Abstract
Objective
To evaluate the association between the incidence of renal scarring on technetium-99 m dimercaptosuccinic acid (DMSA) renal scintigraphy and the severity of renal parenchymal infections, such as acute pyelonephritis (APN), acute focal bacterial nephritis (AFBN), and renal abscess, based on computed tomography (CT) diagnosis.
Methods
Sixty-one children with renal parenchymal infections were included and classified into two groups: those with (renal scarring group) and without renal scarring (non-renal scarring group) on chronic-phase DMSA renal scintigraphy. The severity of renal parenchymal infection was classified into three grades using CT: APN, AFBN, and renal abscess as grades 1, 2, and 3, respectively. The severity of renal parenchymal infection, vesicoureteral reflux (VUR) grade, and intrarenal reflux occurrence during voiding cystourethrography (VCUG) were evaluated between the renal and non-renal scarring groups. Fisher’s exact test and Mann–Whitney U test were used for statistical analysis.
Results
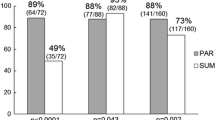
Renal scars were detected in 28 (45.9%) of the 61 patients. We found that 2/9 (22.2%), 18/41 (43.9%), and 8/11 (72.7%) patients with APN (grade 1), AFBN (grade 2), and renal abscess (grade 3) had renal scarring, respectively. There was a significant difference in the grade of severity of renal parenchymal infection between the renal (median = 2 [interquartile range, 2–3]) and non-renal (median = 2 [interquartile range, 2–2]) scarring groups (p = 0.023). There was a significant difference in the grade of VUR between the renal (median = 3 [interquartile range, 0–4]) and non-renal (median = 0 [interquartile range, 0–2]) scarring groups (p = 0.004). No significant difference in intrarenal reflux occurrence was observed between the renal (present/absent: 3/25) and non-renal (present/absent: 0/29) scarring groups (p = 0.112).
Conclusion
Our results showed that pediatric patients with renal scarring on chronic-phase DMSA renal scintigraphy tended to have a more severe renal infection.







Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Newman TB. The new American academy of Pediatrics urinary tract infection guideline. Pediatrics. 2011;128:572–5.
Wan J, Skoog SJ, Hulbert WC, et al. Section on urology response to new guidelines for the diagnosis and management of UTI. Pediatrics. 2012;129:e1051–3.
Baumer JH, Jones RW. Urinary tract infection in children, national institute for health and clinical excellence. Arch Dis Child Educ Pract Ed. 2007;92:189–92.
Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128:595–610.
Yang SS, Tsai JD, Kanematsu A, Han CH. Asian guidelines for urinary tract infection in children. J Infect Chemother. 2021;27:1543–54.
Hellerstein S. The long-term consequences of urinary tract infections: a historic and contemporary perspective. Pediatr Ann. 1999;28:695–9.
Roupakias S, Sinopidis X, Karatza A, Varvarigou A. Predictive risk factors in childhood urinary tract infection, vesicoureteral reflux, and renal scarring management. Clin Pediatr (Phila). 2014;53:1119–33.
Jacobson SH, Hansson S, Jakobsson B. Vesico-ureteric reflux: occurrence and long-term risks. Acta Paediatr Suppl. 1999;88:22–30.
Jakobsson B, Jacobson SH, Hjalmås K. Vesico-ureteric reflux and other risk factors for renal damage: identification of high- and low-risk children. Acta Paediatr Suppl. 1999;88:31–9.
Zaki, M., M. Badawi, G. Al Mutari, D. Ramadan, and M. Adul Rahman, (2005) Acute pyelonephritis and renal scarring in Kuwaiti children: a follow-up study using 99mTc DMSA renal scintigraphy. Pediatr Nephrol 20 1116–9.
Bar-Sever Z, Shammas A, Gheisari F, Vali R. Pediatric Nephro-urology: overview and updates in diuretic renal scans and renal cortical scintigraphy. Semin Nucl Med. 2022;52:419–31.
Shaikh N, Shope TR, Hoberman A, et al. Corticosteroids to prevent kidney scarring in children with a febrile urinary tract infection: a randomized trial. Pediatr Nephrol. 2020;35:2113–20.
Comploj E, Cassar W, Farina A, et al. Conservative management of paediatric renal abscess. J Pediatr Urol. 2013;9:1214–7.
Seidel T, Kuwertz-Broking E, Kaczmarek S, et al. Acute focal bacterial nephritis in 25 children. Pediatr Nephrol. 2007;22:1897–901.
Cheng CH, Tsau YK, Lin TY. Effective duration of antimicrobial therapy for the treatment of acute lobar nephronia. Pediatrics. 2006;117:e84–9.
Linder BJ, Granberg CF. Pediatric renal abscesses: a contemporary series. J Pediatr Urol. 2016;12:99.e1-5.
Soulen MC, Fishman EK, Goldman SM, Gatewood OM. Bacterial renal infection: role of CT. Radiology. 1989;171:703–7.
Cheng CH, Tsau YK, Lin TY. Is acute lobar nephronia the midpoint in the spectrum of upper urinary tract infections between acute pyelonephritis and renal abscess? J Pediatr. 2010;156:82–6.
Bitsori M, Raissaki M, Maraki S, Galanakis E. Acute focal bacterial nephritis, pyonephrosis and renal abscess in children. Pediatr Nephrol. 2015;30:1987–93.
He, Y., W. Zhang, N. Sun, et al. (2019) Experience of pediatric urogenital tract inserted objects: 10-year single-center study. J Pediatr Urol 554.e1-.e8
Rosenfield AT, Glickman MG, Taylor KJ, Crade M, Hodson J. Acute focal bacterial nephritis (acute lobar nephronia). Radiology. 1979;132:553–61.
Cheng CH, Tsau YK, Hsu SY, Lee TL. Effective ultrasonographic predictor for the diagnosis of acute lobar nephronia. Pediatr Infect Dis J. 2004;23:11–4.
Hosokawa, T., Y. Tanami, Y. Sato, et al., (2022) Role of ultrasound in the treatment of pediatric infectious diseases: case series and narrative review. World J Pediatr 1–15
Stunell H, Buckley O, Feeney J, et al. Imaging of acute pyelonephritis in the adult. Eur Radiol. 2007;17:1820–8.
Craig, W.D., B.J. Wagner, and M.D. Travis, (2008) Pyelonephritis: radiologic-pathologic review. Radiographics. 28 255–77, quiz 327–8
Mizutani M, Hasegawa S, Matsushige T, et al. Distinctive inflammatory profile between acute focal bacterial nephritis and acute pyelonephritis in children. Cytokine. 2017;99:24–9.
Fontanilla T, Minaya J, Cortes C, et al. Acute complicated pyelonephritis: contrast-enhanced ultrasound. Abdom Imaging. 2012;37:639–46.
Ergun R, Sekerci CA, Tanidir Y, et al. Abnormal DMSA renal scan findings and associated factors in older children with vesicoureteral reflux. Int Urol Nephrol. 2021;53:1963–8.
Muniz G, Charron M, Lim R, et al. The role of renal contour change in the diagnosis of cortical scarring after urinary tract infection. Am J Nucl Med Mol Imaging. 2022;12:41–3.
Koizumi K, Masaki H, Matsuda H, et al. Japanese consensus guidelines for pediatric nuclear medicine. Part 1: Pediatric radiopharmaceutical administered doses (JSNM pediatric dosage card). Part 2: Technical considerations for pediatric nuclear medicine imaging procedures. Ann Nucl Med. 2014;28:498–503.
Uchiyama, M. , M. Kitamura, (2020) Japanese consensus guidelines for pediatric nuclear medicine. The Japanese society of nuclear medicine 1–87
Fernbach, S.K., K.A. Feinstein, and M.B. Schmidt, (2000) Pediatric voiding cystourethrography: a pictorial guide. Radiographics 20 155–68 discussion 68–71
Läckgren G, Cooper CS, Neveus T, Kirsch AJ. Management of vesicoureteral reflux: what have we learned over the last 20 years? Front Pediatr. 2021;9: 650326.
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. international reflux study in children. Pediatr Radiol. 1985;15:105–9.
Rolleston GL, Maling TM, Hodson CJ. Intrarenal reflux and the scarred kidney. Arch Dis Child. 1974;49:531–9.
Hannerz L, Wikstad I, Johansson L, Broberger O, Aperia A. Distribution of renal scars and intrarenal reflux in children with a past history of urinary tract infection. Acta Radiol. 1987;28:443–6.
Morello W, La Scola C, Alberici I, Montini G. Acute pyelonephritis in children. Pediatr Nephrol. 2016;31:1253–65.
Rathore MH, Barton LL, Luisiri A. Acute lobar nephronia: a review. Pediatrics. 1991;87:728–34.
Klar A, Hurvitz H, Berkun Y, et al. Focal bacterial nephritis (lobar nephronia) in children. J Pediatr. 1996;128:850–3.
Majd M, Nussbaum Blask AR, Markle BM, et al. Acute pyelonephritis: comparison of diagnosis with 99mTc-DMSA, SPECT, spiral CT, MR imaging, and power doppler US in an experimental pig model. Radiology. 2001;218:101–8.
Kajiwara, K., S. Yamano, K. Aoki, et al., (2021) CDCP1 promotes compensatory renal growth by integrating Src and Met signaling. Life Sci Alliance 4
Liu T, Dai C, Xu J, Li S, Chen JK. The expression level of class III phosphatidylinositol-3 kinase controls the degree of compensatory nephron hypertrophy. Am J Physiol Renal Physiol. 2020;318:F628–38.
Bridges CC, Barfuss DW, Joshee L, Zalups RK. Compensatory renal hypertrophy and the uptake of cysteine s-conjugates of Hg2+ in Isolated S2 proximal tubular segments. Toxicol Sci. 2016;154:278–88.
Kim JH, Kim MJ, Lim SH, Kim J, Lee MJ. Length and volume of morphologically normal kidneys in korean children: ultrasound measurement and estimation using body size. Korean J Radiol. 2013;14:677–82.
Shimizu M, Katayama K, Kato E, et al. Evolution of acute focal bacterial nephritis into a renal abscess. Pediatr Nephrol. 2005;20:93–5.
Hosokawa T, Tanami Y, Sato Y, Oguma E. Comparison of imaging findings between acute focal bacterial nephritis (acute lobar nephronia) and acute pyelonephritis: a preliminary evaluation of the sufficiency of ultrasound for the diagnosis of acute focal bacterial nephritis. Emerg Radiol. 2020;27:405–12.
Acknowledgements
We would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for the English language
Funding
No.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no financial or personal relationships that could lead to a conflict of interest.
Ethical approval
This research was conducted in accordance with the tenets of the Declaration of Helsinki.
Informed consent
This retrospective study was approved by the ethics committee of our institution, and the requirement for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hosokawa, T., Uchiyama, M., Tanami, Y. et al. Incidence of renal scarring on technetium-99 m dimercaptosuccinic acid renal scintigraphy after acute pyelonephritis, acute focal bacterial nephritis, and renal abscess. Ann Nucl Med 37, 176–188 (2023). https://doi.org/10.1007/s12149-022-01814-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-022-01814-9