Abstract
Purpose
To determine whether physiological parameters and underlying condition can be used to predict which patients can be managed successfully on non-invasive ventilation (NIV).
Methods
Review of case notes and computerised data of every paediatric intensive care unit (PICU) admission over 7 years where NIV was commenced. Data immediately prior to commencing NIV and 2 h after its establishment was collected. Univariable and multivariable statistical analysis was performed to compare variables.
Results
Eighty-three patients commenced NIV attempting to avoid intubation and 64% succeeded. Those who failed required a higher FiO2 (0.56 vs. 0.47, p = 0.038), had higher respiratory rates (53.3 vs. 40.3 breaths/min, p = 0.012) and lower pH (7.26 vs. 7.34, p = 0.032) before NIV and higher FiO2 after NIV commenced (0.54 vs. 0.43, p = 0.009). Those with a respiratory diagnosis were more likely to be successful. Patients with oncologic disease, particularly if septic, were less likely to avoid intubation using NIV. Multivariable models showed that after adjustment for mode of NIV and underlying diagnosis, respiratory rate before NIV was an independent predictor of success [adjusted odds ratio (OR) 0.95 (0.91, 0.99), p = 0.01]. Eighty patients were extubated to NIV but 15 required re-intubation. Those re-intubated had a higher systolic blood pressure (104 vs. 77.9 mmHg, p = 0.001) and diastolic blood pressure (64.5 vs. 54.1 mmHg, p = 0.0037) after extubation. Multivariable models showed that systolic blood pressure 2 h after extubation was independently associated with outcome [adjusted OR 0.96 (0.93, 0.99), p = 0.007].
Conclusions
Parameters relating to respiratory and cardiovascular status can determine which patients will successfully avoid intubation or re-intubation when placed on NIV. Underlying disease and reason for admission should be considered when predicting the outcome of NIV.
Similar content being viewed by others
Introduction
Endotracheal intubation and mechanical ventilation in critically ill adults and children carries with it a number of potentially serious complications including ventilator-associated pneumonia and sedation-related issues. This can significantly add to morbidity and mortality [1].
Non-invasive ventilation (NIV) is an alternative form of ventilatory support in critical care. It encompasses modes of respiratory support including continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP).
The ability to avoid endotracheal intubation by using NIV means that the upper airway remains intact and both physiological functions and airway defence mechanisms are preserved.
A number of controlled studies and meta-analysis have shown its efficiency in adults [2–6], but experience in the paediatric population is limited [7–10]. Despite this, NIV is frequently used in paediatric intensive care units (PICU) to avoid intubation and prevent re-intubation.
In adults, several retrospective [11, 12] and prospective [13, 14] studies have identified predictive factors for NIV success, but much less information exists for children [15–20].
The aims of this study were to determine whether physiological parameters, as well as the underlying condition requiring respiratory support, can be used to predict which patients in the PICU are likely to be managed successfully with NIV—both as a first-line therapy to avoid intubation and in preventing re-intubation once a child has been extubated. This would allow us to use the technique appropriately and design criteria to aid the clinician in deciding early which patients require intubation.
Materials and methods
Great Ormond Street Children’s Hospital has a 20-bed PICU with an average of 900 admissions per year of which an average of 90% are ventilated. External referrals account for around 67% of admissions.
Every patient who was admitted to our PICU between 1st January 2002 and 31st December 2008 who received NIV was analysed. Both CPAP and BiPAP were considered as modes of NIV [21]. This period was selected because of the availability of archived computerised data, and the attending consultants remained constant in that time. All infants under 1 month of age were excluded from the study as were children managed on the cardiac ICU. Unlike previous studies on predictive factors for NIV success in children [18–20], we did not have any exclusion criteria for commencing NIV based on the amount of oxygen being delivered to the patient, pH or underlying condition. The study was approved by the institutional review board and, as the study was retrospective with no identifiable patient data published, parental consent was not required.
The overall population was divided into two groups depending on whether NIV was used as a first-line treatment or post-extubation to prevent re-intubation and then further divided according to whether CPAP or BiPAP was delivered. NIV was delivered through either an Evita (Dragerwerk, Lubeck, Germany), Servo I (Siemens-Elema, Solna, Sweden) or Servo 300 (Siemens-Elema, Solna, Sweden) ventilator set in CPAP or BiPAP mode.
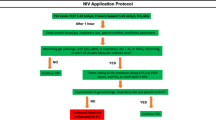
The decision to trial NIV was at the discretion of the attending consultant physician. Although there is no written unit protocol, patients with oncologic disease or neuromuscular weakness were more likely to be commenced on BiPAP. Otherwise, in most patients, CPAP was commenced initially and changed to BiPAP in those whose evolution was not favourable. NIV was stopped and the patient intubated purely at the discretion of the consultant physician when it appeared that the patient was not managing on NIV, but with no set criteria for intubation.
The nasal or facial mask was chosen to provide an optimal fit to the child’s face. Sedation was administered, if required, to a level that improved co-operation without altering respiratory drive. The department policy on oral sedation for such patients was either alimemazine 1–2 mg/kg/dose (max 4 mg/kg/day) or chloral hydrate 30–50 mg/kg/dose (max 200 mg/kg/day).
The underlying condition and reason for needing respiratory support were noted for each case after careful examination of the case notes. Demographic data including age, sex and Paediatric Index of Mortality 2 (PIM2) score were also recorded.
Since 1st January 2002 the PICU has used the CareVue (Philips) system for real-time electronic patient data collection. Clinical staff enter data hourly for every patient, including mode of ventilation, drug administration, physiological parameters and blood gas analysis. Data for every patient admitted to PICU from 1st January 2002 is stored centrally and was available to the researchers.
Physiological parameters relating to respiratory and cardiovascular status were noted from the electronic records immediately prior to commencing NIV and 2 h following its establishment (0 h and 2 h). Blood gas variables were recorded from a blood gas taken immediately prior to commencing NIV and 2 h after its establishment. Capillary samples were taken from most patients (after warming the peripheral extremity) unless an arterial line was in situ or an arterial sample was deemed necessary by the attending physician. FiO2 was delivered to maintain SaO2 between 90 and 95%.
Statistical analysis
Categorical variables were expressed as whole numbers and continuous variables as mean (standard deviation, SD). Univariable analysis was initially performed using the unpaired Student’s t test to compare variables between the success and failure groups. The underlying condition and reason for admission were compared between groups using exact tests (StatXact v. 4.0.1).
Logistic regression models were used to identify significant associations between NIV success and age, sex and physiological parameters. When models were used comparing CPAP or BiPAP, the mode of support required during the initial 2 h post-NIV establishment was determined. Hence patients placed onto BiPAP as a first-line treatment or who transition to BiPAP within 2 h as CPAP provided insufficient support were analysed in the BiPAP cohort. Similarly, a patient doing well on BiPAP who transitions to CPAP after many days would be included in the BiPAP cohort.
Multiple imputation was used in SPSS v17.0 and multivariable models were investigated using stepwise procedures ensuring that any additional predictive factors were independently associated (adjusted p < 0.05) and increased the goodness of fit. Estimated probabilities of success were obtained from the fitted logistic models. The percentages correctly predicted were obtained by dichotomising the estimated probabilities at 0.5 and comparing with whether the individual was successfully managed or not.
A difference was considered statistically significant at a p value of no greater than 0.05. Estimates are presented with 95% confidence intervals (CI).
Results
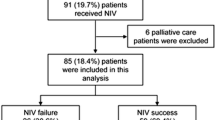
One hundred and sixty-three patients were commenced on NIV during the 7-year study period (Fig. 1).
Eighty-three patients were commenced on NIV as a first-line treatment to avoid intubation which was successful in 53 (64%) cases and unsuccessful in 30 (36%). CPAP alone was administered in 55 cases and BiPAP in 28. CPAP alone was successful in 73% cases and BiPAP in 46%.
Eighty patients were commenced on NIV post-extubation in order to prevent re-intubation which was successful in 65 (81%) cases and unsuccessful in 15 (19%). CPAP alone was used in 57 cases with an 88% success rate and BiPAP used in 23 cases being successful 65% of the time.
The baseline characteristics of the two groups, including the underlying condition requiring support, are shown in Table 1.
Tables 2 and 3 show a comparison of age, PIM2 score and cardiorespiratory parameters between the success and failure groups immediately prior to commencing NIV and 2 h after its establishment, for the first-line treatment and post-extubation cohorts, respectively.
When NIV was being used as a first-line treatment, the respiratory rate before NIV was significantly higher in those individuals who failed their trial (53.3 vs. 40.3 breaths/min, p = 0.012) and these individuals were significantly more acidotic (7.26 vs. 7.34, p = 0.032) compared with those in whom intubation was avoided. Those who failed the trial of NIV required significantly more fractional inspired oxygen (FiO2) before NIV (0.56 vs. 0.47, p = 0.038) to maintain the same partial pressure of oxygen (PO2) (8.73 vs. 8.74 kPa, p = 0.997) and required a higher FiO2 after NIV was applied (0.54 vs. 0.43, p = 0.009).
Patients on CPAP were more likely to avoid intubation with the odds of success being just over three times more in this group compared with the BiPAP group [OR 3.08, 95% CI (1.19, 7.96), p = 0.02]. The univariate coefficients and associations were little changed by adjustment for CPAP/BiPAP choice. After accounting for CPAP/BiPAP and respiratory rate before NIV [adjusted coefficient 0.96 (0.91, 0.99), p = 0.01] no other factors were independently significant. This model correctly predicted 67% of the successes and failures.
When NIV was used post-extubation, those individuals who failed their trial of NIV had significantly higher systolic blood pressures 2 h after NIV was established compared with those individuals in whom re-intubation was prevented (104 vs. 77.9 mmHg, p = 0.001). This group also had higher diastolic blood pressures 2 h after NIV (64.5 vs. 54.1 mmHg, p = 0.037) and mean arterial blood pressures (76.6 vs. 66.7 mmHg, p = 0.064). Those who were successfully extubated had a significant drop in systolic blood pressure (92.6 vs. 77.9 mmHg, p = 0.0015) and diastolic blood pressure (66.8 vs. 54.1 mmHg, p = 0.006).
Patients on CPAP were again more likely to avoid intubation compared with those on BiPAP [OR 3.81, 95% CI (1.19, 12.24), p = 0.025], but again, accounting for CPAP/BiPAP choice had little effect on the univariate coefficients. When multivariable analysis was performed [adjusted OR (CI)], after accounting for CPAP/BiPAP choice and systolic blood pressure after 2 h of NIV [0.96 (0.93, 0.99), p = 0.007], nothing else was independently associated with outcome. This model correctly predicted 79% of successes and failures.
Table 4 shows the success rates of NIV in preventing intubation for different underlying conditions in the first-line treatment and post-extubation cohorts.
During the 7-year study period, the majority of admissions to PICU where NIV was attempted as a first-line treatment to avoid intubation were for primary respiratory illnesses (43%) or a complication related to underlying malignancy (28%). Children with a primary respiratory illness who were treated with NIV avoided intubation in 30/36 cases (83%). Those with an underlying oncological condition successfully avoided intubation in only 8/23 cases (35%). Only 3/15 (20%) with an underlying oncological condition who were admitted because of sepsis successfully avoided intubation. Statistical analysis with exact testing gives a significantly different distribution between those successful on NIV and those not (p = 0.0007)—those with a primary respiratory illness being largely successful and the oncology patients, particularly if septic, not. After adjustment for CPAP/BiPAP choice and diagnosis, respiratory rate prior to NIV remained significantly associated [adjusted OR 0.95 (0.91, 0.99), p = 0.01].
When patients were placed on NIV after extubation, those admitted with a primary respiratory illness successfully avoided re-intubation in 27/33 cases (82%). Each case (6/6) of proven respiratory syncytial virus (RSV)-positive bronchiolitis avoided re-intubation. Children extubated to NIV post-operatively avoided re-intubation in 19/21 cases (90%). With exact testing the distributions are not significantly different (p = 0.9753)—most patients being successful in all diagnostic groups.
Discussion
Studies in the adult population suggest that NIV in acute respiratory failure reduces mortality, need for subsequent mechanical ventilation, and hospital length of stay [3]. Success in this population is, however, dependent on the pathology for which it is used [22].
NIV is also widely studied and well established in the neonates [23]. Since pathologies seen in paediatric critical care differ widely from those in the adult and neonatal intensive care unit, extrapolation from these studies cannot be done.
Despite an increasing use of NIV in the PICU there are few studies on the subject. Those that do exist [15–20] have used small sample numbers and children with limited pathologies.
We investigated predictive factors for the success of NIV in avoiding intubation and preventing re-intubation and also examined the underlying conditions requiring respiratory support with no exclusion on the basis of pathology.
Our study highlights the importance of the underlying condition in predicting the success of NIV. Patients being supported for a primary respiratory illness are more likely to avoid both intubation and re-intubation. Patients with oncologic disease, particularly if septic, are less likely to avoid being intubated by being placed on NIV as a first-line therapy.
Interestingly, our study suggests the importance of the underlying condition rather than the underlying severity of illness. There was no difference in PIM2 scores between success and failure groups within the first-line treatment and post-extubation cohorts. Bernet et al. [15] similarly did not find differences in PIM2 score between patients managed successfully and unsuccessfully on NIV, whereas other studies using Paediatric Risk of Mortality (PRISM) scores [18] and Pediatric Logistic Organ Dysfunction (PELOD) scores [16] have shown a correlation between these prognostic severity scores and prediction of NIV success.
There was no statistically significant difference in age between the success and failure groups in the cohorts we compared. However, the failure groups were on average older and confidence intervals for the differences wide, hence clinically meaningful differences could not be excluded. We therefore considered adjustment for age in our multivariable models but this made little difference whether significant or not. Inclusion of age did not substantially change the other model parameters. The fact that those who failed their trial tended to be older might suggest that they do not tolerate the face mask application of NIV as well as younger patients.
We found that respiratory parameters prior to being placed on NIV in the first-line treatment group were significant in determining success in avoiding intubation—patients who failed their trial of NIV being significantly more tachypnoeic and acidotic as well as needing more oxygen (pre- and post-NIV). Multivariable analysis confirmed the statistical importance of respiratory rate prior to NIV application as well as the FiO2 required on NIV.
The recent study by Muñoz-Bonet et al. [20] examining predictive factors for NIV outcome in a similar population also found that FiO2 requirement on NIV formed part of the success/failure discriminant function, with an FiO2 of greater than 0.57 on NIV predicting failure in nearly 80% of patients. Mayordomo-Colunga et al. [18] reported that their population who failed the trial of NIV also had a statistically significantly higher FiO2 requirement whilst on NIV compared with their success group.
The need for re-intubation has been associated in the adult population with hospital mortality as high as 40% [24] and up to 24% of adult ICU patients require re-intubation due to the development of respiratory failure [25]. The application of NIV to recently extubated patients is therefore theoretically attractive and CPAP has been demonstrated to have a beneficial effect in reducing the likelihood of developing respiratory failure [26].
In predicting success of NIV in preventing re-intubation, we found that those patients who remained hypertensive 2 h after extubation to NIV were significantly more likely to require re-intubation. Those successfully extubated had a statistically significant drop in systolic and diastolic blood pressure after extubation to NIV. No study has described this to date.
The fact that blood pressure was elevated in both groups prior to extubation is unsurprising and likely reflects the fact that sedation has been lifted and the patient is more aware. The finding that those patients who required re-intubation remained hypertensive on NIV is likely to represent a stress response in the failing patient.
We used a combination of CPAP alone and BiPAP in our PICU during the study period. Examining success rates of each revealed the odds of success were greater than three times higher for CPAP over BiPAP. This likely represents the fact that the attending physician will convert from CPAP to BiPAP with patients still showing evidence of respiratory distress on CPAP. BiPAP use was probably therefore reserved for a more distressed population.
BiPAP was also used frequently as a first-line treatment in our unit in patients with oncologic disease to avoid complications associated with invasive ventilation. However, we found that these patients often failed their trial of NIV. The high failure rate on BiPAP might suggest that patients with oncologic disease should be intubated early if evidence of respiratory failure exists rather than attempting rescue with BiPAP.
One aim of our study was to examine the practicality of establishing a protocol for selection of patients and timing of NIV. It appears from the high failure rate of BiPAP that this may not be adequate support for some patients and it may be that our selection of NIV is inappropriate for these individuals. This should be taken into account when writing a unit protocol for use of NIV.
Our study has the limitation of being a retrospective, non-randomised study, but it examines data over a relatively long period of time with a large cohort of paediatric patients. Moreover, data was collected and recorded electronically in real time by clinical staff without the knowledge that the data would later be part of any study. Because of the single-centre setting with a constant group of attending physicians, the NIV procedure and management were also relatively homogenous during the study period.
As a number of our patients received both CPAP and BiPAP, it is difficult to interpret our finding that the univariate coefficients and associations were little changed by adjusting for CPAP or BiPAP choice. Our study period was selected because of the introduction of electronic data collection and because the attending intensivist team members were constant in this time period. A longer study period would have allowed us to obtain a larger cohort of patients who received BiPAP alone.
In the future, randomised controlled trials of paediatric populations would add to our knowledge and ability to provide mechanical ventilatory support to our population in the least harmful and most efficacious way. Such a study would be able to determine hard outcome criteria of NIV compared with conventional ventilation, such as length of ventilation, length of PICU stay and complication rate.
Conclusions
Our results suggest that NIV can play an important role in the PICU in helping to avoid intubation and prevent re-intubation. The underlying condition requiring respiratory support is an important indicator of success and should be taken into account. When used as a first-line treatment to avoid intubating paediatric patients, tachypnoea prior to establishing NIV and oxygen requirement on NIV are predictive factors for failure. In contrast, when NIV is used to prevent re-intubation, persisting hypertension in the hours after establishing NIV should warn the clinician of the likely need for re-intubation.
References
Pingleton SK (1988) Complications of acute respiratory failure. Am Rev Respir Dis 137:1463–1493
Peter JV, Moran JL, Phillips-Hughes J, Warn D (2002) Noninvasive ventilation in acute respiratory failure—a meta-analysis update. Crit Care Med 30:555–562
Keenan SP, Sinuff T, Cook DJ, Hill NS (2004) Does noninvasive positive pressure ventilation improve outcome in acute hypoxaemic respiratory failure? A systemic review. Crit Care Med 32:2516–2523
Girou E, Schortgen F, Delclaux C, Brun-Buisson C, Blot F, Lefort Y, Lemaire F, Brochard L (2000) Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA 284:2361–2367
Confalonieri M, Potena A, Carbone G, Porta RD, Tolley EA, Umberto Meduri G (1999) Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med 160:1585–1591
Hilbert G, Gruson D, Vargas F, Valentino R, Portel L, Gbikpi-Benissan G, Cardinaud JP (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med 344:481–487
Akingbola OA, Servant GM, Custer JR et al (1993) Noninvasive bi-level positive pressure ventilation: management of two pediatric patients. Respir Care 38:1092–1098
Padman R, Lawless S, Von Nessen S (1994) Use of BiPAP by nasal mask in the treatment of respiratory insufficiency in pediatric patients: preliminary investigations. Pediatr Pulmonol 17:119–123
Akingbola OA, Palisano JM, Servant GM et al (1994) BIPAP mask ventilation in pediatric patients with acute respiratory failure. Crit Care Med 22:144
Fortenberry JD, Del Toro J, Jefferson LS, Evey L, Haase D (1995) Management of pediatric acute hypoxaemic respiratory insufficiency with bilevel positive pressure (BiPAP) nasal mask ventilation. Chest 108:1059–1064
Ambrosino N, Foglio K, Rubini F, Clini E, Nava S, Vitacca M (1995) Non-invasive mechanical ventilation for hypercapnic respiratory failure in chronic obstructive pulmonary disease: correlates for success. Thorax 50:755–757
Soo Hoo GW, Santiago S, Williams AJ (1994) Nasal mechanical ventilation for hypercapnic respiratory failure in chronic obstructive pulmonary disease: determinants of success and failure. Crit Care Med 22:1253–1261
Phua J, Kong K, Lee KH, Shen L, Lim TK (2005) Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med 31:533–539
Antonelli M, Conti G, Moro ML, Esquinas A, Gonzalez-Diaz G, Confalonieri M, Pelaia P, Principi T, Gregoretti C, Beltrame F, Pennisi MA, Arcangeli A, Proietti R, Passariello M, Meduri GU (2001) Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multicentre study. Intensive Care Med 27:1718–1728
Bernet V, Hug MI, Frey B (2005) Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med 6:660–664
Essouri S, Chevret L, Durand P, Haas V, Fauroux B, Devictor D (2006) Noninvasive positive pressure ventilation: five years of experience in a paediatric intensive care unit. Pediatr Crit Care Med 7:329–334
Joshi J, Tobias JD (2007) A five-year experience with the use of BIPAP in a pediatric intensive care unit population. J Intensive Care Med 22:38–43
Mayordomo-Colunga J, Medina A, Rey C, Díaz JJ, Concha A, Los Arcos M, Menéndez S (2009) Predictive factors of non invasive ventilation failure in critically ill children: a prospective epidemiological study. Intensive Care Med 35:527–536
Yañez LJ, Yunge M, Emilfork M, Lapadula M, Alcántara A, Fernández C, Lozano J, Contreras M, Conto L, Arevalo C, Gayan A, Hernández F, Pedraza M, Feddersen M, Bejares M, Morales M, Mallea F, Glasinovic M, Cavada G (2008) A prospective, randomized, controlled trial of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 9:484–489
Muñoz-Bonet JI, Flor-Macián EM, Brines J, Roselló-Millet PM, Cruz Llopis M, López-Prats JL, Castillo S (2010) Predictive factors for the outcome of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 11:675–680
L’Her E, Deye N, Lellouche F, Taille S, Demoule A, Fraticelli A, Mancebo J, Brochard L (2005) Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med 172:1112–1118
British Thoracic Society Standards of Care (2002) Non-invasive ventilation in acute respiratory failure. Thorax 57:192–211
Courtney S, Barrington K (2007) Continuous positive airway pressure and noninvasive ventilation. Clin Perinatol 34:73–92
Epstein S, Ciubotaru R (1998) Independent effects of etiology of failure and time of re-intubation on outcome for patients failing extubation. Am J Respir Crit Care Med 158:489–493
Torres A, Gatell JM, Aznar E, el-Ebiary M, Puig de la Bellacasa J, González J, Ferrer M, Rodriguez-Roisin R (1995) Re-intubation increases the risk of nosocomial pneumonia in patients needing mechanical ventilation. Am J Respir Crit Care Med 152:137–141
Hilbert G, Gruson D, Portel L, Gbikpi-Benissan G, Cardinaud JP (1998) Non-invasive pressure support ventilation in COPD patients with post-extubation hypercapnic respiratory insufficiency. Eur Respir J 11:1349–1353
Acknowledgments
No financial support was required for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
James, C.S., Hallewell, C.P.J., James, D.P.L. et al. Predicting the success of non-invasive ventilation in preventing intubation and re-intubation in the paediatric intensive care unit. Intensive Care Med 37, 1994–2001 (2011). https://doi.org/10.1007/s00134-011-2386-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2386-y