Abstract
Objectives
Due to a steadily growing use of stereotactic radiotherapy (SRT) for treatment of brain metastases (BMs), the in-field failure after an initial stereotaxy is an increasingly frequent problem. Repeat stereotactic radiotherapy (re-SRT) shows encouraging results in terms of local control. However, the evidence on prognostic factors limiting the overall survival (OS) of re-treated patients is scarce. Here, we sought to analyze the patients’ and treatment characteristics influencing the survival outcomes after re-SRT.
Methods
Data of all patients with local failure of initial SRT treated from 2012 to 2019 were retrospectively reviewed and cases treated with salvage SRT were analyzed. We analyzed the impact of patients’ and treatment characteristics on overall survival after re-SRT by Kaplan–Meier method and Cox regression models. Local and distant brain control, cause of death, and radionecrosis rate were also assessed.
Results
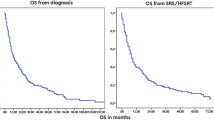
Forty-seven patients with 55 BMs treated with re-SRT were evaluated. Median OS after re-SRT was 9.2 months and the overall local control was 83.6%. Nine BMs (16.4%) presented local relapse (LR), 12 (21.8%) radionecrosis, while 21 patients (44.7%) developed new BMs. Only absence of extracranial metastases at BMs diagnosis (HR 0.42, CI 95%; 0.18–0.97), extracranial disease progression (HR 2.39, CI 95%; 1.06–5.38) and distant brain failure (HR 3.94, CI 95%; 1.68–9.24) after re-SRT were significantly associated with patients’ survival. Extracranial progression following re-SRT was an independent prognosticator of worse OS.
Conclusion
Re-SRT after LR presented excellent local control with acceptable RN rate and improved patients’ survival, limited mainly by extracranial and distant brain progression.


Similar content being viewed by others
Availability of data and materials
The dataset supporting the conclusions of this article is available on request by contacting the authors.
Abbreviations
- BMs:
-
Brain metastases
- SRT:
-
Stereotactic radiotherapy
- re-SRT:
-
Repeat stereotactic radiotherapy
- WBRT:
-
Whole-brain radiotherapy
- Gy:
-
Grays
- fr:
-
Fractions
- LFFS:
-
Local failure-free survival
- mOS:
-
Median overall survival
- NSCLC:
-
Non-small cell lung cancer
- SCLC:
-
Small cell lung cancer
- ORL:
-
Otorhinolaryngology site
- HR:
-
Hazard ratio
- IC:
-
Confidence interval
- LR:
-
Local relapse
- LF:
-
Local failure
- DP:
-
Distal progression
- GTV:
-
Gross target volume
- PTV:
-
Planning target volume
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- MRI:
-
Magnetic resonance imaging
- RN:
-
Radiation necrosis
References
Ostrom QT, Wright CH, Barnholtz-Sloan JS. Brain metastases: epidemiology. Handb Clin Neurol. 2018;149:27–42. https://doi.org/10.1016/B978-0-12-811161-1.00002-5.
Barbour AB, Jacobs CD, Williamson H, et al. Brain metastases treated with radiosurgery or radiation therapy practice patterns for brain metastases in the United States in the stereotactic radiosurgery era. Adv Radiat Oncol. 2019;5(1):43–52. https://doi.org/10.1016/j.adro.2019.07.012.
Sallabanda M, García-Berrocal MI, Romero J, et al. Brain metastases treated with radiosurgery or hypofractionated stereotactic radiotherapy: outcomes and predictors of survival. Clin Transl Oncol. 2020;22:1809–17. https://doi.org/10.1007/s12094-020-02321-x.
Cagney DN, Martin AM, Catalano PJ, et al. Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol. 2017;19(11):1511–21. https://doi.org/10.1093/neuonc/nox077.
Cacho-Díaz B, Spínola-Maroño H, González-Aguilar A, et al. Factors associated with long-term survival in central nervous system metastases. J Neurooncol. 2018;140:159–64. https://doi.org/10.1007/s11060-018-2946-x.
Nieder C, Mehta MP, Geinitz H, Grosu AL. Prognostic and predictive factors in patients with brain metastases from solid tumors: a review of published nomograms. Crit Rev Oncol Hematol. 2018;126:13–8. https://doi.org/10.1016/j.critrevonc.2018.03.018.
Kurtz G, Zadeh G, Gingras-Hill G, et al. Salvage radiosurgery for brain metastases: prognostic factors to consider in patient selection. Int J Radiat Oncol Biol Phys. 2014;88(1):137–42. https://doi.org/10.1016/j.ijrobp.2013.10.003.
Nguyen MN, Noel G, Antoni D. La réirradiation des métastases cérébrales : revue des cinq dernières années [Reirradiation of brain metastasis: Review of the last five years]. Cancer Radiother. 2019;23(6–7):531–40. https://doi.org/10.1016/j.canrad.2019.07.144.
Chidambaram S, Pannullo SC, Schwartz TH, et al. Reirradiation of recurrent brain metastases: where do we stand? World Neurosurg. 2019;125:156–63. https://doi.org/10.1016/j.wneu.2019.01.182.
Gogineni E, Vargo JA, Glaser SM, et al. Long-term survivorship following stereotactic radiosurgery alone for brain metastases: risk of intracranial failure and implications for surveillance and counseling. Neurosurgery. 2018;83:203–9. https://doi.org/10.1093/neuros/nyx376.
Nieder C, Yobuta R, Adler JR. Second re-irradiation of brain metastases: a review of studies involving stereotactic radiosurgery. Cureus. 2018;10(12):e3712. https://doi.org/10.7759/cureus.3712.
Nieder C. Second re-irradiation: a delicate balance between safety and efficacy. Phys Med. 2019;58:155–8. https://doi.org/10.1016/j.ejmp.2019.01.004.
Bilger A, Bretzinger E, Fennell J, et al. Local control and possibility of tailored salvage after hypofractionated stereotactic radiotherapy of the cavity after brain metastases resection. Cancer Med. 2018;7:2350–9. https://doi.org/10.1002/cam4.1486.
Minniti G, Clarke E, Lanzetta G, et al. Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol. 2011;6:48. https://doi.org/10.1186/1748-717X-6-48.
Ayala-Peacock DN, Attia A, Braunstein SE, et al. Prediction of new brain metastases after radiosurgery: validation and analysis of performance of a multi-institutional nomogram. J Neurooncol. 2017;135(2):403–11. https://doi.org/10.1007/s11060-017-2588-4.
Balermpas P, Stera S, von der Müller Grün J, et al. Repeated in-field radiosurgery for locally recurrent brain metastases: feasibility, results and survival in a heavily treated patient cohort. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0198692.
Kim IY, Jung S, Jung TY, et al. Repeat stereotactic radiosurgery for recurred metastatic brain tumors. J Korean Neurosurg Soc. 2018;61:633–9. https://doi.org/10.3340/jkns.2017.0238.
Koffer P, Chan J, Rava P, et al. Repeat stereotactic radiosurgery for locally recurrent brain metastases. World Neurosurg. 2017;104:589–93. https://doi.org/10.1016/j.wneu.2017.04.103.
Dincoglan F, Sager O, Demiral S, et al. Fractionated stereotactic radiosurgery for locally recurrent brain metastases after failed stereotactic radiosurgery. Indian J Cancer. 2019;56(2):151–6. https://doi.org/10.4103/ijc.IJC_786_18.
Chen JC, Petrovich Z, Giannotta SL, Yu C, Apuzzo ML. Radiosurgical salvage therapy for patients presenting with recurrence of metastatic disease to the brain. Neurosurgery. 2000;46(4):860–7. https://doi.org/10.1097/00006123-200004000-00017.
McKay WH, McTyre ER, Okoukoni C, et al. Repeat stereotactic radiosurgery as salvage therapy for locally recurrent brain metastases previously treated with radiosurgery. J Neurosurg. 2017;127:148–56. https://doi.org/10.3171/2016.5.JNS153051.
Rana N, Pendyala P, Cleary RK, et al. Long-term outcomes after salvage stereotactic radiosurgery (SRS) following in-field failure of initial SRS for brain metastases. Front Oncol. 2017;7:279. https://doi.org/10.3389/fonc.2017.00279.
Greto D, Livi L, Bonomo P, et al. Cyberknife stereotactic radiosurgery for the re-irradiation of brain lesions: a single-centre experience. Radiol Med. 2014;119(9):721–6. https://doi.org/10.1007/s11547-014-0383-2.
Moreau J, Khalil T, Dupic G, et al. Second course of stereotactic radiosurgery for locally recurrent brain metastases: safety and efficacy. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0195608.
Loi M, Caini S, Scoccianti S, et al. Stereotactic reirradiation for local failure of brain metastases following previous radiosurgery: systematic review and meta-analysis. Crit Rev Oncol Hematol. 2020;153:103043. https://doi.org/10.1016/j.critrevonc.2020.103043.
Holt DE, Gill BS, Clump DA, et al. Tumor bed radiosurgery following resection and prior stereotactic radiosurgery for locally persistent brain metastasis. Front Oncol. 2015;5:84. https://doi.org/10.3389/fonc.2015.00084.
Iorio-Morin C, Mercure-Cyr R, Figueiredo G, et al. Repeat stereotactic radiosurgery for the management of locally recurrent brain metastases. J Neurooncol. 2019;145(3):551–9. https://doi.org/10.1007/s11060-019-03323-8.
Maranzano E, Trippa F, Casale M, et al. Reirradiation of brain metastases with radiosurgery. Radiother Oncol. 2012;102:192–7. https://doi.org/10.1016/j.radonc.2011.07.018.
Jiang X, Wang H, Song Y, et al. A second course of stereotactic image-guided robotic radiosurgery for patients with cerebral metastasis. World Neurosurg. 2019;123:e621–8. https://doi.org/10.1016/j.wneu.2018.11.238.
Skeie BS, Skeie GO, Enger PØ, et al. Gamma knife surgery in brain melanomas: absence of extracranial metastases and tumor volume strongest indicators of prolonged survival. World Neurosurg. 2011;75(5–6):684–91. https://doi.org/10.1016/j.wneu.2010.12.054 (PMID: 21704936).
Acknowledgements
We would like to thank the Spanish Society of Radiation Oncology (SEOR) and the CRIS Foundation, whose financial support has made this study possible.
Funding
This study received grant from the Spanish Society of Radiation Oncology (SEOR) and CRIS Foundation.
Author information
Authors and Affiliations
Contributions
KH and GL contributed to this study design, carried out the acquisition of data, and drafted the manuscript. KH with IGR statistic support performed statistical analysis. GL and KH participated in data interpretation and manuscript review. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the Gustave Roussy Ethics Committee and conducted in accordance with the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Holub, K., Louvel, G. Efficacy of salvage stereotactic radiotherapy (SRT) for locally recurrent brain metastases after initial SRT and characteristics of target population. Clin Transl Oncol 23, 1463–1473 (2021). https://doi.org/10.1007/s12094-020-02544-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02544-y