Veterans Health Administration MOVE! lifestyle change programme: an observational study. The Lancet Diabetes & Endocrinology. 2015;3(3):173–80. https://doi.org/10.1016/s2213-8587(14)70267-0.
Chan SH, Raffa SD. Examining the dose-response relationship in the Veterans Health Administration’s MOVE!((R)) weight management program: a nationwide observational study. J Gen Intern Med. 2017;32(Suppl 1):18–23. https://doi.org/10.1007/s11606-017-3992-3.
Braun K, Erickson M, Utech A, List R, Garcia JM. Evaluation of veterans MOVE! program for weight loss. J Nutr Educ Behav. 2016;48(5):299–303.e1. https://doi.org/10.1016/j.jneb.2016.02.012.
Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107(10):1755–67. https://doi.org/10.1016/j.jada.2007.07.017.
Rutledge T, Skoyen JA, Wiese JA, Ober KM, Woods GN. A comparison of MOVE! versus TeleMOVE programs for weight loss in veterans with obesity. Obes Res Clin Pract. 2017;11(3):344–51. https://doi.org/10.1016/j.orcp.2016.11.005.
Damschroder LJ, Lutes LD, Kirsh S, Kim HM, Gillon L, Holleman RG, et al. Small-changes obesity treatment among veterans: 12-month outcomes. Am J Prev Med. 2014;47(5):541–53. https://doi.org/10.1016/j.amepre.2014.06.016.
• Lutes LD, Damschroder LJ, Masheb R, Kim HM, Gillon L, Holleman RG, et al. Behavioral treatment for veterans with obesity: 24-month weight outcomes from the ASPIRE-VA Small Changes Randomized Trial. J Gen Intern Med. 2017;32(Suppl 1):40–7. https://doi.org/10.1007/s11606-017-3987-0In a 24-month follow-up of MOVE! compared with ASPIRE-VA, a small changes weight management program, participants enrolled in the online version of ASPIRE-VA lost the most weight (− 2.13 kg). Notably, veterans with diabetes enrolled in the in-person, group format of ASPIRE-VA experienced significant weight regain (+ 2.8 kg).
Thomas DD, Waring ME, Ameli O, Reisman JI, Vimalananda VG. Patient characteristics associated with receipt of prescription weight-management medications among veterans participating in MOVE! Obesity (Silver Spring). 2019;27(7):1168–76. https://doi.org/10.1002/oby.22503.
Semla TP, Ruser C, Good CB, Yanovski SZ, Ames D, Copeland LA, et al. Pharmacotherapy for weight management in the VHA. J Gen Intern Med. 2017;32(Suppl 1):70–3. https://doi.org/10.1007/s11606-016-3949-y.
Gunnar W. Bariatric surgery provided by the Veterans Health Administration: current state and a look to the future. J Gen Intern Med. 2017;32(Suppl 1):4–5. https://doi.org/10.1007/s11606-017-3991-4.
Funk LM, Gunnar W, Dominitz JA, Eisenberg D, Frayne S, Maggard-Gibbons M, et al. A health services research agenda for bariatric surgery within the Veterans Health Administration. J Gen Intern Med. 2017;32(Suppl 1):65–9. https://doi.org/10.1007/s11606-016-3951-4.
Maciejewski ML, Arterburn DE, Van Scoyoc L, Smith VA, Yancy WS Jr, Weidenbacher HJ, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–55. https://doi.org/10.1001/jamasurg.2016.2317.
Murali SB. Long-term survival following bariatric surgery in the VA health system. JAMA. 2015;313(14):1473–4. https://doi.org/10.1001/jama.2015.2580.
Smith VA, Arterburn DE, Berkowitz TSZ, Olsen MK, Livingston EH, Yancy WS Jr, et al. Association between bariatric surgery and long-term health care expenditures among veterans with severe obesity. JAMA Surg. 2019:e193732. https://doi.org/10.1001/jamasurg.2019.3732.
Arterburn DE, Olsen MK, Smith VA, Livingston EH, Van Scoyoc L, Yancy WS Jr, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70. https://doi.org/10.1001/jama.2014.16968.
Barry RG, Amiri FA, Gress TW, Nease DB, Canterbury TD. Laparoscopic vertical sleeve gastrectomy: a 5-year veterans affairs review. Medicine (Baltimore). 2017;96(35):e7508. https://doi.org/10.1097/MD.0000000000007508.
Lee JH, Nguyen QN, Le QA. Comparative effectiveness of 3 bariatric surgery procedures: Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(5):997–1002. https://doi.org/10.1016/j.soard.2016.01.020.
Lyo V, Schafer AL, Stewart L. Roux-en-Y gastric bypass is a safe and effective option that improves major co-morbidities associated with obesity in an older, veteran population. Am J Surg. 2019;218(4):684–8. https://doi.org/10.1016/j.amjsurg.2019.07.027.
Nassour I, Almandoz JP, Adams-Huet B, Kukreja S, Puzziferri N. Metabolic syndrome remission after Roux-en-Y gastric bypass or sleeve gastrectomy. Diabetes Metab Syndr Obes. 2017;10:393–402. https://doi.org/10.2147/DMSO.S142731.
Skancke M, Schoolfield C, Grossman R, Kerns JC, Abel N, Brody F. Laparoscopic sleeve gastrectomy for morbid obesity at a veterans affairs medical center. J Laparoendosc Adv Surg Tech A. 2018;28(6):650–5. https://doi.org/10.1089/lap.2018.0002.
Vitello DJ, Beach-Bachmann J, Vitello JM. Bariatric surgery among obese veterans: a retrospective review of complications and intermediate term results from a single institution. Obes Surg. 2016;26(8):1906–11. https://doi.org/10.1007/s11695-015-2033-8.
Maggard-Gibbons M, Dawes AJ. Bariatric surgery is associated with improved long-term survival in severely obese US veterans. Evid Based Med. 2015;20(4):148. https://doi.org/10.1136/ebmed-2015-110181.
Kitamura R, Chen R, Trickey A, Eisenberg D. Positive and negative independent predictive factors of weight loss after bariatric surgery in a veteran population. Obes Surg. 2020:1–7. https://doi.org/10.1007/s11695-020-04428-0.
Chen GL, Kubat E, Eisenberg D. Prevalence of anemia 10 years after Roux-en-Y gastric bypass in a single veterans affairs medical center. JAMA Surg. 2018;153(1):86–7. https://doi.org/10.1001/jamasurg.2017.3158.
Eisenberg D, Lohnberg JA, Kubat EP, Bates CC, Greenberg LM, Frayne SM. Systems innovation model: an integrated interdisciplinary team approach pre- and post-bariatric surgery at a veterans affairs (VA) medical center. Surg Obes Relat Dis. 2017;13(4):600–6. https://doi.org/10.1016/j.soard.2016.11.007.
Grace N, Kubat E, Eisenberg D. An integrated, collaborative multidisciplinary clinic improves 12-month follow-up after bariatric surgery at a single veterans affairs medical center. Bariatric Surgical Practice and Patient Care. 2017;12(4):170–2. https://doi.org/10.1089/bari.2017.0033.
Voils CI, Adler R, Strawbridge E, Grubber J, Allen KD, Olsen MK, et al. Early-phase study of a telephone-based intervention to reduce weight regain among bariatric surgery patients. Health Psychol. 2020. https://doi.org/10.1037/hea0000835.
Batch BC, Goldstein K, Yancy WS Jr, Sanders LL, Danus S, Grambow SC, et al. Outcome by gender in the veterans health administration motivating overweight/obese veterans everywhere weight management program. J Women’s Health (Larchmt). 2018;27(1):32–9. https://doi.org/10.1089/jwh.2016.6212.
Goodrich DE, Klingaman EA, Verchinina L, Goldberg RW, Littman AJ, Janney CA, et al. Sex differences in weight loss among veterans with serious mental illness: observational study of a national weight management program. Womens Health Issues. 2016;26(4):410–9. https://doi.org/10.1016/j.whi.2016.05.001.
Maguen S, Hoerster KD, Littman AJ, Klingaman EA, Evans-Hudnall G, Holleman R, et al. Iraq and Afghanistan veterans with PTSD participate less in VA’s weight loss program than those without PTSD. J Affect Disord. 2016;193:289–94. https://doi.org/10.1016/j.jad.2015.12.078.
Muralidharan A, Klingaman EA, Prior SJ, Molinari V, Goldberg RW. Medical and psychosocial barriers to weight management in older veterans with and without serious mental illness. Psychol Serv. 2016;13(4):419–27. https://doi.org/10.1037/ser0000088.
Janney CA, Masheb RM, Lutes LD, Holleman RG, Kim HM, Gillon LR, et al. Mental health and behavioral weight loss: 24-month outcomes in veterans. J Affect Disord. 2017;215:197–204. https://doi.org/10.1016/j.jad.2017.03.003.
McKinnon CR, Garvin JT. Weight reduction goal achievement among veterans with mental health diagnoses. J Am Psychiatr Nurses Assoc. 2019;25(4):257–65. https://doi.org/10.1177/1078390318800594.
Littman AJ, Damschroder LJ, Verchinina L, Lai Z, Kim HM, Hoerster KD, et al. National evaluation of obesity screening and treatment among veterans with and without mental health disorders. Gen Hosp Psychiatry. 2015;37(1):7–13. https://doi.org/10.1016/j.genhosppsych.2014.11.005.
Higgins DM, Buta E, Dorflinger L, Masheb RM, Ruser CB, Goulet JL, et al. Prevalence and correlates of painful conditions and multimorbidity in national sample of overweight/obese veterans. J Rehabil Res Dev. 2016;53(1):71–82. https://doi.org/10.1682/JRRD.2014.10.0251.
Masheb RM, Lutes LD, Kim HM, Holleman RG, Goodrich DE, Janney CA, et al. Weight loss outcomes in patients with pain. Obesity (Silver Spring). 2015;23(9):1778–84. https://doi.org/10.1002/oby.21160.
Kubat E, Giori NJ, Hwa K, Eisenberg D. Osteoarthritis in veterans undergoing bariatric surgery is associated with decreased excess weight loss: 5-year outcomes. Surg Obes Relat Dis. 2016;12(7):1426–30. https://doi.org/10.1016/j.soard.2016.02.012.
Haibach JP, Haibach MA, Hall KS, Masheb RM, Little MA, Shepardson RL, et al. Military and veteran health behavior research and practice: challenges and opportunities. J Behav Med. 2017;40(1):175–93. https://doi.org/10.1007/s10865-016-9794-y.
Nightingale BA, Cassin SE. Disordered eating among individuals with excess weight: a review of recent research. Curr Obes Rep. 2019;8(2):112–27. https://doi.org/10.1007/s13679-019-00333-5.
Dorflinger LM, Masheb RM. PTSD is associated with emotional eating among veterans seeking treatment for overweight/obesity. Eat Behav. 2018;31:8–11. https://doi.org/10.1016/j.eatbeh.2018.07.005.
Dorflinger LM, Ruser CB, Masheb RM. Night eating among veterans with obesity. Appetite. 2017;117:330–4. https://doi.org/10.1016/j.appet.2017.07.011.
Peneau S, Menard E, Mejean C, Bellisle F, Hercberg S. Sex and dieting modify the association between emotional eating and weight status. Am J Clin Nutr. 2013;97(6):1307–13. https://doi.org/10.3945/ajcn.112.054916.
Gallant AR, Lundgren J, Drapeau V. The night-eating syndrome and obesity. Obes Rev. 2012;13(6):528–36. https://doi.org/10.1111/j.1467-789X.2011.00975.x.
Frayn M, Knäuper B. Emotional eating and weight in adults: a review. Curr Psychol. 2017;37(4):924–33. https://doi.org/10.1007/s12144-017-9577-9.
Stunkard AJ, Allison KC. Two forms of disordered eating in obesity: binge eating and night eating. Int J Obes Relat Metab Disord. 2003;27(1):1–12. https://doi.org/10.1038/sj.ijo.0802186.
Dochat C, Godfrey KM, Golshan S, Cuneo JG, Afari N. Dietary restraint and weight loss in relation to disinhibited eating in obese veterans following a behavioral weight loss intervention. Appetite. 2019;140:98–104. https://doi.org/10.1016/j.appet.2019.05.013.
Masheb RM, Lutes LD, Kim HM, Holleman RG, Goodrich DE, Janney CA, et al. High-frequency binge eating predicts weight gain among veterans receiving behavioral weight loss treatments. Obesity (Silver Spring). 2015;23(1):54–61. https://doi.org/10.1002/oby.20931.
Stanton MV, Matsuura J, Fairchild JK, Lohnberg JA, Bayley PJ. Mindfulness as a weight loss treatment for veterans. Front Nutr. 2016;3:30. https://doi.org/10.3389/fnut.2016.00030.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kristy Cuthbert has no conflicts of interest to report.
Sabrina Hardin has no conflicts of interest to report.
Rachel Zelkowitz has no conflicts of interest to report.
Karen Mitchell has no conflicts of interest to report.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Disclaimer
The contents of this article do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Psychological Issues
Rights and permissions
About this article
Cite this article
Cuthbert, K., Hardin, S., Zelkowitz, R. et al. Eating Disorders and Overweight/Obesity in Veterans: Prevalence, Risk Factors, and Treatment Considerations. Curr Obes Rep 9, 98–108 (2020). https://doi.org/10.1007/s13679-020-00374-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-020-00374-1