Abstract
Background
The differences in outcomes after aneurysmal subarachnoid hemorrhage (aSAH) between the sexes have not been concretely determined. This study aimed to evaluate the differences in epidemiology, outcomes, and risk factors between male and female patients with aSAH.
Methods
We performed a multicenter, retrospective study of patients with aSAH from 2017 to 2020. We investigated the epidemiological differences between the two sexes. Propensity score matching (PSM) was used to compare short-term outcomes between the sexes. Binary logarithmic regression was performed to investigate the odds ratio (OR) for dependent survival in patients of different sexes.
Results
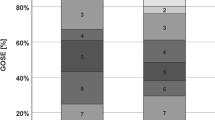
A total of 5,407 consecutive patients with aSAH were included in this study, and the female-to-male ratio was 1.8:1. The peak incidence of aSAH occurred in the 6th and 7th decades in males and females, respectively. There were more female patients with internal carotid artery or posterior communicating artery aneurysms (53.2%), and there were more male patients with anterior cerebral artery or anterior communicating artery aneurysms (43.2%). The incidence of multiple aneurysms was greater in female patients (21.5% vs. 14.2%, P < 0.001). There was no significant difference in outcomes before and after PSM at discharge. The dependent survival risk was related only to the clinical condition on admission in women. In addition, age > 50 years (OR 1.88, 95% confidence interval 1.17–3.02; P = 0.01) and hypertension (OR 1.81, 95% confidence interval 1.25–2.61; P = 0.002) were also risk factors for male patients.
Conclusions
There were more female patients with aneurysms than male patients in this study. Most aneurysm locations were different between the two groups. There was no significant difference in discharge outcomes before and after PSM. The risk factors for dependent survival were different between female and male patients.





Similar content being viewed by others
References
van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet. 2007;369(9558):306–18. https://doi.org/10.1016/S0140-6736(07)60153-6.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354(4):387–96. https://doi.org/10.1056/NEJMra052732.
Fuentes AM, Stone McGuire L, Amin-Hanjani S. Sex differences in cerebral aneurysms and subarachnoid hemorrhage. Stroke. 2022;53(2):624–33. https://doi.org/10.1161/STROKEAHA.121.037147.
de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365–72. https://doi.org/10.1136/jnnp.2007.117655.
Kaminogo M, Yonekura M, Shibata S. Incidence and outcome of multiple intracranial aneurysms in a defined population. Stroke. 2003;34(1):16–21. https://doi.org/10.1161/01.str.0000046763.48330.ad.
Juvela S. Risk factors for multiple intracranial aneurysms. Stroke. 2000;31(2):392–7. https://doi.org/10.1161/01.str.31.2.392.
Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ. Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated meta-analysis. Stroke. 2007;38(4):1404–10. https://doi.org/10.1161/01.STR.0000260955.51401.cd.
Yang Y, Wang B, Ge X, et al. Natural course of ruptured but untreated intracranial aneurysms: a multicenter 2-year follow-up study. Stroke. 2023;54(8):2087–95. https://doi.org/10.1161/strokeaha.123.042530.
Hamdan A, Barnes J, Mitchell P. Subarachnoid hemorrhage and the female sex: analysis of risk factors, aneurysm characteristics, and outcomes. J Neurosurg. 2014;121(6):1367–73. https://doi.org/10.3171/2014.7.JNS132318.
Lindner SH, Bor AS, Rinkel GJ. Differences in risk factors according to the site of intracranial aneurysms. J Neurol Neurosurg Psychiatry. 2010;81(1):116–8. https://doi.org/10.1136/jnnp.2008.163063.
Locksley HB. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg. 1966;25(2):219–39. https://doi.org/10.3171/jns.1966.25.2.0219.
Aarhus M, Helland CA, Wester K. Differences in anatomical distribution, gender, and sidedness between ruptured and unruptured intracranial aneurysms in a defined patient population. Acta Neurochir (Wien). 2009;151(12):1569–74. https://doi.org/10.1007/s00701-009-0316-3.
Molenberg R, Thio CHL, Aalbers MW, et al. Sex hormones and risk of aneurysmal subarachnoid hemorrhage: a Mendelian randomization study. Stroke. 2022;53(9):2870–5. https://doi.org/10.1161/STROKEAHA.121.038035.
McDowell MM, Zhao Y, Kellner CP, et al. Demographic and clinical predictors of multiple intracranial aneurysms in patients with subarachnoid hemorrhage. J Neurosurg. 2018;128(4):961–8. https://doi.org/10.3171/2017.1.JNS162785.
Horikoshi T, Akiyama I, Yamagata Z, Sugita M, Nukui H. Magnetic resonance angiographic evidence of sex-linked variations in the circle of willis and the occurrence of cerebral aneurysms. J Neurosurg. 2002;96(4):697–703. https://doi.org/10.3171/jns.2002.96.4.0697.
Lindekleiv HM, Valen-Sendstad K, Morgan MK, et al. Sex differences in intracranial arterial bifurcations. Gend Med. 2010;7(2):149–55. https://doi.org/10.1016/j.genm.2010.03.003.
Schupper AJ, Hardigan TA, Mehta A, et al. Sex and racial disparity in outcome of aneurysmal subarachnoid hemorrhage in the United States: a 20-year analysis. Stroke. 2023;54(5):1347–56. https://doi.org/10.1161/strokeaha.122.041488.
Turan N, Heider RA, Zaharieva D, Ahmad FU, Barrow DL, Pradilla G. Sex differences in the formation of intracranial aneurysms and incidence and outcome of subarachnoid hemorrhage: review of experimental and human studies. Transl Stroke Res. 2016;7(1):12–9. https://doi.org/10.1007/s12975-015-0434-6.
Acosta JN, Szejko N, Both CP, et al. Genetically determined smoking behavior and risk of nontraumatic subarachnoid hemorrhage. Stroke. 2021;52(2):582–7. https://doi.org/10.1161/strokeaha.120.031622.
Pegoli M, Mandrekar J, Rabinstein AA, Lanzino G. Predictors of excellent functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2015;122(2):414–8. https://doi.org/10.3171/2014.10.JNS14290.
Jabbarli R, Reinhard M, Roelz R, et al. Early identification of individuals at high risk for cerebral infarction after aneurysmal subarachnoid hemorrhage: the BEHAVIOR score. J Cereb Blood Flow Metab. 2015;35(10):1587–92. https://doi.org/10.1038/jcbfm.2015.81.
Larrew T, Pryor W 3rd, Weinberg J, et al. Aneurysmal subarachnoid hemorrhage: a statewide assessment of outcome based on risk factors, aneurysm characteristics, and geo-demography. J Neurointerv Surg. 2015;7(11):855–60. https://doi.org/10.1136/neurintsurg-2014-011359.
Galea JP, Dulhanty L, Patel HC, UK, Ireland Subarachnoid Hemorrhage Database C. Predictors of outcome in aneurysmal subarachnoid hemorrhage patients: observations from a multicenter data set. Stroke. 2017;48(11):2958–63. https://doi.org/10.1161/STROKEAHA.117.017777.
Rosenlrn J, Eskesen V, Schmidt K. Clinical features and outcome in females and males with ruptured intracranial saccular aneurysms. Br J Neurosurg. 1993;7(3):287–90. https://doi.org/10.3109/02688699309023811.
Tam AK, Ilodigwe D, Mocco J, et al. Impact of systemic inflammatory response syndrome on vasospasm, cerebral infarction, and outcome after subarachnoid hemorrhage: exploratory analysis of CONSCIOUS-1 database. Neurocrit Care. 2010;13(2):182–9. https://doi.org/10.1007/s12028-010-9402-x.
Lambert G, Naredi S, Eden E, Rydenhag B, Friberg P. Monoamine metabolism and sympathetic nervous activation following subarachnoid haemorrhage: influence of gender and hydrocephalus. Brain Res Bull. 2002;58(1):77–82. https://doi.org/10.1016/s0361-9230(02)00762-1.
Dasenbrock HH, Rudy RF, Rosalind Lai PM, et al. Cigarette smoking and outcomes after aneurysmal subarachnoid hemorrhage: a nationwide analysis. J Neurosurg. 2018;129(2):446–57. https://doi.org/10.3171/2016.10.JNS16748.
Bögli SY, Utebay D, Smits N, et al. Sex-related differences of invasive therapy in patients with aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien). 2022;164(11):2899–908. https://doi.org/10.1007/s00701-022-05345-0.
Hammer A, Steiner A, Ranaie G, et al. Impact of comorbidities and smoking on the outcome in aneurysmal subarachnoid hemorrhage. Sci Rep. 2018;8(1):12335. https://doi.org/10.1038/s41598-018-30878-9.
Slettebø H, Karic T, Sorteberg A. Impact of smoking on course and outcome of aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien). 2020;162(12):3117–28. https://doi.org/10.1007/s00701-020-04506-3.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A. Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke. 1994;25(7):1342–7. https://doi.org/10.1161/01.str.25.7.1342.
Hawkins RI. Smoking, platelets and thrombosis. Nature. 1972;236(5348):450–2. https://doi.org/10.1038/236450a0.
Lasner TM, Weil RJ, Riina HA, et al. Cigarette smoking-induced increase in the risk of symptomatic vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg. 1997;87(3):381–4. https://doi.org/10.3171/jns.1997.87.3.0381.
Weir BK, Kongable GL, Kassell NF, Schultz JR, Truskowski LL, Sigrest A. Cigarette smoking as a cause of aneurysmal subarachnoid hemorrhage and risk for vasospasm: a report of the Cooperative Aneurysm Study. J Neurosurg. 1998;89(3):405–11. https://doi.org/10.3171/jns.1998.89.3.0405.
Pobereskin LH. Influence of premorbid factors on survival following subarachnoid hemorrhage. J Neurosurg. 2001;95(4):555–9. https://doi.org/10.3171/jns.2001.95.4.0555.
Carandang RA, Barton B, Rordorf GA, Ogilvy CS, Sims JR. Nicotine replacement therapy after subarachnoid hemorrhage is not associated with increased vasospasm. Stroke. 2011;42(11):3080–6. https://doi.org/10.1161/STROKEAHA.111.620955.
Seder DB, Schmidt JM, Badjatia N, et al. Transdermal nicotine replacement therapy in cigarette smokers with acute subarachnoid hemorrhage. Neurocrit Care. 2011;14(1):77–83. https://doi.org/10.1007/s12028-010-9456-9.
Funding
This work was supported by the Tianjin Medical University General Hospital Clinical Research Program (Grant No. 22ZYYLCCG07) and the Natural Science Foundation of Tianjin, China (Grant No. 20JCZDJC00300).
Author information
Authors and Affiliations
Contributions
Manuscript writing: Chao Peng, Yan Zhao and Fan Li; Data collection: Chao Peng, Yan Zhao, Fan Li, Tie-zhu Guo, Xiang-dong Wang, and Bang-yue Wang; Data analysis: Chao Peng, Yan Zhao, Fan Li, Heng-rui Zhang, Yi-fan Yang, Qing-guo Liu and Xin-liang Ren; Study conception and design: Xin-yu Yang; Manuscript editing: Xin-yu Yang, Qing-guo Liu and Xin-liang Ren; Funding acquisition: Xin-yu Yang; Supervision: Xin-yu Yang. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethical Approval/Informed Consent
This study protocol was examined and approved by the Medical Ethics Committee of Tianjin Medical University General Hospital (No. IRB2022-YX-175-01).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peng, C., Zhao, Y., Li, F. et al. Aneurysmal Subarachnoid Hemorrhage and Sex Differences: Analysis of Epidemiology, Outcomes, and Risk Factors. Neurocrit Care (2024). https://doi.org/10.1007/s12028-023-01929-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01929-5