Abstract
The challenges of parental cancer while caring for young offspring are often neglected by researchers and healthcare providers. Focusing on parents with cancer, this cross-sectional study examines the mediating and moderating roles of a malleable risk factor, psychological inflexibility, in the relationships between perceived illness severity and parental quality of life (QoL) and family outcomes. Psychological inflexibility was conceptualized using the acceptance and commitment therapy (ACT) framework. A total of 86 parents with cancer caring for young offspring (aged 11–24 years; M = 17.94, SD = 3.68) completed a survey that assessed psychological inflexibility, parental mental and physical health QoL, family outcomes (family functioning, parenting concerns, and openness to discuss cancer), socio-demographics, and illness variables. Mediation analyses indicated that higher perceived illness severity was associated with higher levels of psychological inflexibility, which in turn were related to higher detrimental impacts on parental QoL and family outcomes. Results of moderation analyses were non-significant. Findings highlight the detrimental impacts of illness severity on psychological inflexibility, suggesting that it is a psychosocial risk factor in parents dealing with cancer. ACT-based interventions which foster psychological flexibility are likely to enhance parental QoL and family outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is a serious public health problem and the second leading cause of mortality globally (World Health Organization, 2022). Cancer caused 9.96 million deaths in 2020, and projections indicate a substantial rise, with an estimated 27.0 million cases expected by 2040. Despite the rise in the five-year survival rate to over 60% thanks to advancements in detection and treatments (Sung et al., 2021), the cancer journey entails a complex web of challenges that extend beyond physical health. Cancer patients often grapple with diverse cancer-related demands, including coping with treatment side effects, adapting to functional loss, and confronting existential fears related to mortality. These adjustment hurdles often elicit profound psychological distress which is associated with reduced quality of life (QoL) (Abdelhadi, 2023). While anxiety and depression are the most frequently reported psychological symptoms, many cancer patients also experience elevated health anxiety, cancer-related post-traumatic stress, and sleep disturbances, all of which disrupt daily living (Hong et al., 2020). Pain, a prevalent cancer symptom, further compounds distress and diminishes QoL (Abdelhadi, 2023). Additionally, the unpredictable trajectory of the illness, from diagnosis to long-term survivorship, presents a substantial challenge that can hinder psychological adjustment (Guan et al., 2021).
Cancer also has a profound impact on parenting and family functioning. A systematic review conducted in Western countries estimated that a considerable proportion (14–25%) of individuals with cancer have offspring up to age 25 years (Inhestern et al., 2021). Notably, the age range 11–24 was identified by a Lancet commission as a key focus area for youth health and well-being studies (Patton et al., 2016). This age range has also been commonly examined in research exploring the effects of parental illnesses, including cancer, on young offspring (e.g., Landi et al., 2020; Morris et al., 2018; Walczak et al., 2018). It encompasses key developmental phases involving transition from adolescence to young adulthood. During these transformative years, young individuals are shaping their identities, asserting independence, and navigating toward higher education or employment (Patton et al., 2016). The presence of a severe parental illness, such as cancer, can significantly amplify the challenges faced during these life transitions. Parents with cancer must navigate the multifaceted demands of managing their illness while parenting. They confront the delicate task of addressing cancer-related concerns within the family and ensuring the well-being of their maturing children (Johannsen et al., 2022; Newman et al., 2023).
A diagnosis of cancer in the context of being responsible for parenting can magnify fears of loss, jeopardize the family’s long-term outlook, and threaten the family’s sense of identity (Fugmann et al., 2023; Newman et al., 2023; Walczak et al., 2018). For offspring aged 11–24, witnessing a parent’s battle with cancer can heighten anxieties about their own health and future (Morris et al., 2018; Mota-George et al., 2023). Furthermore, cancer and its treatments reshape everyday roles within the family. These changes can lead to family functioning problems such as increased family conflicts, less cohesion, and limited communication about cancer, further complicating the developmental challenges faced by offspring in this age range (Kuswanto et al., 2018; Landi et al., 2022a; Pedersen & Revenson, 2005).
The assessment of parenting worries among cancer patients was the focus of a questionnaire developed by Muriel and colleagues. Their research identified parenting concerns as a potential independent factor contributing to the psychological strain associated with cancer (Muriel et al., 2012). In a study observing parents with cancer six years post-diagnosis, higher parenting concerns– ranging from practical to emotional impacts on young offspring and concerns about the co-parent/partner– were associated with higher emotional distress and diminished parenting confidence (Inhestern et al., 2016). As these young offspring navigate developmental milestones, the repercussions of a parent’s cancer diagnosis may further adversely affect their well-being. Yet, there is a paucity of research examining how potentially modifiable risk factors affect the psychological adjustment and QoL of parents with cancer and their families.
One such risk factor is psychological inflexibility (PI), which encapsulates a person’s unwillingness to connect to ongoing unwanted inner states, such as unpleasant thoughts, emotions, and memories. This experiential avoidance leads to an overreliance on automatic and rigid psychological responses which can derail the pursuit of personal values (Hayes et al., 2012). The acceptance and commitment therapy (ACT) framework posits PI as a transdiagnostic factor that plays a role in the onset and maintenance of various mental health problems (Levin et al., 2014). The goal of ACT is to cultivate psychological flexibility (PF), the capacity to effectively manage these challenging internal states while adapting actions to meet the demands of the current context, thereby ensuring alignment with one’s core values (Hayes et al., 2012). Essentially, PF fosters a range of behavioral responses that enhance adjustment to evolving situations and is therefore considered a fundamental aspect of mental health (Stockton et al., 2019).
In the context of cancer, studies suggest that elevated PI is associated with higher psychological distress and lower QoL (Gillanders et al., 2015; Hulbert-Williams & Storey, 2016; Novakov, 2021). Systematic reviews have noted the potential of ACT interventions in enhancing mental health and QoL for individuals with cancer and other chronic illnesses (Li et al., 2021; Salari et al., 2023; Zhao et al., 2021). Consistent with the PF framework underpinning ACT, one systematic review found evidence to support PF as the therapeutic mechanism responsible for intervention effects on QoL and other outcomes (Stockton et al., 2019). While no specific published studies to date have explored the impact of PI on parents with cancer, in the broader literature parental PI is associated with heightened parental stress, reduced emotional availability, less compassionate family interactions, and lower well-being for both parents and their young offspring (Caldas et al., 2023; Daks & Rogge, 2020). Furthermore, families with parents who report high PI often evidence family conflict, communication problems, and reduced cohesion (Daks & Rogge, 2020). Consequently, when a parent with cancer, particularly one with young offspring, shows high levels of PI, family functioning and QoL can be significantly compromised.
Evidence indicates that PI can function as both a mediator and moderator in the relationship between a stressor and psychosocial outcomes. Study findings that have supported the mediational role of PI have clarified the pathway through which a stressor impacts PI and subsequently influences psychological distress (see for example, Fischer et al., 2016). Conversely, research findings that have highlighted the moderation role of PI, show how it affects the intensity or direction of the relationship between stressor and psychosocial outcome (see for example, Landi et al., 2021; Pakenham et al., 2020). However, no published research has examined either the moderating or mediating PI roles in the links between perceived illness severity and QoL and family functioning outcomes in the context of parental cancer. In the cancer and chronic illness fields, the literature has typically focused on individuals who have serious health problems without considering parenting status (Novakov, 2021; Özönder Ünal et al., 2023; Probst et al., 2018). Overall, the aforementioned studies support the notion that PI can both mediate and moderate the impact of stressors and psychosocial outcomes in the context of a serious medical condition. Hence, in the present study we investigate both the mediating and moderating roles of PI in the link between perceived illness severity QoL and family outcomes in parents with cancer.
The Present Study
The investigation of PI as a modifiable risk factor that detrimentally affects parental QoL and family outcomes could inform the development of support services tailored to parents dealing with cancer while also caring for young offspring. Therefore, the purpose of this study is to investigate the role of PI in linking perceived illness severity to physical and mental QoL and family outcomes (including family functioning, parenting concerns, and openness to discuss cancer) in parents with cancer. In the absence of clear theoretical and empirical evidence favoring either the mediating or moderating roles of PI in this context, this study examines both mechanisms. Two hypotheses are proposed:
-
1.
Hypothesis 1 (Mediation) proposes that PI mediates the adverse effects of illness severity on parental QoL and family outcomes. Specifically, we predict that greater perceived illness severity will be associated with higher PI, which, in turn, will be related to greater negative impacts of illness severity on parental QoL and family outcomes.
-
2.
Hypothesis 2 (Moderation) proposes that the effect of perceived illness severity on parental QoL and family outcomes varies as a function of variations in levels of PI. Specifically, we predict that higher PI will exacerbate the detrimental effects of illness severity on parental QoL and family outcomes for those with increasing levels of illness severity.
Materials and methods
Participants and recruitment procedure
The study involved 86 Italian parents with cancer who had adolescent and young adult offspring (aged 11–24 years; M = 17.94, SD = 3.68; range = 11.63–23.95). The inclusion criteria required participants to have a diagnosis of cancer for at least 6 months and children aged between 11 and 24. An exclusion criterion for the study was the presence of a severe medical condition in any other family member. The study was advertised as “The Promotion of Mental Health and Well-being in Parents with Cancer” and was publicized through various channels via a convenience sampling method. Recruitment strategies included the dissemination of informational brochures and posters in local community cancer organizations (i.e., AIMaC - Italian Association of Cancer Patients, Relatives and Friends, AIRC Foundation for the research on cancer, etc.), health facility waiting rooms (i.e., general practitioners, hospitals, and cancer specialist clinics), and via social media (i.e., online self-help and family support groups). Prospective participants initiated contact with the research team to enroll in the study. Surveys were distributed and collected in person, typically at a participant’s home, by a member of the research team. Due to the diverse recruitment methods, an overall response rate could not be calculated. The main reasons for nonparticipation were time constraints, emotional distress, and other health complications. The recruitment period was from November 2018 to May 2019. The study received clearance by the University of Bologna ethics committee.
Measures
Socio-demographics and illness-related variables
Parents provided information regarding their gender, age, marital status, level of education, employment status, socio-economic background, and nationality. Additionally, they detailed the number of individuals in their household, specifying how many children they had within the 11–24 age bracket. Parents also provided the name of their cancer diagnosis and the number of years since their diagnosis.
Illness severity
To assess perceptions of illness severity, we utilized scales established in prior research (e.g., Ireland & Pakenham, 2010; Landi et al., 2022b). Cancer severity: parents rated the seriousness of their cancer. Physical pain: parents rated the severity of their physical pain in the previous month. Both items were rated on a 5-point Likert scale (1 not at all serious to 5 very serious). Illness unpredictability: parents rated their agreement with five statements regarding the unpredictability of their illness on a 5-point Likert scale (1 strongly disagree to 5 strongly agree). The cancer severity, pain and illness unpredictability scores were significantly positively intercorrelated (range 0.27–0.30, p < 0.05; mean intercorrelation = 0.28). Hence, a Perceived Illness Parental Severity Index was formulated by averaging the three scores (range 1–5), where a higher index score indicated higher perceived illness severity. This Perceived Parental Illness Severity Index variable is labelled illness severity from here-on. Observed McDonald’s omega = 0.82.
PI
The Italian validated short-form of the 8-item Avoidance and Fusion Questionnaire for Youth (AFQ-Y8) (Greco et al., 2008) was employed to measure PI. The AFQ-Y8 has been shown to possess excellent psychometric properties in adult populations (Fergus et al., 2012) and among individuals with cancer (Cederberg et al., 2018). Items are rated on a 5-point Likert scale (0 not at all true to 4 very true). A total score is calculated by summing item ratings (range 0–32). Higher scores indicate greater levels of PI. Observed McDonald’s omega = 0.75.
QoL
The validated Italian version of the Short Form 12 (SF-12) questionnaire (Ware et al., 1996) was utilized to evaluate QoL. The SF-12 generates two composite scores reflecting physical and mental health QoL, derived from the weighted sum of relevant items, with scores ranging from 0 to 100. Higher composite scores indicate better QoL (Ware et al., 1996). The SF-12 is recognized for its robust validity and consistency (Ware et al., 1996). Observed McDonald’s omegas: physical health QoL = 0.94 and mental health QoL = 0.92.
Family functioning
The Italian version of the 12-item global family functioning subscale of the Family Assessment Device (FAD) (Epstein et al., 1983) was used to gauge family functioning. Subscale items are rated on a 5-point Likert scale (0 strongly agree to 4 strongly disagree). A mean subscale score is calculated. Higher scores reflect more effective family functioning (range 0–4). Reliability and validity of the FAD are well-established (Epstein et al., 1983). Observed McDonald’s omega = 0.91.
Parenting concerns
The 15-item Parenting Concerns Questionnaire (PCQ) (Muriel et al., 2012) measures the severity of concerns parents have about the practical and emotional repercussions of cancer on their young offspring, as well as worries related to the co-parent/partner. Respondents rated their concerns on a 5-point Likert scale (1 no concerns to 5 extremely concerned). A mean score is calculated. Higher scores indicate greater parenting concerns (range 1–5). The PCQ has demonstrated good psychometric properties (Muriel et al., 2012). Observed McDonald’s omega = 0.87. Footnote 1
Openness to discuss cancer in the family
The 8−item Openness to Discuss Cancer in the Family (ODCF) Scale measures how willing cancer patients are to talk about their illness with immediate family members (Mesters et al., 1997). Items are rated on a 5−point Likert scale (0 strongly agree to 4 strongly disagree). A mean score is calculated (range 0–4), which reflects the quality of cancer−related communication within the family. Higher scores denote more open communication. Observed McDonald’s omega = 0.84. Footnote 2
In summary, the focal study variables are illness severity (independent variable), PI (moderator or mediator), and the dependent variables parental QoL outcomes (physical and mental) and family outcomes (family functioning, parenting concerns, openness to discuss cancer). Socio-demographic and illness-related variables were assessed to gauge the broader context.
Data analysis approach
There was a very low level of missing data (0.29%). Mplus 8.3 was utilized to carry out mediation and moderation analyses using the maximum likelihood estimation (Muthén & Muthén, 1998–2018), while all other statistical analyses were conducted in SPSS 24. Correlations were used to examine relations among illness severity, PI, parental QoL outcomes (physical and mental), family outcomes (family functioning, parenting concerns, openness to discuss cancer) and potential confounding socio-demographic and illness-related variables. Socio-demographic and illness-related variables that were significantly correlated with one or more of the focal study variables were included as control variables in subsequent mediation and moderation analyses.
Mediational analyses were conducted to investigate the mediating role of PI in the relationship between illness severity and the dependent variables (i.e., physical and mental health QoL, family functioning, parenting concerns, and openness to discuss cancer). Indirect effects were determined by generating bias-corrected 95% confidence intervals (CIs) from 10,000 random bootstrap samples (Hayes & Scharkow, 2013), with statistical significance recognized when zero did not fall within these CIs. Moderation analyses were undertaken to determine the moderating effects of PI on the association between illness severity and both parental QoL and family outcomes (Hayes, 2017). These analyses investigated the illness severity X PI interaction effects on the dependent variables.
Results
Participant characteristics and correlations among study variables
Table 1 presents the sample characteristics, and Table 2 provides means, standard deviations, ranges, skewness, and kurtosis, as well as correlations among study variables. Illness severity was significantly positively associated with parenting concerns (r = 0.33, p < 0.01) and negatively associated with both physical health QoL (r = − 0.53, p < 0.001) and openness to discuss cancer (r = − 0.48, p < 0.001). These correlations between higher illness severity and poorer parental QoL and family outcomes support the validity of the Perceived Parental Illness Severity Index. PI was significantly correlated with all parental QoL and family outcomes, with most of the correlation coefficients being of a moderate magnitude and in the expected direction– that is, elevated PI was associated with worse parental QoL and family outcomes. Most of the parental QoL and family outcomes were significantly correlated with each other and in the expected direction.
To determine potential confounding socio-demographic and illness-related variables to be controlled for in the primary analyses, we examined the correlations between these variables and the study focal variables. We employed Pearson’s correlations for continuous variables and Spearman’s correlations for categorical variables. To address the large number of correlations performed, we applied a stricter significance threshold (p < 0.01). The only significant correlation was between parenting concerns and family size (r = − 0.43, p < 0.001), indicating that larger family size was associated with lower levels of parenting concerns. Consequently, in subsequent mediational and moderation analyses, we controlled for the effects of family size.
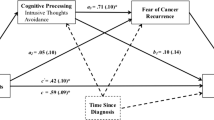
Mediation analyses
Table 3 presents standardized coefficients along with 95% confidence intervals, derived from 10,000 bootstraps, for each mediational model assessing parental QoL and family outcomes. The mediational models are diagrammatically presented in Fig. 1. In relation to parental QoL outcomes, the indirect effects reveal that PI serves as a significant mediator in the relationship between illness severity and both parental QoL outcomes: physical health QoL (standardized indirect effect ab = − 0.03, SE = 0.03, 95% CI [− 0.108, − 0.001]), and mental health QoL (standardized indirect effect ab = − 0.07, SE = 0.05, 95% CI [− 0.169, − 0.005]). Participants with higher illness severity exhibited higher levels of PI (a = 0.17, SE = 0.11) which, in turn, were associated with more pronounced adverse effects of illness severity on parental QoL outcomes (physical health QoL: b = − 0.19, SE = 0.10; mental health QoL: b = − 0.40, SE = 0.11). These models accounted for 19.4% and 32.3% of the variance in mental health and physical health QoL, respectively.
In relation to family outcomes, the indirect effects also indicated that PI plays a significant mediating role in the relationship between illness severity and all family outcomes: family functioning (standardized indirect effect ab = − 0.09, SE = 0.06, 95% CI [− 0.197, − 0.005]), parenting concerns (standardized indirect effect ab = 0.04, SE = 0.03, 95% CI [0.002, 0.102]), and openness to discuss cancer (standardized indirect effect ab = − 0.04, SE = 0.03, 95% CI [− 0.112, − 0.005]). Participants with higher illness severity exhibited elevated levels of PI (a = 0.17, SE = 0.11) which, in turn, were associated with more pronounced adverse effects of illness severity on family outcomes (family functioning: b = − 0.49, SE = 0.10; parenting concerns: b = 0.20, SE = 0.10; openness to discuss cancer: b = − 0.25, SE = 0.09). These models accounted for between 23.2% (family functioning) to 32.2% (parenting concerns) of the variance. In summary, across all models, higher levels of PI were linked to greater negative impacts of illness severity on all parental QoL and family outcomes.
Moderation analyses
Results from the moderation analyses indicated that the interaction between illness severity and PI had non-significant effects on all outcomes: parental QoL outcomes (physical health QoL: interaction standardized coefficient = 0.021, SE = 0.083, p = 0.797, 95% CI [− 0.116, 0.158]; mental health QoL: interaction standardized coefficient = − 0.034, SE = 0.091, p = 0.705, 95% CI [− 0.213, 0.115]) and family outcomes (family functioning: interaction standardized coefficient = − 0.008, SE = 0.089, p = 0.929, 95% CI [− 0.154, 0.138]; parenting concerns: interaction standardized coefficient = − 0.045, SE = 0.087, p = 0.437, 95% CI [− 0.113, 0.097]; openness to discuss cancer: interaction standardized coefficient = 0.043, SE = 0.022, p = 0.467, 95% CI [0.097, − 0.139]).
Discussion
In the context of parents with cancer caring for young offspring (aged 11–24 years), this study investigated the mediating and moderating roles of a malleable risk factor, parental PI, in the relationship between illness severity and parental QoL and family outcomes. Results supported the mediation model (Hypothesis 1), revealing that greater perceived illness severity was associated with higher levels of parental PI, which in turn exacerbated the adverse consequences of illness severity on parental QoL and family outcomes (including family functioning, parenting concerns, and openness to discuss cancer). This is the first published study demonstrating the mediating role of PI in the link between illness severity and QoL and family outcomes in parents with cancer. These findings align with those of prior research in the broader literature that have also demonstrated the mediating role of PI (Fischer et al., 2016; Özönder Ünal et al., 2023).
Results did not support the moderating role of PI in parents with cancer (hypothesis 2), indicating the relationship between illness severity and QoL and family outcomes did not vary as a function of different levels of PI. This is in contrast to the findings of studies that support the moderating role of PI in the link between a stressor and psychosocial outcomes in other health contexts (Landi et al., 2021; Pakenham et al., 2020; Probst et al., 2018). Whether PI operates via a mediating or moderating mechanism may depend on the health context given that PI and PF processes are context sensitive (Pakenham et al., 2023). Additionally, how PI functions to influence parental QoL and family functioning is likely to change over time in accord with evolving family developmental stages. Future research should explore the role of PI in the context of the long-term effects of parental cancer on QoL and family adjustment. This would provide valuable insights into whether the relative strength of mediating and moderating mechanisms change and how they shape psychosocial outcomes over time.
The results from this study align with prior research that has identified PI as a psychosocial risk factor among individuals with cancer by way of its association with lower physical and mental QoL (Gillanders et al., 2015; Hulbert-Williams & Storey, 2016; Novakov, 2021). However, present findings extend this pattern of results by demonstrating that the adverse effects of illness severity on QoL and family functioning occur via its association with PI in the context of parental cancer.
Regarding broader theoretical implications of these findings, our results provide support for the mediating role of PI in the link between stressor and psychosocial outcome. However, whether PI functions via a mediating or moderating mechanism may depend on context, as discussed above. Further theory driven research is required to investigate how the nature of relations among PI, stressors, and outcomes changes as a function of different contexts.
Reviews have demonstrated that ACT interventions promote mental health and QoL in individuals with cancer (Li et al., 2021; Salari et al., 2023; Zhao et al., 2021) and other chronic illnesses, and that these improvements occur via increases in PF (Stockton et al., 2019). In addition, preliminary findings from evaluations of ACT interventions that included parental therapeutic components show improvements in parenting skills and family functioning (Byrne et al., 2021). Moreover, when parents exhibit higher PF, they are likely to experience improved QoL, which can positively influence family dynamics and resilience (Daks & Rogge, 2020). Given this body of evidence and the present results showing that PI is a risk factor for parental cancer-related QoL and family functioning, ACT-based interventions are likely to enhance adjustment in the parent with cancer and positively impact family functioning. In view of evidence showing that ACT enhances interpersonal relations (Bernal-Manrique et al., 2020), it is likely that such interventions will also promote effective communication about cancer-related issues within the family (Hulbert-Williams et al., 2021). Additionally, evidence suggests that increased parental PF leads to more adaptive parenting practices, which in the cancer context may enable parents to better address the unique challenges faced by their young offspring related to living with a parent affected by cancer (Daks & Rogge, 2020). Hence, future research should implement and evaluate the integration of ACT informed services and interventions into healthcare settings that support parents with cancer.
Adults with cancer who parent young offspring constitute a vulnerable subgroup of cancer patients with specific needs that are often overlooked by researchers and healthcare providers (Fugmann et al., 2023; Johannsen et al., 2022; Newman et al., 2023). More attention should be placed on the unique challenges of parents coping with cancer while also fulfilling their parental responsibilities. However, there tends to be a shortfall in recognition among healthcare practitioners regarding the presence and impact of young offspring in the lives of patients undergoing cancer treatment (Kazlauskaite & Mendenhall, 2023). Limited psycho-oncological care resources also contribute to the tendency to neglect parenthood issues in standard clinical practice (Inhestern et al., 2021; Johannsen et al., 2022; Newman et al., 2023). This study brings to light the negative impacts that the severity of the illness can have on parental PI, affecting both the individual and family dynamics, and underscores the necessity for interventions that enhance PF to be incorporated during cancer care. For instance, healthcare practitioners could routinely use self-report measures to detect parents who are struggling to meet illness and parenting demands and then integrate parenting supports into the broader cancer treatment process (Fugmann et al., 2023; Inhestern et al., 2016, 2021; Johannsen et al., 2022). Parents identified as vulnerable could benefit from being offered ACT interventions to boost PF, either face-to-face or through digital platforms.
Study limitations and future research recommendations
Interpretation of study results should be tempered by the following methodological constraints. First, the generalizability of findings is limited due to non-random convenience sampling, which may increase volunteer response bias. In this regard, there was an overrepresentation of women and breast cancer in this study. Subsequent studies should explore how parental roles (comparing mothers to fathers) influence the dynamics between illness severity, PI, QoL, and family functioning. However, it should be noted that participants were recruited from a wide range of facilities using diverse recruitment strategies to maximize representativeness of the sample. Additionally, the use of a cross-sectional design means that it is not possible to ascertain cause-and-effect relationships among illness severity, parental PI, QoL, and family outcomes. Moreover, the relatively small sample size may increase the risk of Type II error (Fritz & MacKinnon, 2007; Sommet et al., 2023), potentially obscuring the detection of subtle effects among study variables. To enhance the statistical power and rigor of investigations into the role of PI in shaping adjustment to cancer in parents, future research should use a larger sample size. Lastly, this study measured PI without assessing PF. Future research should investigate the role of PF as a potential protective factor for parents dealing with cancer.
Conclusions
Individuals with cancer involved in parenting young offspring (aged 11–24 years) have specific challenges that are frequently overlooked by researchers and healthcare providers. Notwithstanding methodological weaknesses, findings from this study reveal the detrimental impacts of perceived illness severity on PI and, ultimately on parental QoL and family outcomes. These results can inform the creation of supports for parents with cancer and young offspring that enhance PF. Specifically, ACT-based interventions designed to boost PF and address the intricate dynamics of coping with cancer while parenting young offspring are likely to foster parental QoL and positive family functioning. Evaluation of such interventions in future research will advance psycho-oncological care, and shed more light on the moderating and mediating roles of PI in the links between illness severity and QoL and family outcomes in the parental cancer context.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Notes
1 Since the PCQ has not been validated in Italian, a Confirmatory Factor Analysis was conducted. Model fit was satisfactory for the original PCQ three-factor model: χ2 (87) = 573.642, p < 0.001; CFI = 0.924; TLI = 0.905; RMSEA = 0.070; RMSEA 90%; CI = 0.038, 0.078.
2 Because the ODCF has not been validated in Italian, a Confirmatory Factor Analysis was conducted. Model fit was satisfactory for the original ODCF one-factor model: χ2 (87) = 486.265, p < 0.001; CFI = 0.947; TLI = 0.915; RMSEA = 0.065; RMSEA 90%; CI = 0.023, 0.071.
References
Abdelhadi, O. (2023). The impact of psychological distress on quality of care and access to mental health services in cancer survivors. Frontiers in Health Services. https://doi.org/10.3389/frhs.2023.1111677.
Bernal-Manrique, K. N., García-Martín, M. B., & Ruiz, F. J. (2020). Effect of acceptance and commitment therapy in improving interpersonal skills in adolescents: A randomized waitlist control trial. Journal of Contextual Behavioral Science, 17, 86–94. https://doi.org/10.1016/j.jcbs.2020.06.008.
Byrne, G., Ghráda, Á. N., O’Mahony, T., & Brennan, E. (2021). A systematic review of the use of acceptance and commitment therapy in supporting parents. Psychology and Psychotherapy: Theory Research and Practice, 94(S2), e12282. https://doi.org/10.1111/papt.12282.
Caldas, S. V., Antonsen, L. R., Hamilton, A. S., & Moyer, D. N. (2023). Measurement of psychological flexibility in the context of parenting: A scoping review. Journal of Contextual Behavioral Science, 30, 61–69. https://doi.org/10.1016/j.jcbs.2023.09.001.
Cederberg, J. T., Weineland, S., Dahl, J., & Ljungman, G. (2018). A preliminary validation of the Swedish short version of the Avoidance and Fusion Questionnaire for Youth (AFQ-Y8) for children and adolescents with cancer. Journal of Contextual Behavioral Science, 10, 103–107. https://doi.org/10.1016/j.jcbs.2018.09.004.
Daks, J. S., & Rogge, R. D. (2020). Examining the correlates of psychological flexibility in romantic relationship and family dynamics: A meta-analysis. Journal of Contextual Behavioral Science, 18, 214–238. https://doi.org/10.1016/j.jcbs.2020.09.010.
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment device. Journal of Marital and Family Therapy, 9(2), 171–180. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x.
Fergus, T. A., Valentiner, D. P., Gillen, M. J., Hiraoka, R., Twohig, M. P., Abramowitz, J. S., & McGrath, P. B. (2012). Assessing psychological inflexibility: The psychometric properties of the Avoidance and Fusion Questionnaire for Youth in two adult samples. Psychological Assessment, 24(2), 402–408. https://doi.org/10.1037/a0025776.
Fischer, T. D., Smout, M. F., & Delfabbro, P. H. (2016). The relationship between psychological flexibility, early maladaptive schemas, perceived parenting and psychopathology. Journal of Contextual Behavioral Science, 5(3), 169–177. https://doi.org/10.1016/j.jcbs.2016.06.002.
Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18(3), 233–239. https://doi.org/10.1111/j.1467-9280.2007.01882.x.
Fugmann, D., Richter, P., Karger, A., Ernstmann, N., Hönig, K., Bergelt, C., Faller, H., Maatouk, I., Hornemann, B., Stein, B., Teufel, M., Goerling, U., Erim, Y., Geiser, F., Albus, C., Senf, B., Wickert, M., & Weis, J. (2023). Caring for dependent children impacts practical and emotional problems and need for support, but not perceived distress among cancer patients. Psycho-Oncology, 32(8), 1231–1239. https://doi.org/10.1002/pon.6173.
Gillanders, D. T., Sinclair, A. K., MacLean, M., & Jardine, K. (2015). Illness cognitions, cognitive fusion, avoidance and self-compassion as predictors of distress and quality of life in a heterogeneous sample of adults, after cancer. Journal of Contextual Behavioral Science, 4(4), 300–311. https://doi.org/10.1016/j.jcbs.2015.07.003.
Greco, L. A., Lambert, W., & Baer, R. A. (2008). Psychological inflexibility in childhood and adolescence: Development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychological Assessment, 20(2), 93–102. https://doi.org/10.1037/1040-3590.20.2.93.
Guan, T., Qan’ir, Y., & Song, L. (2021). Systematic review of illness uncertainty management interventions for cancer patients and their family caregivers. Supportive Care in Cancer, 29(8), 4623–4640. https://doi.org/10.1007/s00520-020-05931-x.
Hayes, A. F. (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. Guilford.
Hayes, A. F., & Scharkow, M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychological Science, 24(10), 1918–1927. https://doi.org/10.1177/0956797613480187.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and Commitment Therapy, Second Edition: The Process and Practice of Mindful Change. Guilford Press.
Hong, S. J., Shin, N. M., & Jung, S. (2020). A predictive model of fear of cancer recurrence for patients undergoing chemotherapy. Supportive Care in Cancer, 28(9), 4173–4181. https://doi.org/10.1007/s00520-019-05245-7.
Hulbert-Williams, N. J., & Storey, L. (2016). Psychological flexibility correlates with patient-reported outcomes independent of clinical or sociodemographic characteristics. Supportive Care in Cancer, 24(6), 2513–2521. https://doi.org/10.1007/s00520-015-3050-9.
Hulbert-Williams, N. J., Owen, R., & Nelson, C. J. (2021). Acceptance and Commitment Therapy (ACT) for Cancer Patients. In W. Breitbart, P. Butow, P. Jacobsen, W. Lam, M. Lazenby, & M. Loscalzo (Eds.), Psycho-Oncology (4th ed., pp. 438–444). Oxford Academic. https://doi.org/10.1093/med/9780190097653.001.0001
Inhestern, L., Bultmann, J. C., Beierlein, V., Möller, B., Romer, G., Koch, U., & Bergelt, C. (2016). Understanding parenting concerns in cancer survivors with minor and young-adult children. Journal of Psychosomatic Research, 87, 1–6. https://doi.org/10.1016/j.jpsychores.2016.05.008.
Inhestern, L., Bultmann, J. C., Johannsen, L. M., Beierlein, V., Möller, B., Romer, G., Koch, U., & Bergelt, C. (2021). Estimates of prevalence rates of cancer patients with children and well-being in affected children: A systematic review on population-based findings. Frontiers in Psychiatry, 12, 765314. https://doi.org/10.3389/fpsyt.2021.765314.
Ireland, M. J., & Pakenham, K. I. (2010). Youth adjustment to parental illness or disability: The role of illness characteristics, caregiving, and attachment. Psychology Health & Medicine, 15(6), 632–645. https://doi.org/10.1080/13548506.2010.498891.
Johannsen, L., Brandt, M., Frerichs, W., Inhestern, L., & Bergelt, C. (2022). The impact of cancer on the mental health of patients parenting minor children: A systematic review of quantitative evidence. Psycho-Oncology, 31(6), 869–878. https://doi.org/10.1002/pon.5912.
Kazlauskaite, V., & Mendenhall, T. (2023). Providers working with parents who are diagnosed with cancer. Current Psychology. https://doi.org/10.1007/s12144-023-05208-6.
Kuswanto, C. N., Stafford, L., Sharp, J., & Schofield, P. (2018). Psychological distress, role, and identity changes in mothers following a diagnosis of cancer: A systematic review. Psycho-Oncology, 27(12), 2700–2708. https://doi.org/10.1002/pon.4904.
Landi, G., Andreozzi, M. S., Pakenham, K. I., Grandi, S., & Tossani, E. (2020). Psychosocial adjustment of young offspring in the context of parental type 1 and type 2 diabetes: A systematic review. Diabetic Medicine, 37(7), 1103–1113. https://doi.org/10.1111/dme.14271.
Landi, G., Pakenham, K. I., Benassi, M., Giovagnoli, S., Tossani, E., & Grandi, S. (2021). A model of the effects of parental illness on youth adjustment and family functioning: The moderating effects of psychological flexibility on youth caregiving and stress. International Journal of Environmental Research and Public Health, 18(9), 4902. https://doi.org/10.3390/ijerph18094902.
Landi, G., Boccolini, G., Giovagnoli, S., Pakenham, K. I., Grandi, S., & Tossani, E. (2022a). Validation of the Italian young carer of parents inventory-revised (YCOPI-R). Disability and Rehabilitation, 44(5), 795–806. https://doi.org/10.1080/09638288.2020.1780478.
Landi, G., Duzen, A., Patterson, P., McDonald, F. E. J., Crocetti, E., Grandi, S., & Tossani, E. (2022b). Illness unpredictability and psychosocial adjustment of adolescent and young adults impacted by parental cancer: The mediating role of unmet needs. Supportive Care in Cancer, 30(1), 145–155. https://doi.org/10.1007/s00520-021-06379-3.
Levin, M. E., MacLane, C., Daflos, S., Seeley, J., Hayes, S. C., Biglan, A., & Pistorello, J. (2014). Examining psychological inflexibility as a transdiagnostic process across psychological disorders. Journal of Contextual Behavioral Science, 3(3), 155–163. https://doi.org/10.1016/j.jcbs.2014.06.003.
Li, Z., Li, Y., Guo, L., Li, M., & Yang, K. (2021). Effectiveness of acceptance and commitment therapy for mental illness in cancer patients: A systematic review and meta-analysis of randomised controlled trials. International Journal of Clinical Practice, 75(6), e13982. https://doi.org/10.1111/ijcp.13982.
Mesters, I., van den Borne, H., McCormick, L., Pruyn, J., de Boer, M., & Imbos, T. (1997). Openness to discuss Cancer in the nuclear family: Scale, development, and validation. Psychosomatic Medicine, 59(3), 269.
Morris, J., Turnbull, D., Preen, D., Zajac, I., & Martini, A. (2018). The psychological, social, and behavioural impact of a parent’s cancer on adolescent and young adult offspring aged 10–24 at time of diagnosis: A systematic review. Journal of Adolescence, 65, 61–71. https://doi.org/10.1016/j.adolescence.2018.03.001.
Mota-George, G., Martinez, A., & Dains, J. E. (2023). Quality of life in adult cancer patients with underage children: An integrative review. Journal of the Advanced Practitioner in Oncology, 14(5), 390–402. https://doi.org/10.6004/jadpro.2023.14.5.4.
Muriel, A. C., Moore, C. W., Baer, L., Park, E. R., Kornblith, A. B., Pirl, W., Prigerson, H., Ing, J., & Rauch, P. K. (2012). Measuring psychosocial distress and parenting concerns among adults with cancer. Cancer, 118(22), 5671–5678. https://doi.org/10.1002/cncr.27572.
Muthén, L. K., & Muthén, B. O. (1998–2018). Mplus User’s Guide. Eighth Edition Muthén & Muthén.
Newman, R., Kaldenberg, J., Stursberg, L., Pinto, B., Jimenez, C., & Glazer, K. (2023). Parents living with and beyond cancer: A scoping review of unmet supportive care needs and impact on daily life. British Journal of Occupational Therapy, 86(9), 599–614. https://doi.org/10.1177/03080226231183281.
Novakov, I. (2021). Emotional state, fatigue, functional status and quality of life in breast cancer: Exploring the moderating role of psychological inflexibility. Psychology Health & Medicine, 26(7), 877–886. https://doi.org/10.1080/13548506.2020.1842896.
Özönder Ünal, I., Ünal, C., Duymaz, T., & Ordu, C. (2023). The relationship between psychological flexibility, self-compassion, and posttraumatic growth in cancer patients in the COVID-19 pandemic. Supportive Care in Cancer, 31(7), 428. https://doi.org/10.1007/s00520-023-07891-4.
Pakenham, K. I., Landi, G., Boccolini, G., Furlani, A., Grandi, S., & Tossani, E. (2020). The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science, 17, 109–118. https://doi.org/10.1016/j.jcbs.2020.07.003.
Pakenham, K. I., Landi, G., Cattivelli, R., Grandi, S., & Tossani, E. (2023). Identification of psychological flexibility and inflexibility profiles during the COVID-19 pandemic. Journal of Clinical Psychology. https://doi.org/10.1002/jclp.23536.
Patton, G. C., Sawyer, S. M., Santelli, J. S., Ross, D. A., Afifi, R., Allen, N. B., Arora, M., Azzopardi, P., Baldwin, W., Bonell, C., Kakuma, R., Kennedy, E., Mahon, J., McGovern, T., Mokdad, A. H., Patel, V., Petroni, S., Reavley, N., Taiwo, K., & Viner, R. M. (2016). Our future: A Lancet commission on adolescent health and wellbeing. The Lancet, 387(10036), 2423–2478. https://doi.org/10.1016/S0140-6736(16)00579-1.
Pedersen, S., & Revenson, T. A. (2005). Parental illness, family functioning, and adolescent well-being: A family ecology framework to guide research. Journal of Family Psychology, 19, 404–419. https://doi.org/10.1037/0893-3200.19.3.404.
Probst, T., Baumeister, H., McCracken, L. M., & Lin, J. (2018). Baseline psychological inflexibility moderates the outcome pain interference in a randomized controlled trial on internet-based acceptance and commitment therapy for chronic pain. Journal of Clinical Medicine, 8(1), 24. https://doi.org/10.3390/jcm8010024.
Salari, N., Rezaie, L., Khazaie, H., Bokaee, S., Ghasemi, H., Mohammadi, M., & Khaledi-Paveh, B. (2023). The effect of acceptance and commitment therapy on anxiety and depression in patients with cancer: A systematic review. Current Psychology, 42(7), 5694–5716. https://doi.org/10.1007/s12144-021-01934-x.
Sommet, N., Weissman, D. L., Cheutin, N., & Elliot, A. J. (2023). How many participants do I need to test an interaction? Conducting an appropriate power analysis and achieving sufficient power to detect an interaction. Advances in Methods and Practices in Psychological Science, 6(3). https://doi.org/10.1177/25152459231178728.
Stockton, D., Kellett, S., Berrios, R., Sirois, F., Wilkinson, N., & Miles, G. (2019). Identifying the underlying mechanisms of change during Acceptance and Commitment Therapy (ACT): A systematic review of contemporary mediation studies. Behavioural and Cognitive Psychotherapy, 47(3), 332–362. https://doi.org/10.1017/S1352465818000553.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660.
Walczak, A., McDonald, F., Patterson, P., Dobinson, K., & Allison, K. (2018). How does parental cancer affect adolescent and young adult offspring? A systematic review. International Journal of Nursing Studies, 77, 54–80. https://doi.org/10.1016/j.ijnurstu.2017.08.017.
Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-Item short-form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
World Health Organization (2022). Cancer: Key Facts. https://www.who.int/news-room/fact-sheets/detail/cancer.
Zhao, C., Lai, L., Zhang, L., Cai, Z., Ren, Z., Shi, C., Luo, W., & Yan, Y. (2021). The effects of acceptance and commitment therapy on the psychological and physical outcomes among cancer patients: A meta-analysis with trial sequential analysis. Journal of Psychosomatic Research, 140, 110304. https://doi.org/10.1016/j.jpsychores.2020.110304.
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization: G.L, K.I.P., E.T, S.G.; Methodology: G.L, K.I.P., R.C., L.G.; Formal analysis and investigation: G.L; Writing—original draft preparation: G.L., K.I.P.; Writing—review and editing: G.L, K.I.P., R.C., L.G., S.G., E.T; Supervision: K.I.P., E.T, S.G.
Corresponding author
Ethics declarations
Competing interests
The authors report there are no competing interests to declare.
Ethical approval
The authors declare no competing interests that are relevant to the content of this article. This study was approved by the University of Bologna ethics committee (ethics approval number: 148,989) and informed consent was obtained from all participants.
Consent for publication
All authors agreed to the submission of the manuscript and agree to take responsibility and be accountable for the contents of the article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Landi, G., Pakenham, K.I., Cattivelli, R. et al. Parental cancer: mediating and moderating roles of psychological inflexibility in the links between illness severity and parental quality of life and family outcomes. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06008-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12144-024-06008-2