Abstract
Objective
The recommended durations of treatment for acute focal bacterial nephritis (AFBN) and acute pyelonephritis (APN) are different. This study aimed to clarify the sonographic findings used to differentiate AFBN from APN during diagnosis and to compare these findings with those obtained using computed tomography (CT).
Methods
Eleven children with urinary tract infection who underwent contrast-enhanced CT and ultrasound examinations within a 24-h period were included. Diagnoses of AFBN and APN were established using CT data as the gold standard; viz., a focal area of poor enhancement is observed in AFBN but not in APN. The following ultrasound findings were evaluated: focal loss of corticomedullary differentiation (one/multiple), focal hyperechogenicity, abscess formation, and diffuse nephromegaly. Fisher’s exact test was used for statistical analysis.
Results
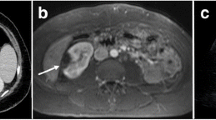
Of the 11 patients, 8 had AFBN and 3 had APN. The two groups differed significantly in the incidence of a focal loss of corticomedullary differentiation (present/absent, 8/8 vs. 0/3; p = 0.01) but not in the incidence of focal hyperechogenicity, abscess formation, and diffuse nephromegaly (present/absent, 2/8 vs. 0/3, p > 0.99; 1/8 vs. 0/3, p > 0.99; and 5/8 vs. 3/3, p = 0.49, respectively). The poorly enhanced area used to diagnose AFBN on CT images appeared as a focal loss of corticomedullary differentiation in ultrasound examinations. CT revealed multiple lesions in two cases in which ultrasound revealed only single lesions.
Conclusion
In our small cohort, ultrasound could be adequately used to diagnose AFBN based on the presence of a focal loss of corticomedullary differentiation. CT may not be required to differentiate AFBN from APN.




Similar content being viewed by others
References
Bitsori M, Raissaki M, Maraki S, Galanakis E (2015) Acute focal bacterial nephritis, pyonephrosis and renal abscess in children. Pediatr Nephrol 30(11):1987–1993. https://doi.org/10.1007/s00467-015-3141-3
Rosenfield AT, Glickman MG, Taylor KJ, Crade M, Hodson J (1979) Acute focal bacterial nephritis (acute lobar nephronia). Radiology 132(3):553–561. https://doi.org/10.1148/132.3.553
Cheng CH, Tsau YK, Lin TY (2006) Effective duration of antimicrobial therapy for the treatment of acute lobar nephronia. Pediatrics 117(1):e84–e89. https://doi.org/10.1542/peds.2005-0917
Morello W, La Scola C, Alberici I, Montini G (2016) Acute pyelonephritis in children. Pediatr Nephrol 31(8):1253–1265. https://doi.org/10.1007/s00467-015-3168-5
Rathore MH, Barton LL, Luisiri A (1991) Acute lobar nephronia: a review. Pediatrics 87(5):728–734
Klar A, Hurvitz H, Berkun Y, Nadjari M, Blinder G, Israeli T, Halamish A, Katz A, Shazberg G, Branski D (1996) Focal bacterial nephritis (lobar nephronia) in children. J Pediatr 128(6):850–853. https://doi.org/10.1016/s0022-3476(96)70340-2
Kline MW, Kaplan SL, Baker CJ (1988) Acute focal bacterial nephritis: diverse clinical presentations in pediatric patients. Pediatr Infect Dis J 7(5):346–349. https://doi.org/10.1097/00006454-198805000-00012
Cheng CH, Tsau YK, Lin TY (2010) Is acute lobar nephronia the midpoint in the spectrum of upper urinary tract infections between acute pyelonephritis and renal abscess? J Pediatr 156(1):82–86. https://doi.org/10.1016/j.jpeds.2009.07.010
Cheng CH, Tsau YK, Hsu SY, Lee TL (2004) Effective ultrasonographic predictor for the diagnosis of acute lobar nephronia. Pediatr Infect Dis J 23(1):11–14. https://doi.org/10.1097/01.inf.0000105202.57991.3e
Dacher JN, Pfister C, Monroc M, Eurin D, LeDosseur P (1996) Power Doppler sonographic pattern of acute pyelonephritis in children: comparison with CT. AJR Am J Roentgenol 166(6):1451–1455. https://doi.org/10.2214/ajr.166.6.8633462
Stunell H, Buckley O, Feeney J, Geoghegan T, Browne RF, Torreggiani WC (2007) Imaging of acute pyelonephritis in the adult. Eur Radiol 17(7):1820–1828. https://doi.org/10.1007/s00330-006-0366-3
Craig WD, Wagner BJ, Travis MD (2008) Pyelonephritis: radiologic-pathologic review. Radiographics 28(1):255–277; quiz 327-258. https://doi.org/10.1148/rg.281075171
Hosokawa T, Yamada Y, Tanami Y, Sato Y, Ishimaru T, Tanaka Y, Kawashima H, Oguma E (2019) Comparison of diagnostic accuracy for fistulae at ultrasound and voiding cystourethrogram in neonates with anorectal malformation. Pediatr Radiol 49(5):609–616. https://doi.org/10.1007/s00247-018-04339-4
Lavocat MP, Granjon D, Allard D, Gay C, Freycon MT, Dubois F (1997) Imaging of pyelonephritis. Pediatr Radiol 27(2):159–165. https://doi.org/10.1007/s002470050091
Mizutani M, Hasegawa S, Matsushige T, Ohta N, Kittaka S, Hoshide M, Kusuda T, Takahashi K, Ichihara K, Ohga S (2017) Distinctive inflammatory profile between acute focal bacterial nephritis and acute pyelonephritis in children. Cytokine 99:24–29. https://doi.org/10.1016/j.cyto.2017.06.012
Farmer KD, Gellett LR, Dubbins PA (2002) The sonographic appearance of acute focal pyelonephritis 8 years experience. Clin Radiol 57(6):483–487. https://doi.org/10.1053/crad.2002.0935
Soulen MC, Fishman EK, Goldman SM, Gatewood OM (1989) Bacterial renal infection: role of CT. Radiology 171(3):703–707. https://doi.org/10.1148/radiology.171.3.2655002
Kim JH, Kim MJ, Lim SH, Kim J, Lee MJ (2013) Length and volume of morphologically normal kidneys in Korean children: ultrasound measurement and estimation using body size. Korean J Radiol 14(4):677–682. https://doi.org/10.3348/kjr.2013.14.4.677
Hosokawa T, Yamada Y, Tanami Y, Sato Y, Ko Y, Nomura K, Oguma E (2020) Computed tomography findings of mediastinitis after cardiovascular surgery. Pediatr Int 62(2):206–213. https://doi.org/10.1111/ped.14101
Shimizu M, Katayama K, Kato E, Miyayama S, Sugata T, Ohta K (2005) Evolution of acute focal bacterial nephritis into a renal abscess. Pediatr Nephrol 20(1):93–95. https://doi.org/10.1007/s00467-004-1646-2
Hosokawa T, Suzuki S, Tanami Y, Sato Y, Ko Y, Nomura K, Hosokawa M, Oguma E, Yamada Y (2019) Ultrasound evaluation of complications after cardiovascular surgery in pediatric patients: a case series. Med Ultrason Epub ahead of print. Doi:https://doi.org/10.11152/mu-1982
Hosokawa T, Yamada Y, Tanami Y, Sato Y, Ishimaru T, Kawashima H, Oguma E (2019) Associations between sonographic findings and operative time of transumbilical laparoscopic-assisted appendectomy for acute appendicitis in children. AJR Am J Roentgenol:1–9. doi:https://doi.org/10.2214/ajr.18.20937
Saunders HS, Dyer RB, Shifrin RY, Scharling ES, Bechtold RE, Zagoria RJ (1995) The CT nephrogram: implications for evaluation of urinary tract disease. Radiographics 15(5):1069–1085; discussion 1086-1068. https://doi.org/10.1148/radiographics.15.5.7501851
He Y, Zhang W, Sun N, Feng G, Ni X, Song H (2019) Experience of pediatric urogenital tract inserted objects: 10-year single-center study. J Pediatr Urol 15(5):554.e551–554.e558. https://doi.org/10.1016/j.jpurol.2019.05.038
Albracht CD, Hreha TN, Hunstad DA (2020) Sex effects in pyelonephritis. Pediatr Nephrol:1–9. https://doi.org/10.1007/s00467-020-04492-9
Seitz K, Bernatik T, Strobel D, Blank W, Friedrich-Rust M, Strunk H, Greis C, Kratzer W, Schuler A (2010) Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM multicenter trial): CEUS vs. MRI--a prospective comparison in 269 patients. Ultraschall Med 31(5):492–499. https://doi.org/10.1055/s-0029-1245591
Fontanilla T, Minaya J, Cortes C, Hernando CG, Aranguena RP, Arriaga J, Carmona MS, Alcolado A (2012) Acute complicated pyelonephritis: contrast-enhanced ultrasound. Abdom Imaging 37(4):639–646. https://doi.org/10.1007/s00261-011-9781-2
Hashimoto M, Ohkuma K, Akita H, Yamada Y, Nakatsuka S, Mizuno R, Oya M, Jinzaki M (2019) Usefulness of contrast-enhanced ultrasonography for diagnosis of renal cell carcinoma in dialysis patients: comparison with computed tomography. Medicine (Baltimore) 98(47):e18053. https://doi.org/10.1097/md.0000000000018053
Author information
Authors and Affiliations
Contributions
T.H. and Y.T designed the study; Y.T and Y.S collected and analyzed data; T.H and Y.T
wrote the manuscript; T.H and Y.T performed the statistical analysis and drafted the manuscript; and E.O critically reviewed the manuscript and supervised the whole study process.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human subjects
This research was performed in accordance with the tenets of the Declaration of Helsinki.
Informed consent
This retrospective study was approved by the ethics committee of our institution, and informed consent was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hosokawa, T., Tanami, Y., Sato, Y. et al. Comparison of imaging findings between acute focal bacterial nephritis (acute lobar nephronia) and acute pyelonephritis: a preliminary evaluation of the sufficiency of ultrasound for the diagnosis of acute focal bacterial nephritis. Emerg Radiol 27, 405–412 (2020). https://doi.org/10.1007/s10140-020-01771-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-020-01771-8