Abstract
Objectives
To determine the clinical profile and outcome of children requiring noninvasive ventilation (NIV) in a PICU.
Methods
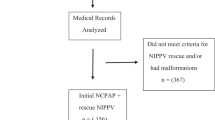
This prospective observational study was conducted in the PICU at Dayanand Medical College and Hospital, Punjab. Children (1 mo–18 y) with moderate-to-severe respiratory distress who received NIV during one-year period were included. Failure was defined as the need for endotracheal intubation. The patients received bilevel positive airway pressure (BiPAP) with inspiratory and expiratory positive airway pressure (8–18 cm H2O and 4–8 cm), respectively and indigenous continuous positive airway pressure (CPAP) were included. Vital signs (heart rate, respiratory rate) and gasometric parameters (pH, HCO3, pCO2, pO2) were recorded.
Results
Out of total 115 patients, 81.7% were successfully treated by NIV whereas 18.3% constituted NIV failure group. Two types of NIV were used, 65.2% were started on BiPAP and 34.8% on indigenous bubble CPAP. Most common diagnosis was tropical fever (24.3%), bronchopneumonia (20%), and sepsis with multiple organ dysfunction syndrome (MODS) (7.8%). Commonest indication of NIV was respiratory distress (70.4%) and prevention of postextubation respiratory failure (20.8%). Seven patients (6.9%) died during the study. NIV failure is higher in children with sepsis with MODS, abnormal blood gas (acidosis), and moderate-to-severe acute respiratory distress syndrome (ARDS).
Conclusions
This study demonstrates that NIV is an effective form of respiratory support for children with acute respiratory distress/failure. Sepsis with MODS, acidosis and ARDS (moderate to severe) were predictors of NIV failure. Careful patient selection may help in judicious use of NIV in PICU.

Similar content being viewed by others
References
Liesching T, Kwok H, Hill NS. Acute applications of noninvasive positive pressure ventilation. Chest. 2003;124:699–713.
Dohna-Schwake C, Stehling F, Tschiedel E, Wallot M, Mellies U. Non invasive ventilation on a pediatric intensive care unit: feasibility, efficacy and predictors of success. Pediatr Pulmonol. 2011;46:1114–20.
Deis JN, Abramo TJ, Crawley L. Noninvasive respiratory support. Pediatr Emerg Care. 2008;24:331–9.
Sharma H, Singh D, Pooni P, Mohan U. A study of profile of ventilator–associated pneumonia in children in Punjab. J Trop Pediatr. 2009;55:393–5.
Khurana S, Bhargava S, Pooni P, et al. Risk factors for extubation failure in mechanically ventilated children in pediatric intensive care unit. Ind J Child Health. 2019;6:379–82.
Morris JV, Ramnarayan P, Parslow RC, Fleming SJ. Outcomes for children receiving noninvasive ventilation as the first line mode of mechanical ventilation at the intensive care admission: apropensity score matched cohort study. Crit Care Med. 2017;45:1045–53.
Wolfer A, Calderini E, Iannella E, et al. Network of Pediatric Intensive care unit study group. Evolution of noninvasive mechanical ventilation use: a cohort study among Italian PICUs. Pediatr Crit Care Med. 2015;16:418–27.
Foder KL. Noninvasive Respiratory support in infants and children. Respir Care. 2017;62:699–717.
Korang SK, Feinberg J, Wetterslev J, Jakobsen JC. Non invasive positive pressure ventilation for acute asthma in children. Cochrane Database Syst Rev. 2016;9:CD012067.
Ganu SS, Gautam A, Wilkins B, Egan J. Increase in use of non – invasive ventilation for infants with severe bronchiolitis is associated with decline in intubation rates over a decade. Intensive Care Med. 2012;38:1177–83
Lum LC, Abdel-Latif ME, de Bruyne JA, Nathan AM, Gan CS. Noninvasive ventilation in a tertiary paediatric intensive care unit in a middle income country. Pediatr Crit Care Med. 2011;12:e7–13.
Almeida L, Ruza F. Insuficiencia respiratoria aguda. In: Tratado de Cuidados Intensivos Pedia´tricos. Third Edition. Ruza F (Ed). Madrid: Norma-Capitel. 2003;730–46.
Teague WG. Noninvasive ventilation in the pediatric intensive care unit for children with acute respiratory failure. Pediatr Pulmonol. 2003;35:418–26.
Emeriaud G, Napolitano N, Polikoff L, et al; National Emergency Airway Registry for Children (NEAR4KIDS)Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI).Impact of failure of noninvasive ventilation on the safety of pediatric tracheal intubation. Crit Care Med. 2020;48:1503–12.
Mayordomo-Colunga J, Medina A, Rey C, et al. Predictive factors of non invasive ventilation failure in critically ill children: a prospective epidemiological study. Intensive Care Med. 2009;35:527–36.
Campion A, Huvenne H, Leteurtre S, et al. Noninvasive ventilation in infants with severe infection presumably due to respiratory syncytial virus: feasibility and failure criteria. Arch Pediatr. 2006;13:1404–9.
Muñoz-Bonet JI, Flor-Macián EM, Brines J, et al. Predictive factors for the outcome of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med. 2010;11:675–80.
Bellani G, Laffey JG, Pham T, et al; LUNG SAFE Investigators; ESICM Trials Group. Noninvasive ventilation of patients with acute respiratory distress syndrome. insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77.
Essouri S, Chevret L, Durand P, Haas V, Fauroux B, Devictor D. Noninvasive positive pressure ventilation: five years of experience in a pediatric intensive care unit. Pediatr Crit Care Med. 2006;7:329–34.
Kovacikoa L, Skrak P, Dobos D, Zahorec M. Noninvasive positive pressure ventilation in critically ill children with cardiac disease. Pediatr Cardiol. 2014;35:676–83.
Ottonello G, Villa G, Doglio L, et al. Noninvasive ventilation with positive airway pressure in pediatric intensive care. Minerva Pediatr. 2007;59:85–9.
Munoz-Bonet JI, Flor-Macian EM, Rosello PM, et al. Noninvasive ventilation in pediatric acute respiratory failure by means of a conventional volumetric ventilator. World J Pediatr. 2010;6:323–30.
James CS, Hallewell CP, James DP, Wade A, Mok QQ. Predicting the success of non–invasive ventilation in preventing intubation and reintubation in the paediatric intensive care unit. Intensive Care Med. 2011;37:1994–2001.
Yañez LJ, Yunge M, Emilfork M, et al. A prospective, randomized, controlled trial of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med.2008;9:484–9.
Bernet V, Hug, MI, Frey B. Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med. 2005;6:660–4.
Demoule A, Girou E, Richard JC, Taillé S, Brochard L. Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med. 2006;32:1747–55.
Carrillo A, Gonzalez-Diaz G, Ferrer M, et al. Non invasive ventilation in community acquired pneumonia and severe acute respiratory failure. Intensive Care Med. 2012;38:458–66.
Acknowledgements
The authors wish to thank Dr Deepak Bhat, Dr GS Dhooria, Dr Goraya, Dr Kamal A., and Dr Shruti Kakkar for their constant encouragement and the PICU nurses for their contribution in the patient care.
Author information
Authors and Affiliations
Contributions
PAP conceived this study; DP, SB helped with data collection and analysis; and PAP, KSG prepared the manuscript. All authors approved the manuscript before submitting. PAP will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Punn, D., Gill, K.S., Bhargava, S. et al. Clinical Profile and Outcome of Children Requiring Noninvasive Ventilation (NIV). Indian J Pediatr 89, 466–472 (2022). https://doi.org/10.1007/s12098-021-03965-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-021-03965-5