Abstract
Fungi are among the predominant pathogens seen in a greater proportion of infections acquired in healthcare settings. A common fungus that causes infections in medical settings is Candida species. Hospitalized patients who suffer from fungal diseases such as candidiasis and candidemia often have elevated rates of mortality and morbidity. It is evident that longer hospital stays have the possibility of bacterial and fungal recurrence and also have a negative economic impact. If left untreated, a Candida infection can spread to other organs and cause a systemic infection that can result in sepsis. Clinicians can treat patients quickly when fungal infections are timely detected, this enhances the results of clinical trials. Developing novel, sensitive, and quick methods for detecting Candida species is imperative. Conventional detection techniques are unsuitable for clinical settings and point-of-care systems as they require expensive equipment and take a longer detection time. This review examines a few of the most widely used biosensor systems for the detection of Candida species, their sensitivity, and the limit of detection. It focuses on various biorecognition elements used and follows utilization and advances in nanotechnology in the context of sensing. In addition to enabling general analysis and quick real-time analysis, crucial for detecting Candida species, biosensors provide an intriguing alternative to more conventional techniques.



Similar content being viewed by others
Abbreviations
- ISFET:
-
Ion-sensitive field-effect transistor
- NAC:
-
N-acetylcysteine
- BMT:
-
Bone marrow transplantation
- OC:
-
Oral candidiasis
- BSA:
-
Broad spectrum antibiotic
- PNA-FISH:
-
Peptide nucleic acid fluorescent in situ hybridization
- SWCNTs:
-
Single-walled carbon nanotubes
- SPR:
-
Surface plasmon resonance
- FET:
-
Field-effect transistor
- SAM:
-
Self-assemble monolayer
- SERS:
-
Surface-enhanced Raman spectral
- NP:
-
Nanoparticle
- LOD:
-
Limit of detection
- AuNP:
-
Gold nanoparticle
- C. albicans :
-
Candida albicans
- NMR:
-
Nuclear magnetic resonance
References
Douglas LJ (2003) Candida biofilms and their role in infection. Trends Microbiol 11:30–36. https://doi.org/10.1016/S0966-842X(02)00002-1
Havlickova B, Czaika VA, Friedrich M (2008) Epidemiological trends in skin mycoses worldwide. Mycoses 51:2–15. https://doi.org/10.1111/j.1439-0507.2008.01606.x
Odds FC (1994) Pathogenesis of Candida infections. J Am Acad Dermatol 31:S2–S5. https://doi.org/10.1016/S0190-9622(08)81257-1
Lim CS-Y, Rosli R, Seow HF, Chong PP (2012) Candida and invasive candidiasis: back to basics. Eur J Clin Microbiol Infect Dis 31:21–31. https://doi.org/10.1007/s10096-011-1273-3
Rodrigues ME, Silva S, Azeredo J, Henriques M (2016) Novel strategies to fight Candida species infection. Crit Rev Microbiol 42:594–606. https://doi.org/10.3109/1040841X.2014.974500
Magill SS et al (2014) Multistate point-prevalence survey of health care-associated infections. N Engl J Med 370:1198–1208. https://doi.org/10.1056/NEJMoa1306801
He Z-X, Shi L-C, Ran X-Y, Li W, Wang X-L, Wang F-K (2016) Development of a lateral flow immunoassay for the rapid diagnosis of invasive candidiasis. Front Microbiol 7:1451. https://doi.org/10.3389/fmicb.2016.01451
Neppelenbroek KH et al (2014) Identification of Candida species in the clinical laboratory: a review of conventional, commercial, and molecular techniques. Oral Dis 20:329–344. https://doi.org/10.1111/odi.12123
Vigneshvar S, Sudhakumari CC, Senthilkumaran B, Prakash H (2016) Recent advances in biosensor technology for potential applications—an overview. Front Bioeng Biotechnol 4:11. https://doi.org/10.3389/fbioe.2016.00011
Rodovalho VR, Alves LM, Castro ACH, Madurro JM, Brito-Madurro AG, Santos AR (2015) Biosensors applied to diagnosis of infectious diseases–an update. Austin J Biosens Bioelectron 1:10–15
da Silva-Junio AG et al (2022) Electrochemical biosensor based on Temporin-PTA peptide for detection of microorganisms. J Pharm Biomed Anal 216:114788. https://doi.org/10.1016/j.jpba.2022.114788
Ribeiro KL et al (2021) Impedimetric clavmo peptide-based sensor differentiates ploidy of candida species. Biochem Eng J 167:107918. https://doi.org/10.1016/j.bej.2020.107918
Singh S, Kumar V, Dhanjal DS, Thotapalli S, Sonali, Singh J (2020) Importance and recent aspects of fungal-based biosensors. In: New and future developments in microbial biotechnology and bioengineering. Elsevier, New York, pp 301–309. https://doi.org/10.1016/B978-0-12-821008-6.00018-9
Patel A et al (2021) Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis 27:2349–2359. https://doi.org/10.3201/eid2709.210934
Alves J, Alonso-Tarrés C, Rello J (2022) How to identify invasive candidemia in ICU—A narrative review. Antibiotics 11:1804. https://doi.org/10.3390/antibiotics11121804
Krcmery V, Barnes AJ (2002) Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. J Hosp Infect 50:243–260. https://doi.org/10.1053/jhin.2001.1151
Talapko J et al (2021) Candida albicans—the virulence factors and clinical manifestations of infection. J Fungi 7:79. https://doi.org/10.3390/jof7020079
Al-Karaawi ZM et al (2002) Molecular characterization of Candida spp. isolated from the oral cavities of patients from diverse clinical settings. Oral Microbiol Immunol 17:44–49. https://doi.org/10.1046/j.0902-0055.2001.00081.x
Millsop JW, Fazel N (2016) Oral candidiasis. Clin Dermatol 34:487–494. https://doi.org/10.1016/j.clindermatol.2016.02.022
Pappas PG et al (2003) A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis 37:634–643. https://doi.org/10.1086/376906
Cleveland AA et al (2015) Declining incidence of candidemia and the shifting epidemiology of candida resistance in two US Metropolitan areas, 2008–2013: results from population-based surveillance. PLoS ONE 10:e0120452. https://doi.org/10.1371/journal.pone.0120452
Blumberg HM et al (2001) Risk Factors for Candidal Bloodstream Infections in Surgical Intensive Care Unit Patients: The NEMIS Prospective Multicenter Study. Clin Infect Dis 33:177–186. https://doi.org/10.1086/321811
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R (1994) Candida colonization and subsequent infections in critically III surgical patients. Ann Surg 220:751–758. https://doi.org/10.1097/00000658-199412000-00008
Mayer FL, Wilson D, Hube B (2013) Candida albicans pathogenicity mechanisms. Virulence 4:119–128. https://doi.org/10.4161/viru.22913
Perlroth J, Choi B, Spellberg B (2007) Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med Mycol 45:321–346. https://doi.org/10.1080/13693780701218689
Spellberg B, Marr KA, Filler SG (2014) Candida: what should clinicians and scientists be talking about? In: Candida and candidiasis. ASM Press, Herndon, pp 1–8. https://doi.org/10.1128/9781555817176.ch1
Lewis JH, Patel HR, Zimmerman HJ (2007) The spectrum of hepatic candidiasis. Hepatology 2:479S-487S. https://doi.org/10.1002/hep.1840020415
Maksymiuk AW, Thongprasert S, Hopfer R, Luna M, Fainstein V, Bodey GP (1984) Systemic candidiasis in cancer patients. Am J Med 77:20–27
Parker JC, McCloskey JJ, Lee RS (1981) Human cerebral candidosis—a postmortem evaluation of 19 patients. Hum Pathol 12:23–28. https://doi.org/10.1016/S0046-8177(81)80238-9
Sánchez-Portocarrero J, Pérez-Cecilia E, Corral O, Romero-Vivas J, Picazo JJ (2000) The central nervous system and infection by Candida species. Diagn Microbiol Infect Dis 37:169–179. https://doi.org/10.1016/S0732-8893(00)00140-1
de Oliveira CS, Colombo AL, Francisco EC, de Lima B, Gandra RF, de Carvalho MCP, de Maia Carrilho CMD, Petinelli R, Pelison M, Helbel C, Czelusniak G, Morales HMP, Perozin JS, Pinheiro RL, Cognialli R, Breda GL, Queiroz-Telles F (2021) Nical and epidemiological aspects of Candidemia in eight medical centers in the state of Parana, Brazil: Parana Candidemia Network. Braz J Infect Dis 25:101041
Fricker-Hidalgo H et al (2001) Evaluation of Candida ID, a new chromogenic medium for fungal isolation and preliminary identification of some yeast species. J Clin Microbiol 39:1647–1649. https://doi.org/10.1128/JCM.39.4.1647-1649.2001
Kitch TT, Jacobs MR, McGinnis MR, Appelbaum PC (1996) Ability of RapID Yeast Plus System to identify 304 clinically significant yeasts within 5 hours. J Clin Microbiol 34:1069–1071. https://doi.org/10.1128/jcm.34.5.1069-1071.1996
Slifkin M (2000) Tween 80 opacity test responses of various Candida species. J Clin Microbiol 38:4626–4628. https://doi.org/10.1128/JCM.38.12.4626-4628.2000
Garbee DD, Pierce SS, Manning J (2017) Opportunistic fungal infections in critical care units. Crit Care Nurs Clin North Am 29:67–79. https://doi.org/10.1016/j.cnc.2016.09.011
de Oliveira-Santos GC et al (2018) Candida infections and therapeutic strategies: mechanisms of action for traditional and alternative agents. Front Microbiol 9:1351. https://doi.org/10.3389/fmicb.2018.01351
Rivero-Menendez O et al (2019) Clinical and laboratory development of echinocandin resistance in Candida glabrata: molecular characterization. Front Microbiol 10:1585. https://doi.org/10.3389/fmicb.2019.01585
Pristov KE, Ghannoum MA (2019) Resistance of Candida to azoles and echinocandins worldwide. Clin Microbiol Infect 25:792–798. https://doi.org/10.1016/j.cmi.2019.03.028
Fenn JP et al (1994) Comparison of updated Vitek Yeast Biochemical Card and API 20C yeast identification systems. J Clin Microbiol 32:1184–1187. https://doi.org/10.1128/jcm.32.5.1184-1187.1994
Dwivedi M, Muralidhar S, Saluja D (2020) Hibiscus sabdariffa extract inhibits adhesion, biofilm initiation and formation in Candida albicans. Indian J Microbiol 60:96–106. https://doi.org/10.1007/s12088-019-00835-9
Kim H-J, Brehm-Stecher BF (2015) Design and evaluation of peptide nucleic acid probes for specific identification of Candida albicans. J Clin Microbiol 53:511–521. https://doi.org/10.1128/JCM.02417-14
Turhan O et al (2017) Evaluation of MALDI-TOF-MS for the Identification of Yeast Isolates Causing Bloodstream Infection. Clin Lab. https://doi.org/10.7754/Clin.Lab.2016.161101
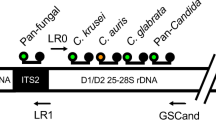
Fidler G, Leiter E, Kocsube S, Biro S, Paholcsek M (2018) Validation of a simplex PCR assay enabling reliable identification of clinically relevant Candida species. BMC Infect Dis 18:393. https://doi.org/10.1186/s12879-018-3283-6
Berenguer J, Buck M, Witebsky F, Stock F, Pizzo PA, Walsh TJ (1993) Lysis—centrifugation blood cultures in the detection of tissue-proven invasive candidiasis disseminated versus single-organ infection. Diagn Microbiol Infect Dis 17:103–109. https://doi.org/10.1016/0732-8893(93)90020-8
Carvalho A et al (2007) Multiplex PCR identification of eight clinically relevant Candida species. Med Mycol 45:619–627. https://doi.org/10.1080/13693780701501787
Katsyv A, Schoelmerich MC, Basen M, Müller V (2021) The pyruvate:ferredoxin oxidoreductase of the thermophilic acetogen, Thermoanaerobacter kivui. FEBS Open Bio 11:1332–1342. https://doi.org/10.1002/2211-5463.13136
Agarwal S, Manchanda V, Verma N, Bhalla P (2011) Yeast identification in routine clinical microbiology laboratory and its clinical relevance. Indian J Med Microbiol 29:172–177. https://doi.org/10.4103/0255-0857.81794
Bayona JVM, García CS, Palop NT, Cardona CG (2020) Evaluation of a novel chromogenic medium for Candida spp. identification and comparison with CHROMagarTM Candida for the detection of Candida auris in surveillance samples. Diagn Microbiol Infect Dis 98:115168. https://doi.org/10.1016/j.diagmicrobio.2020.115168
Monday LM, Acosta TP, Alangaden G (2021) T2Candida for the diagnosis and management of invasive Candida infections. J Fungi 7:178. https://doi.org/10.3390/jof7030178
Himmelreich U et al (2003) Rapid Identification of Candida species by using nuclear magnetic resonance spectroscopy and a statistical classification strategy. Appl Environ Microbiol 69:4566–4574. https://doi.org/10.1128/AEM.69.8.4566-4574.2003
Martínez-Murcia A, Navarro A, Bru G, Chowdhary A, Hagen F, Meis JF (2018) Internal validation of GPS™ MONODOSE CanAur dtec-qPCR kit following the UNE/EN ISO/IEC 17025:2005 for detection of the emerging yeast Candida auris. Mycoses 61:877–884. https://doi.org/10.1111/myc.12834
García-Salazar E et al (2022) Detection and molecular identification of eight candida species in clinical samples by simplex PCR. Microorganisms 10:374. https://doi.org/10.3390/microorganisms10020374
Zhang J, Hung G-C, Nagamine K, Li B, Tsai S, Lo S-C (2016) Development of Candida -specific real-time PCR assays for the detection and identification of eight medically important Candida species. Microbiol Insights 9:MBI.S38517. https://doi.org/10.4137/MBI.S38517
Cooper GR, Nettleton RW (1978) A spread-spectrum technique for high-capacity mobile communications. IEEE Trans Veh Technol 27:264–275. https://doi.org/10.1109/T-VT.1978.23758
Schmidt CM (2004) Pancreaticoduodenectomy. Arch Surg 139:718. https://doi.org/10.1001/archsurg.139.7.718
Alam MZ et al (2014) Candida identification: a journey from conventional to molecular methods in medical mycology. World J Microbiol Biotechnol 30:1437–1451. https://doi.org/10.1007/s11274-013-1574-z
Mohanty SP, Kougianos E (2006) Biosensors: a tutorial review. IEEE Potentials 25:35–40. https://doi.org/10.1109/MP.2006.1649009
Organic thin-film transistors as transducers for (bio) analytical applications. https://link.springer.com/journal/216.
Damborský P, Švitel J, Katrlík J (2016) Optical biosensors. Essays Biochem 60:91–100. https://doi.org/10.1042/EBC20150010
Cooper RM et al (2014) A microdevice for rapid optical detection of magnetically captured rare blood pathogens. Lab Chip 14:182–188. https://doi.org/10.1039/C3LC50935D
Sahin B, Kaya T (2019) Electrochemical amperometric biosensor applications of nanostructured metal oxides: a review. Mater Res Express 6:42003. https://doi.org/10.1088/2053-1591/aafa95
Reyna-Beltrán E, Méndez CIB, Iranzo M, Mormeneo S, Luna-Arias JP (2019) The cell wall of Candida albicans: a proteomics view. In: Candida albicans. IntechOpen. https://doi.org/10.5772/intechopen.82348
Sendid B, Tabouret M, Poirot JL, Mathieu D, Fruit J, Poulain D (1999) New enzyme immunoassays for sensitive detection of circulating Candida albicans Mannan and antimannan antibodies: useful combined test for diagnosis of systemic candidiasis. J Clin Microbiol 37:1510–1517. https://doi.org/10.1128/JCM.37.5.1510-1517.1999
Villamizar RA, Maroto A, Rius FX (2009) Improved detection of Candida albicans with carbon nanotube field-effect transistors. Sens Actuators B Chem 136:451–457. https://doi.org/10.1016/j.snb.2008.10.013
Muramatsu H, Kajiwara K, Tamiya E, Karube I (1986) Piezoelectric immuno sensor for the detection of Candida albicans microbes. Anal Chim Acta 188:257–261. https://doi.org/10.1016/S0003-2670(00)86049-3
Sá SR, Junior AGS, Lima-Neto RG, Andrade CAS, Oliveira MDL (2020) Lectin-based impedimetric biosensor for differentiation of pathogenic candida species. Talanta 220:121375. https://doi.org/10.1016/j.talanta.2020.121375
Kwasny D, Tehrani S, Almeida C, Schjødt I, Dimaki M, Svendsen W (2018) Direct Detection of Candida albicans with a Membrane Based Electrochemical Impedance Spectroscopy Sensor. Sensors 18:2214. https://doi.org/10.3390/s18072214
Yodmongkol S et al (2016) Application of surface plasmon resonance biosensor for the detection of Candida albicans. Jpn J Appl Phys 55:02BE03. https://doi.org/10.7567/JJAP.55.02BE03
Pan Y-L, Yang T-S, Chang T-C, Chang H-C (2009) Rapid identification of Candida albicans based on Raman spectral biosensing technology. In: 2009 IEEE 3rd international conference on nano/molecular medicine and engineering. IEEE, pp 120–124. https://doi.org/10.1109/NANOMED.2009.5559104.
Hassan RYA, El-Attar RO, Hassan HNA, Ahmed MA, Khaled E (2017) Carbon nanotube-based electrochemical biosensors for determination of Candida albicans’s quorum sensing molecule. Sens Actuators B Chem 244:565–570. https://doi.org/10.1016/j.snb.2017.01.028
Pla L et al (2021) Oligonucleotide-capped nanoporous anodic alumina biosensor as diagnostic tool for rapid and accurate detection of Candida auris in clinical samples. Emerg Microbes Infect 10:407–415. https://doi.org/10.1080/22221751.2020.1870411
Metzgar D et al (2013) Broad-spectrum biosensor capable of detecting and identifying diverse bacterial and candida species in blood. J Clin Microbiol 51:2670–2678. https://doi.org/10.1128/JCM.00966-13
Demuyser L, Van Genechten W, Mizuno H, Colombo S, Van Dijck P (2018) Introducing fluorescence resonance energy transfer-based biosensors for the analysis of cAMP-PKA signalling in the fungal pathogen Candida glabrata. Cell Microbiol 20:e12863. https://doi.org/10.1111/cmi.12863
Katrlík J, Holazová A, Medovarská I, Seilerová I, Gemeiner P, Bystrický S (2022) SPR biosensor chip based on mannan isolated from Candida dubliniensis yeasts applied in immunization effectiveness testing. Sens Actuators B Chem 350:130883. https://doi.org/10.1016/j.snb.2021.130883
Akyilmaz E, Dinçkaya E (2005) An amperometric microbial biosensor development based on Candida tropicalis yeast cells for sensitive determination of ethanol. Biosens Bioelectron 20:1263–1269. https://doi.org/10.1016/j.bios.2004.04.010
Wang Y et al (2021) Development and application of a multiple cross displacement amplification combined with nanoparticle-based lateral flow biosensor assay to detect Candida tropicalis. Front Microbiol. https://doi.org/10.3389/fmicb.2021.681488
Akyilmaz E, Guvenc C, Koylu H (2020) A novel mıcrobıal bıosensor system based on C. tropicalis yeast cells for selectıve determınatıon of L-Ascorbıc acid. Bioelectrochemistry 132:107420. https://doi.org/10.1016/j.bioelechem.2019.107420
Dedić J, Kesić A, Hodžić Z, Ibrišimović M, Hadžigrahić N, Mehmedinović NI (2020) Early detection of fungal pathogens in patients with immunodeficiency involving a novel biosensor technology. Int J Dev Res
Cai Z, Luck LA, Punihaole D, Madura JD, Asher SA (2016) Photonic crystal protein hydrogel sensor materials enabled by conformationally induced volume phase transition. Chem Sci 7:4557–4562. https://doi.org/10.1039/C6SC00682E
Asghar W, Sher M, Khan NS, Vyas JM, Demirci U (2019) Microfluidic Chip for Detection of Fungal Infections. ACS Omega 4:7474–7481. https://doi.org/10.1021/acsomega.9b00499
Wang Y et al (2016) Antimicrobial blue light inactivation of gram-negative pathogens in biofilms. In vitro and in vivo studies. J Infect Dis 213:1380–1387. https://doi.org/10.1093/infdis/jiw070
Freire F, Ferraresi C, Jorge AOC, Hamblin MR (2016) Photodynamic therapy of oral Candida infection in a mouse model. J Photochem Photobiol B 159:161–168. https://doi.org/10.1016/j.jphotobiol.2016.03.049
Sukhanova A et al (2002) Highly stable fluorescent nanocrystals as a novel class of labels for immunohistochemical analysis of paraffin-embedded tissue sections. Lab Invest 82:1259–1261. https://doi.org/10.1097/01.LAB.0000027837.13582.E8
Han M, Gao X, Su JZ, Nie S (2001) Quantum-dot-tagged microbeads for multiplexed optical coding of biomolecules. Nat Biotechnol 19:631–635. https://doi.org/10.1038/90228
Li Y, Schluesener HJ, Xu S (2010) Gold nanoparticle-based biosensors. Gold Bull 43:29–41. https://doi.org/10.1007/BF03214964
DeVisser A et al (2011) RETRACTED: Differential impact of diabetes and hypertension in the brain: Adverse effects in grey matter. Neurobiol Dis 44:161–173. https://doi.org/10.1016/j.nbd.2011.06.005
Chatterjee S, Wen J, Chen A (2013) Electrochemical determination of methylglyoxal as a biomarker in humanplasma. Biosens Bioelectron 42:349–354. https://doi.org/10.1016/j.bios.2012.10.091
Zamora-Gálvez A, Morales-Narváez E, Mayorga-Martinez CC, Merkoçi A (2017) Nanomaterials connected to antibodies and molecularly imprinted polymers as bio/receptors for bio/sensor applications. Appl Mater Today 9:387–401. https://doi.org/10.1016/j.apmt.2017.09.006
Singh KR, Nayak V, Sarkar T, Singh RP (2020) Cerium oxide nanoparticles: properties, biosynthesis and biomedical application. RSC Adv 10:27194–27214. https://doi.org/10.1039/D0RA04736H
Chauhan N, Chawla S, Pundir CS, Jain U (2017) An electrochemical sensor for detection of neurotransmitter-acetylcholine using metal nanoparticles, 2D material and conducting polymer modified electrode. Biosens Bioelectron 89:377–383. https://doi.org/10.1016/j.bios.2016.06.047
Costa MP, Andrade CAS, Montenegro RA, Melo FL, Oliveira MDL (2014) Self-assembled monolayers of mercaptobenzoic acid and magnetite nanoparticles as an efficient support for development of tuberculosis genosensor. J Colloid Interface Sci 433:141–148. https://doi.org/10.1016/j.jcis.2014.07.014
Deusenbery C, Wang Y, Shukla A (2021) Recent innovations in bacterial infection detection and treatment. ACS Infect Dis 7:695–720. https://doi.org/10.1021/acsinfecdis.0c00890
Long GL, Winefordner JD (1983) Limit of detection. A closer look at the IUPAC definition. Anal Chem 55:712A-724A. https://doi.org/10.1021/ac00258a001
Sheybani R, Shukla A (2017) Highly sensitive label-free dual sensor array for rapid detection of wound bacteria. Biosens Bioelectron 92:425–433. https://doi.org/10.1016/j.bios.2016.10.084
Wang J, Liu G, Jan MR (2004) Ultrasensitive electrical biosensing of proteins and DNA: carbon-nanotube derived amplification of the recognition and transduction events. J Am Chem Soc 126:3010–3011. https://doi.org/10.1021/ja031723w
Huang G-W, Xiao H-M, Fu S-Y (2015) Wearable electronics of silver-nanowire/poly(dimethylsiloxane) nanocomposite for smart clothing. Sci Rep 5:13971. https://doi.org/10.1038/srep13971
Brolo AG (2012) Plasmonics for future biosensors. Nat Photonics 6:709–713. https://doi.org/10.1038/nphoton.2012.266
Ambhorkar P et al (2018) Nanowire-based biosensors: from growth to applications. Micromachines (Basel) 9:679. https://doi.org/10.3390/mi9120679
Kim W et al (2018) A label-free cellulose SERS biosensor chip with improvement of nanoparticle-enhanced LSPR effects for early diagnosis of subarachnoid hemorrhage-induced complications. Biosens Bioelectron 111:59–65. https://doi.org/10.1016/j.bios.2018.04.003
Nooranian S, Mohammadinejad A, Mohajeri T, Aleyaghoob G, Kazemi-Oskuee R (2022) Biosensors based on aptamer-conjugated gold nanoparticles: a review. Biotechnol Appl Biochem 69:1517–1534. https://doi.org/10.1002/bab.2224
Fei J, Dou W, Zhao G (2015) A sandwich electrochemical immunosensor for Salmonella pullorum and Salmonella gallinarum based on a screen-printed carbon electrode modified with an ionic liquid and electrodeposited gold nanoparticles. Microchim Acta 182:2267–2275. https://doi.org/10.1007/s00604-015-1573-x
Razmi N, Hasanzadeh M, Willander M, Nur O (2020) Recent progress on the electrochemical biosensing of Escherichia coli O157:H7: material and methods overview. Biosensors (Basel) 10:54. https://doi.org/10.3390/bios10050054
Gaba S, Jain U (2024) Advanced biosensors for nanomaterial-based detection of transforming growth factor alpha and beta, a class of major polypeptide regulators. Int J Biol Macromol 257:128622. https://doi.org/10.1016/j.ijbiomac.2023.128622
Gaba S, Chauhan N, Chandra R, Jain U (2024) Future advances of artificial biosensor technology in biomedical applications. Talanta Open. https://doi.org/10.1016/j.talo.2024.100301
Balayan S, Chauhan N, Chandra R, Jain U (2022) Molecular imprinting based electrochemical biosensor for identification of serum amyloid A (SAA), a neonatal sepsis biomarker. Int J Biol Macromol 195:589–597. https://doi.org/10.1016/j.ijbiomac.2021.12.045
Acknowledgements
The authors would like to acknowledge Shodh Grant (UPES/R&D/SHODH/202314) supported by UPES R&D, Dehradun to Nidhi Chauhan and Riya Verma.
Author information
Authors and Affiliations
Contributions
Riya Verma: Writing original draft, Review—writing and editing; Smriti Gaba: Writing original draft, Review—writing and editing, Nidhi Chauhan: Supervision, Review—writing and editing; Ramesh Chandra: Supervision, Review—writing and editing, Utkarsh Jain: Supervision, Conceptualization, Review—writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors Riya Verma and Smriti Gaba are shared co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verma, R., Gaba, S., Chauhan, N. et al. Biodetection Strategies for Selective Identification of Candidiasis. Indian J Microbiol (2024). https://doi.org/10.1007/s12088-024-01288-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12088-024-01288-5