Abstract
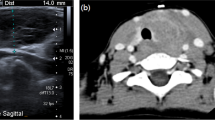
Thyroid gland involvement by Langerhans cell histiocytosis is extremely rare. A 35-year-old woman with a history of a suprasellar mass previously diagnosed as a ganglioglioma and complicated by diabetes insipidus, hypogonadotropic hypogonadism, and central hypothyroidism presented with acute onset of neck enlargement. On ultrasound examination, almost the entire thyroid appeared replaced by abnormal lobulated hypoechoic tissue with increased vascularity. Fine needle aspiration (FNA) of the thyroid was performed and revealed singly scattered and loosely cohesive large cells with abundant cytoplasm, including some with irregular nuclear contours and nuclear grooves. No thyroid follicular cells were noted. Based on the cytomorphologic findings and ancillary studies (immunohistochemistry and flow cytometry analysis) a cytological diagnosis of “positive for neoplastic cells” with features suggestive of monocytic/histiocytic origin, possibly Langerhans cell histiocytosis (LCH) was rendered. Following FNA, the patient underwent an incisional thyroid biopsy that confirmed the cytological impression of LCH. In light of the new diagnosis of LCH, the prior suprasellar mass biopsy slides were re-reviewed and rare cells suspicious for LCH were observed. Appropriate treatment for systemic LCH was initiated successfully. This case demonstrates that the presence of enlarged and loosely cohesive cells, especially those with irregular nuclear contours, in thyroid FNA specimens should raise suspicion for LCH. The diagnosis of LCH in FNA specimens is challenging. Additional material should be allocated for ancillary studies to confirm the morphological impression. In our case, not only was the thyroid FNA crucial in diagnosing LCH, but instrumental in initiating a thorough diagnostic work-up for multisystem involvement and thus unmasking the true etiology of the patient’s suprasellar mass and associated endocrinopathies.





Similar content being viewed by others
References
Hand A. Polyuria and tuberculosis. Proc Pathol Soc Phila. 1893;16:282–4 (Archives of Pediatrics, New York, 1893: 10: 673–675).
Willman CL, McClain KL. An update on clonality, cytokines, and viral etiology in Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12(2):408–16.
Egeler RM, D’Angio GJ. Langerhans cell histiocytosis. J Pediatr. 1995;127(1):1–11.
Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other Langerin-expressing dendritic cells. Nat Rev Immunol. 2008;8(12):935–47.
Romani N, Clausen BE, Stoitzner P. Langerhans cells and more: langerin-expressing dendritic cell subsets in the skin. Immunol Rev. 2010;234(1):120–41.
Patten DK, Wani A, Tolley N. Solitary Langerhans histiocytosis of the thyroid gland: a case report and literature review. Head Neck Pathol. 2012;6(2):279–89. doi:10.1007/s12105-011-0321-8.
Merad M, Manz MG, Karsunky H, Wagers A, Peters W, Charo I, Weissman IL, Cyster JG, Engleman EG. Langerhans cells renew in the skin throughout life under steady-state conditions. Nat Immunol. 2002;3(12):1135–41.
Willman CL, Busque L, Griffith BB, Favara BE, McClain KL, Duncan MH, Gilliland DG. Langerhans’-cell histiocytosis (histiocytosis X)—a clonal proliferative disease. N Engl J Med. 1994;331(3):154–60.
Mete Ö, Doğan Ö, Kapran Y, Tihan D, Erbil Y, Ozarmağan S. Interstitial Langerhans cell histiocytosis-like lesion in an adult presented with diverticulitis: a reactive or neoplastic condition? Pathol Oncol Res. 2011;17(2):403–7.
Berres ML, Lim KP, Peters T, et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med. 2014;211(4):669–83.
Chakraborty R, Hampton OA, Shen X, et al. Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood. 2014;123(19):3007–15.
Haroche J, Charlotte F, Arnaud L, et al. High prevalence of BRAF V600E mutations in Erdheim–Chester disease but not in other non-Langerhans cell histiocytoses. Blood. 2012;120(13):2700–3.
Hervier B, Harcoche J, Arnaud L. Association of both Langerhans cell histiocytosis and Erheim–Chester disease linked to the BTAFV600E mutation. Blood. 2014;124(7):1119–26. doi:10.1182/blood-2013-12-543793.
Brown NA, Furtado LV, Betz BL, et al. High prevalence of somatic MAP2K1 mutations in BRAF V600E-negative Langerhans cell histiocytosis. Blood. 2014;124(10):1655–8.
Nelson DS, Quispel W, Badaliam-Very G, et al. Somatic activating ARAF mutations in Langerhans cell histiocytosis. Blood. 2014;123(20):3152–5.
Thompson LD. Langerhans cell histiocytosis isolated to the thyroid gland. Eur Arch Otorhinolaryngol. 1996;253:62–5. doi:10.1007/BF00176706.
Thompson LD, Wenig BM, Adair CF, Smith BC, Heffess CS. Langerhans cell histiocytosis of the thyroid: a series of seven cases and a review of the literature. Mod Pathol. 1996;9:145–9.
Lassalle A, Hofman V, Santini J, Sadoul JL, Hofman P. Isolated Langerhans cell histiocytosis of the thyroid and Graves’ diseases: an unreported association. Pathology. 2008;40:525–7.
Abarra A, Chhina N, Joharatnam J, Tharakkan G, Todd J. Langerhans cell histiocytosis and Graves’ disease. Presented at society for endocrinology BES. Harrogate; 2012. Endocrine Abstracts, 28, p. 372.
Goldstein N, Layfield LJ. Thyromegaly secondary to simultaneous papillary thyroid carcinoma and histiocytosis X. Report of a case and review of the literature. Acta Cytol. 1991;35(4):422–6.
Diego E, Biagetti B, Iglesias C, Gonzales O, Mesa J. Langerhans cell histiocytosis and papillary thyroid carcinoma. Rev Clin Esp. 2014;214(2):e19–21.
Kirchgraber PR, Weaver MG, Arafah BM, Abdul-Karim FW. Fine needle aspiration cytology of Langerhans cell histiocytosis involving the thyroid. Acta Cytol. 1994;38:101–6.
Dey P, Luthra UK, Sheikh ZA. Fine needle aspiration cytology of Langerhans cell histiocytosis of the thyroid. Acta Cytol. 1999;43:429–31. doi:10.1159/000331093.
Sahoo M, Karak AS, Bhatnagar D, Bal CS. Fine-needle aspiration cytology in a case of isolated involvement of thyroid with Langerhans cell histiocytosis. Diagn Cytopathol. 1998;19:33–7. doi:10.1002/(SICI)1097-0339(199807)19:1<33:AID-DC7>3.0.CO;2-P.
Ma JT, Ho FC, Wang C, Lam KS, Yeung RT. Primary hypothyroidism and essential hypernatremia in a patient with histiocytosis X. Aust NZ J Med. 1985;15:72–4.
Akhtar M, Ali MA, Bakry M, Sackey K, Sabbah R. Fine-needle aspiration biopsy of Langerhans histiocytosis (histiocytosis-X). Diagn Cytopathol. 1993;9(5):527–33.
Kumar N, Sayed S, Vinayak S. Diagnosis of Langerhans cell histiocytosis on fine needle aspiration cytology: a case report and review of the cytology literature. Pathol Res Int. 2011;20:439518. doi:10.4061/2011/439518.
Acknowledgments
Presented in part at the 84th Annual American Thyroid Association Meeting, October 29–November 2, 2014, Coronado, CA and received Trainee’s Poster Contest Award.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saqi, A., Kuker, A.P., Ebner, S.A. et al. Langerhans Cell Histiocytosis: Diagnosis on Thyroid Aspirate and Review of the Literature. Head and Neck Pathol 9, 496–502 (2015). https://doi.org/10.1007/s12105-015-0608-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-015-0608-2