Abstract
Introduction
Neuromonitoring represents a cornerstone in the comprehensive management of patients with traumatic brain injury (TBI), allowing for early detection of complications such as increased intracranial pressure (ICP) [1]. This has led to a search for noninvasive modalities that are reliable and deployable at bedside. Among these, ultrasonographic optic nerve sheath diameter (ONSD) measurement is a strong contender, estimating ICP by quantifying the distension of the optic nerve at higher ICP values. Thus, this scoping review seeks to describe the existing evidence for the use of ONSD in estimating ICP in adult TBI patients as compared to gold-standard invasive methods.
Materials and Methods
This review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews, with a main search of PubMed and EMBASE. The search was limited to studies of adult patients with TBI published in any language between 2012 and 2022. Sixteen studies were included for analysis, with all studies conducted in high-income countries.
Results
All of the studies reviewed measured ONSD using the same probe frequency. In most studies, the marker position for ONSD measurement was initially 3 mm behind the globe, retina, or papilla. A few studies utilized additional parameters such as the ONSD/ETD (eyeball transverse diameter) ratio or ODE (optic disc elevation), which also exhibit high sensitivity and reliability.
Conclusion
Overall, ONSD exhibits great test accuracy and has a strong, almost linear correlation with invasive methods. Thus, ONSD should be considered one of the most effective noninvasive techniques for ICP estimation in TBI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuromonitoring is essential for the management of patients with traumatic brain injury (TBI), allowing early detection of potential insults such as increased intracranial pressure (ICP), which may precipitate a cascade of events (from ischemia to brain herniation) that warrant proper and timely treatment [1,2,3]. Thus, efficient, reliable, and widely available tools for such ICP monitoring are also equally essential. Currently, the gold standard for neuromonitoring consists of intraventricular and intraparenchymal transducers; however, these techniques are costly and require skilled personnel. As a consequence, these techniques are usually restricted to high-level centers [4, 5]. Invasive devices are also generally contraindicated in patients with bleeding disorders while also carrying the risk of infection and malfunction [6,7,8,9]. This has led to a search for noninvasive modalities for ICP monitoring that are inexpensive, reliable, reproducible, and tailored for point-of-care applications [10, 11]. Different methods are described in the literature for noninvasive ICP (nICP) estimation, which include, but are not limited to, optic nerve sheath diameter (ONSD) measurement as assessed by ultrasound, computerized tomography or magnetic resonance imaging [12, 13], transcranial Doppler-derived indices (e.g., pulsatility index and flow velocities) [14], and the measurement of pupil size and other dynamic pupillary variables (Neurologic Pupillary Index, NPi, latency, constriction velocity, and dilation velocity) [15]. The goal of this work is to characterize the evidence concerning exclusively ONSD abilities to estimate nICP in adult patients with TBI.
Review Questions
The objective of this scoping review is to describe the extent and type of evidence for nICP monitoring in TBI using ONSD, as compared with standard invasive methods in the adult population. Applying the Patient, Concept, Context (PCC) framework, the following specific questions were formulated:
-
1.
Which methods are available for nICP monitoring using ultrasound-measured ONSD?
-
2.
What evidence exists for the association and accuracy of nICP monitoring using ultrasound-measured ONSD versus invasive monitoring for ICP estimation?
Methods
This scoping review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews.
Inclusion Criteria
Participants
This scoping review considered studies including patients over 18 years old suffering from TBI who underwent nICP monitoring using ONSD and required diagnostic invasive ICP (ICPi) monitoring for ICP estimation. All studies in the pediatric population (defined here as < 18 years) were excluded.
Concept
The concept of this scoping review was to include studies that investigated nICP monitoring by ONSD in adult patients with all degrees of TBI (mild, moderate, and severe) as compared with the analysis derived from gold-standard invasive methods. Topics in this concept include, but are not limited to, device features, methodological details, variables derived from said methods, the diagnostic accuracy of each method in detecting intracranial hypertension, the reliability of these methods, and the sensitivity and specificity of a specific ONSD method in the diagnosis of intracranial hypertension.
Context
This scoping review did not consider the specific race, gender, or geographic location of participants in the selected studies. Given that the anatomy and pathophysiology of TBI within the pediatric population differ substantially from those of their adult counterparts, especially in the mid and lower age ranges (e.g., < 14 years and > 50 years), and because of the large amount of literature that consider “adults” by a cutoff of 18 years, exclusion was determined solely by participant age, with only studies conducted in adults > 18 years being included.
Types of Sources
The present scoping review assessed both experimental and quasi-experimental study designs including randomized controlled trials, nonrandomized controlled trials, before-and-after studies, and interrupted time-series studies. In addition, analytical observational studies including prospective and retrospective cohort studies, case–control studies, and analytical cross-sectional studies were considered for inclusion. This review also considered descriptive observational study designs including case series, individual case reports, and descriptive cross-sectional studies for inclusion. Qualitative studies that focus on qualitative data were also considered, including but not limited to, designs such as phenomenology, grounded theory, ethnography, qualitative description, action research, and feminist research. In addition, systematic reviews that met the inclusion criteria were also considered, depending on the research question.
Search Strategy
An initial search in EMBASE and PubMed was undertaken, aimed at locating published studies in the adult population between January 2012 and June 2022 so as to obtain the most updated evidence and technological advances on the subject and because, specifically from 2012, the results by year in the two employed databases (exhibited in bar charts in their websites) showed an important increase in the publication of studies in the topic. Additionally, studies published in any language were included, as the available and useful literature was in a variety of languages. Studies that contained noninvasive monitoring with techniques other than ONSD were excluded. Studies containing ICPi or nICP monitoring for the diagnosis of intracranial hypertension from etiologies other than TBI were also excluded. We also exclude narrative reviews in the topic because, although in general they are comprehensive in the information that they provide, they are influenced subjectively by the authors and may have outdated sources. A detailed search strategy for both databases is contained in online Appendix 1.
Source of Evidence Screening/Selection
The initial EMBASE and PubMed search yielded 106 studies. All identified citations were collated and uploaded into Covidence, and one duplicated study was removed. Studies were screened by two independent researchers (KM and SV) and one collaborator (OF). After examining 105 titles and abstracts for inclusion, 74 irrelevant studies were removed, 31 full-text studies were assessed for eligibility, and 15 studies were excluded for reasons described in Fig. 1. The results of the search are reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist [16].
Results
After reviewing and applying inclusion and exclusion criteria, 16 studies were included for final analysis. We did not find any qualitative study with designs such as phenomenology, grounded theory, ethnography, qualitative description, action research, and feminist research. Figure 2 provides the characteristics of the included publications. Table 1 provides the extracted information based upon the formulated research questions.
Methods for nICP Monitoring Using Ultrasound-Measured ONSD
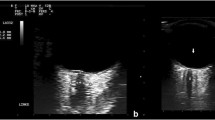
After reviewing in detail each of the studies included, the reported technical settings were identical in terms of probe frequency (a 7.5 MHz linear probe), with the exception of three studies that mentioned a range of frequencies rather than any single one [17,18,19].
Regarding the position of the ONSD measurement, all studies reported an initial measurement 3 mm behind the globe, retina, or papilla, whereas one study measured 2.8 mm behind the globe, and another in a range of 3–4 mm [20, 21]. Probe orientation for ONSD ultrasound was mentioned in four studies (Table 1). In three studies, the orientation was axial only [1, 21, 22]. In one, orientation was both axial and sagittal [23]. In the previous study and one other, a description of patient positioning during the ultrasound study (head of bed at 30°) was made [23, 24].
Regarding the method of estimating the final ONSD measurement, ten studies reported how they obtained the final value in mm (Table 1). Some considered an average of four values (one axial and one sagittal measurement for each eye) [23, 25] while some used an average of three values [19, 26, 27] or an average of two values [17, 20, 21, 28, 29]. The remaining included studies did not mention any details regarding the methods for obtaining the final ONSD measurement [18, 22, 24, 30,31,32].
Besides isolated ONSD measurements for ICP estimation of correlation with ICPi, three studies assessed parameters apart from ONSD that leveraged ultrasonography such as eyeball transverse diameter (ETD) [26], ONSD/ETD ratio [19], and optic disk elevation (ODE) (estimated by measuring the maximum height of the optic disk above the retina) [3]. One study even went as far as to propose a formula-based nICP estimation based on ONSD values as follows [25]:
Uniquely, one of these studies assessed three different ONSD measurements: the proper optic nerve (ON) diameter (between the pia mater), the measured distance between the external borders of the hypoechogenic leptomeninges or dura mater (ONSDI), and the ONSD including the subarachnoid space (SAS), defined as the subarachnoid diameter (ONSDE) [19]. Each method description along with its associated variables is summarized in Table 1.
nICP by ONSD Versus ICPi Monitoring for ICP Estimation
Of the studies analyzed, only five did not mention a calculated correlation between ONSD and ICPi [21, 22, 24, 28, 30]. All studies except for two considered “elevated intracranial pressure” as greater than or equal to 20 mm Hg [18, 27]. Two studies specifically used the term “intracranial hypertension” to refer to values above this threshold (Table 1) [23, 25]. On the other hand, four studies assessed different ICP thresholds and estimated their corresponding ONSD threshold values (Table 1): Launey et al. reported ICPi values of 20 mm Hg, 25 mm Hg, and 30 mm Hg, Soliman et al. reported values of 20 mm Hg and 25 mm Hg, Wang et al. of 13 mm Hg and 22 mm Hg, and Agrawal et al. of 22 mm Hg and 25 mm Hg [18, 20, 27, 29].
Regarding the ICPi monitoring technique, the vast majority of studies considered either intraparenchymal techniques, intraventricular techniques, or both, and only three studies did not mention the type of ICPi method employed (Table 1) [21, 28, 30]. None of the analyzed studies made any specifications about the side of injury or type of injury (e.g., contusion vs. subdural hematoma) with respect to ICPi and nICP estimation or about the site of ICP probe placement in relation to the side of ONSD measurement. All the studies were performed in high-income countries (Fig. 2).
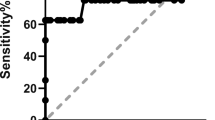
In a prospective cohort study of 27 patients with TBI, ONSD accurately predicted ICPi greater than 20 mm Hg with a sensitivity of 83.3% (95% Confidence Interval CI [35.9%, 99.6%]) and a specificity of 100% (95% CI [83.9%, 100%]). The positive predictive value of an ONSD value greater than or equal to 5.2 mm was 100% (95% CI [48%,100%]), and the negative predictive value of ONSD less than 5.2 mm was 95.5% (95% CI [77.2%, 99.9%]) (Table 1). The receiver operating characteristic curve demonstrated an area under the curve of 0.865 [17].
In a diagnostic test accuracy study performed in 120 patients with TBI, both ONSD and ODE were analyzed. The optimal ONSD threshold for detecting ICPi greater than 25 mm Hg was 7.2 mm, with a sensitivity of 83% (95% CI [36, 100%]) and a specificity of 76% (95% CI [67%, 84%]). Notably, a cutoff of 7.2 mm similarly detected ICPi greater than 22 mm Hg and less than 25 mm Hg at the expense of a slight decrease in sensitivity and increase in specificity to 82% (95% CI [48%, 98%]) and 79% (95% CI [70%, 86%]), respectively. Meanwhile, ODE showed an optimal threshold of greater than 0.04 cm to detect an ICPi greater than 22 mm Hg, with a sensitivity of 90% (95% CI [56%, 100%]) and a specificity of 71% (95% CI [61%, 79%]) (Table 1) [18].
A prospective cohort study in 50 patients calculated variables apart from ONSD including ONSDI, ONSDE, and ETD for the ONSD/ETD ratio (Table 1). The values for ONSDE, ONSDI, and ONSD/ETD ratio were significantly associated with ICP (p = 0.005, p < 0.001, and p < 0.001, respectively). The greatest association with ICPi was with ONSD (r = 0.511) and ONSD/ETD ratio (r = 0.59) The cutoff values in terms of ONSD/ETD, ONSDI, and ONSDE for an ICPi of greater than or equal to 20 mm Hg were 0.264, 6.15, and 5.05, respectively [19].
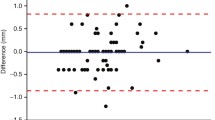
A cohort study performed in 73 patients that correlated maximum, minimum, and standard deviation values for both ONSD and ICPi found a good correlation between the two modalities (r = 0.8717, p < 0.0001) in the setting of TBI [24].
A prospective cohort study performed in 40 patients using two ICPi cutoff values (20 and 25 mm Hg), found a strong correlation between ONSD values and invasive monitoring (r = 0.74, p < 0.0001), with an ONSD cutoff value of 6.4 mm for an ICPi of 20 mm Hg and of 6.6 mm for an ICPi of 25 mm Hg. Sensitivity and specificity were both more than 80% (Table 1) [20].
In a prospective cohort study of 20 patients with TBI, an ONSD greater than 5.55 mm was shown to have a sensitivity of 81.8% and a specificity of 88.9% for prediction of ICP increases (Area Under Curve 0.919; 95% CI [0.798,1.0], p < 0.002). The median ICPi value was 22.75 mm Hg, with no head-to-head value comparison between ONSD in mm versus ICP in mm Hg [21].
In another cohort study in 11 patients with TBI, a linear relationship between ONSD and ICPi was documented when a specific ICP-lowering treatment was applied, with an average posttreatment decrease in ONSD of 0.62 mm (p = 0.0001) and an average posttreatment decrease in ICPi of 3.33 mm Hg (p = 0.0001). Correlations were similar in the pretreatment stage (Table 1) [22].
Another prospective cohort study in 100 patients (30 with TBI) found a significant, moderate correlation between ICPi and ONSD (r = 0.53, p 0.002), with an ONSD cutoff value greater than 5.3 mm predictive of intracranial hypertension (ICPi > 20 mm Hg). This cutoff value was associated with a sensitivity of 67% and a specificity of 73% [23].
In a cohort study assessing ONSD and another ultrasound-estimated measurement, the ETD, in 52 patients, better accuracy was observed for the ONSD/ETD ratio over ONSD in isolation. An ONSD/ETD cutoff value was set at 0.25 (sensitivity of 90%, specificity of 82.3%), and an ONSD cutoff value was set at 5.53 mm (sensitivity of 80%, specificity of 79.3%) [26].
A Chinese case–control study with a total sample size of 75 (35 patients with TBI, 40 healthy controls), showed a significant correlation between ONSD and ICPi (r = 0.771, p < 0.0001). Here, the cutoff value for detecting ICP above 13 mm Hg was defined as 5.48 mm, with sensitivity and specificity of 91.1% and 88.0%, respectively. Similarly, the cutoff value for detecting ICP above 22 mm Hg was 5.83 mm, with sensitivity and specificity of 94.4% and 81.0%, respectively (Table 1) [27].
In a systematic review of four studies in patients with TBI, the sensitivity and specificity were 91% and 82% for sonographic ONSD in the prediction of intracranial hypertension [28].
A prospective cohort study in 135 patients (66 with TBI) in the United States described both a weak-moderate correlation (r = 0.498, p = 0.292) between ONSD and ICPi values. However, no data regarding other specific values nor a ICPi estimation method were specified [30].
A systematic review of 12 studies concluded that ultrasound ONSD measurements less than 5 mm could be considered “normal ICP,” whereas measurements greater than 6 mm represented an elevated ICP (ICP > 20 mm Hg). This ICP cutoff was considered accurate for assessing “ICP crisis,” with sensitivity and specificity approaching 90% and 85%, respectively [31].
Lastly, in a French study of 54 patients with TBI, an ONSD cutoff value of 5.6 mm had a sensitivity and negative predictive value of 100% for detecting ICPi greater than 20 mm Hg, with an area under the curve of 0.73 (95% CI [0.59–0.86]) [33].
Discussion
According to the information extracted from the reviewed studies and their reported results, ONSD seems to have a great accuracy and good correlation with ICPi, both in isolated absolute values and in incremental or decremental changes. The relationship between ONSD and ICPi values is almost linear. Nevertheless, OSND is more useful in detecting high ICP than in identifying normal ICP, which is clinically useful given that undetected ICP elevation often leads to detrimental consequences in patients with TBI, whereas low or normal ICP is usually less concerning.
The theoretical principles of ONSD ultrasound measurements as an indirect estimation of ICP depend on an extensive number of pathophysiological phenomena, which are mainly related to cerebrospinal fluid (CSF) dynamics and ICP transmission to the space surrounding the ON [34]. Strictly speaking, the ON is not a nerve by histological terms, but instead a central nervous system (CNS) white matter tract that extends into the orbit, where it is surrounded by CSF throughout its entire length. Given this particular anatomical configuration, the ON is sensitive to ICP changes in its surrounding layers. The dura mater and, to a lesser extent, the arachnoid, allow the circulation and storage of CSF due to their ability to physically expand [35]. There are several theories regarding CSF dynamics as a whole that, in specific CNS areas such as the ON, take into account the role of other parameters in CSF dynamics, such as physics per se [36, 37], bridging veins and sagittal sinus pressures [38], and the rate of CSF production and drainage (via arachnoid villi and the glymphatic system) [34, 37], among others. However, there is no single unified theory that comprises and integrates all of these phenomena, and some deserve to be mentioned specifically with respect to the ON and ONSD.
Free, bidirectional communication between the intracranial SAS and the ON SAS (optic nerve subarachnoidal space) has been proposed in an attempt to define how the cranial CSF that enters the SAS of the ON could change its direction of flow against the volume gradient that directs it from the higher volume site of production (in the intracranial space) toward the SAS of the ON [35]. Two outflow routes have been proposed. The first is from the SAS of the distal portion of the ON, and the second via the glymphatic system [34, 35]. Thus, for now, we can speculate that a certain amount of CSF is already circulating around the ON in the SAS at baseline and that “extra fluid” (in the setting of TBI and other CNS diseases) in fact represents CSF redistribution as a compensatory mechanism in early-stage and mid-stage of ICP increases. This excess fluid occupies the SAS and leads to ONSD distention detected by ultrasound. Other possibly related mechanisms, such as impaired exchange between intracranial CSF and ON SAS, described in other diseases have not yet been considered in TBI, given the different disease processes and underlying pathophysiology [39]. As such, ONSD estimation indeed represents a noninvasive way of detecting ICP changes by assessing, from a CSF-dynamics point-of-view, early “buffering mechanisms” in cases of intracranial compliance compromise [40].
With respect to the sonographic techniques for ONSD evaluation and assessment of other similar parameters described in the analyzed studies, the information extracted was generally highly variable in terms of the probe’s plane of orientation/insonation [25, 41], patient positioning [23, 24], anatomical landmarks for ONSD measurement [19], and final ONSD measurement calculation methods (Table 1). It is worth mentioning that there were three additional proposed methods apart from ONSD for nICP estimation: ODE [18], ONSD/ETD ratio [19], and a formula-based method leveraging calculated ONSD values (Table 1) [25]. Some of these methods demonstrated better correlation with ICPi and even greater sensitivity and specificity than ONSD alone [18, 19]. Such methods may represent an attempt to individualize ONSD measurements by taking into account eyeball size and its relation to ONSD for each patient [19]; however, there are also recently published data that contrarily report no correlation between global size and ONSD in a healthy Latin American population, creating possible uncertainties regarding the usefulness of these techniques for nICP assessment [42]. On the other hand, these methods may constitute a sonographic assessment of optic disk changes, which may be detected earlier than changes in routine fundoscopy, specifically papilledema [18, 43]. Thus, specifically, the formula-based method proposed by Robba et al. may have a great potential for nICP estimation, although it must be validated in further studies before any considerations regarding its efficacy and accuracy for this purpose can be made (Table 1) [25]. Given the huge differences in the described methods for ONSD ultrasound estimation among all studies, there is undoubtedly a need for establishment of a formal protocol that considers the aforementioned parameters, includes details that may not be as obvious (such as the position of the patient’s gaze during measurement), and can be applied across different regions of the world. Currently, there are emerging data that could represent important starting points, such as anatomical landmark identification and a quality checklist [44, 45].
Overall, ONSD correlations with ICPi were moderate to high in the reviewed studies (Table 1), with all of them reporting ONSD values greater than 5 mm corresponding with elevated ICP values (> 20 mm Hg). However, the highest sensitivity, specificity, predictive ability for high ICP values [23] and diagnostic accuracy [18] were seen with values greater than or equal to 5.85 mm. This effect was even more pronounced for values exceeding 6 mm, in line with concomitant ICP increases. Specific data for different ICP thresholds were given by Launey et al. and Soliman et al. (Table 1) [20, 29]. In the near future, we need more studies that consider standardized ultrasound techniques for ONSD measurement based on criteria for quality, definitions of intracranial hypertension (based on physiology rather than simple ICP values), decompressive craniectomy-induced changes in ONSD estimations, ONSD correlations with ICP properties (e.g., waveform trends), and site-of-injury descriptions to help identify compartmentalized vs. diffuse ICP changes.
Limitations
This review, as their first and third counterparts, has multiple limitations. First, only studies in patients 18 years or older were included, potentially leaving out valuable information from patients 16 years and older who are also considered part of the “adult population.” Second, as a matter of a scoping review design, in-depth statistical analyses or risk-of-bias assessments that are usually performed in systematic reviews were not done in our study. This may represent a weakness for data interpretation in terms of diagnostic accuracy and nICP-ICPi correlation comparison between studies. Third, studies that assessed other ICPi monitoring techniques (e.g., opening pressure by lumbar puncture) were not included in our review, given that intraventricular/intraparenchymal catheters are still considered the gold standard. This is a potential loss of valuable additional information. Notwithstanding, we agree that this paper can be seen as complementary to the aforementioned work by Aletreby et al. regarding ONSD for nICP monitoring [46]. Finally, we only included studies in patients with TBI. As such, the analyses and conclusions derived from this work cannot be extrapolated to other neurocritical care patient populations (e.g., aSAH, ischemic stroke, or intracerebral hemorrhage).
Conclusions
This review can be considered an update acknowledging ONSD as possibly (when properly done), one of the most practical, fast, and reliable methods for nICP monitoring in patients with TBI. ONSD cutoffs that correlate with ICPi values were provided, although it must be underscored that these still cannot be considered a replacement for invasive techniques. ONSD seems to be promising for bedside identification of patients with high degrees of neurological deterioration secondary to intracranial hypertension.
References
Evensen KB, Eide PK. Measuring intracranial pressure by invasive, less invasive or non-invasive means: limitations and avenues for improvement. Fluids Barriers CNS. 2020;17(1):34. https://doi.org/10.1186/s12987-020-00195-3.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1). https://doi.org/10.1227/NEU.0000000000001432.
Vik A, Nag T, Fredriksli OA, et al. Relationship of “dose” of intracranial hypertension to outcome in severe traumatic brain injury. J Neurosurg. 2008;109(4):678–84. https://doi.org/10.3171/JNS/2008/109/10/0678.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367(26):2471–81. https://doi.org/10.1056/NEJMoa1207363.
Robba C, Graziano F, Rebora P, et al. Intracranial pressure monitoring in patients with acute brain injury in the intensive care unit (SYNAPSE-ICU): an international, prospective observational cohort study. Lancet Neurol. 2021;20(7):548–58. https://doi.org/10.1016/S1474-4422(21)00138-1.
Czosnyka M, Pickard JD. Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry. 2004;75(6):813–21. https://doi.org/10.1136/jnnp.2003.033126.
Hawthorne C, Piper I. Monitoring of intracranial pressure in patients with traumatic brain injury. Front Neurol. 2014;5:121. https://doi.org/10.3389/fneur.2014.00121.
Feng J, Yang C, Jiang J. Real-world appraisal of intracranial pressure monitoring. Lancet Neurol. 2021;20(7):502–3. https://doi.org/10.1016/S1474-4422(21)00164-2.
Tavakoli S, Peitz G, Ares W, et al. Complications of invasive intracranial pressure monitoring devices in neurocritical care. Neurosurg Focus. 2017;43(5):E6. https://doi.org/10.3171/2017.8.FOCUS17450.
Wang LJ, Chen LM, Chen Y, et al. Ultrasonography assessments of optic nerve sheath diameter as a noninvasive and dynamic method of detecting changes in intracranial pressure. JAMA Ophthalmol. 2018;136(3):250–6. https://doi.org/10.1001/jamaophthalmol.2017.6560.
Vitiello L, Salerno G, De Bernardo M, et al. Ultrasound detection of intracranial hypertension in brain injuries. Front Med (Lausanne). 2022;9:870808. https://doi.org/10.3389/fmed.2022.870808.
Raval R, Shen J, Lau D, et al. Comparison of three point-of-care ultrasound views and MRI measurements for optic nerve sheath diameter: a prospective validity study. Neurocrit Care. 2020;33(1):173–81. https://doi.org/10.1007/s12028-019-00881-7.
Sekhon MS, Griesdale DE, Robba C, et al. Optic nerve sheath diameter on computed tomography is correlated with simultaneously measured intracranial pressure in patients with severe traumatic brain injury. Intensive Care Med. 2014;40(9):1267–74. https://doi.org/10.1007/s00134-014-3392-7.
Cardim D, Robba C, Bohdanowicz M, et al. Non-invasive monitoring of intracranial pressure using transcranial doppler ultrasonography: is it possible? Neurocrit Care. 2016;25(3):473–91. https://doi.org/10.1007/s12028-016-0258-6.
Chen JW, Gombart ZJ, Rogers S, et al. Pupillary reactivity as an early indicator of increased intracranial pressure: the introduction of the neurological pupil index. Surg Neurol Int. 2011;2:82. https://doi.org/10.4103/2152-7806.82248.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Frumin E, Schlang J, Wiechmann W, et al. Prospective analysis of single operator sonographic optic nerve sheath diameter measurement for diagnosis of elevated intracranial pressure. West J Emerg Med. 2014;15(2):217–20. https://doi.org/10.5811/westjem.2013.9.16191.
Agrawal D, Raghavendran K, Zhao L, et al. A prospective study of optic nerve ultrasound for the detection of elevated intracranial pressure in severe traumatic brain injury. Crit Care Med. 2020;48(12):e1278–85. https://doi.org/10.1097/CCM.0000000000004689.
Youm JY, Lee JH, Park HS. Comparison of transorbital ultrasound measurements to predict intracranial pressure in brain-injured patients requiring external ventricular drainage. J Neurosurg. 2022;136(1):257–63. https://doi.org/10.3171/2021.1.JNS204218.
Soliman I, Johnson GGRJ, Gillman LM, et al. New optic nerve sonography quality criteria in the diagnostic evaluation of traumatic brain injury. Crit Care Res Pract. 2018;2018:3589762. https://doi.org/10.1155/2018/3589762.
Wang Y, Yuan Z, Zhang Z, et al. Lateral ventricular volume asymmetry and optic nerve sheath diameter predict intracranial pressure in traumatic brain injury patients. Appl Bionics Biomech. 2022;2022:9808334. https://doi.org/10.1155/2022/9808334.
Kashyap S, Brazdzionis J, Savla P, et al. Osteopathic manipulative treatment to optimize the glymphatic environment in severe traumatic brain injury measured with optic nerve sheath diameter, intracranial pressure monitoring, and neurological pupil index. Cureus. 2021;13(3):e13823. https://doi.org/10.7759/cureus.13823.
Robba C, Pozzebon S, Moro B, et al. Multimodal non-invasive assessment of intracranial hypertension: an observational study. Crit Care. 2020;24(1):379. https://doi.org/10.1186/s13054-020-03105-z.
Zhou J, Li J, Ye T, et al. Ultrasound measurements versus invasive intracranial pressure measurement method in patients with brain injury: a retrospective study. BMC Med Imaging. 2019;19(1):53. https://doi.org/10.1186/s12880-019-0354-0.
Robba C, Cardim D, Tajsic T, et al. Ultrasound non-invasive measurement of intracranial pressure in neurointensive care: a prospective observational study. PLoS Med. 2017;14(7):e1002356. https://doi.org/10.1371/journal.pmed.1002356.
Du J, Deng Y, Li H, et al. Ratio of optic nerve sheath diameter to eyeball transverse diameter by ultrasound can predict intracranial hypertension in traumatic brain injury patients: a prospective study. Neurocrit Care. 2020;32(2):478–85. https://doi.org/10.1007/s12028-019-00762-z.
Wang J, Li K, Li H, et al. Ultrasonographic optic nerve sheath diameter correlation with ICP and accuracy as a tool for noninvasive surrogate ICP measurement in patients with decompressive craniotomy. J Neurosurg. 2019;19:1–7. https://doi.org/10.3171/2019.4.JNS183297.
Lee SH, Kim HS, Yun SJ. Optic nerve sheath diameter measurement for predicting raised intracranial pressure in adult patients with severe traumatic brain injury: a meta-analysis. J Crit Care. 2020;56:182–7. https://doi.org/10.1016/j.jcrc.2020.01.006.
Launey Y, Nesseler N, Le Maguet P, et al. Effect of osmotherapy on optic nerve sheath diameter in patients with increased intracranial pressure. J Neurotrauma. 2014;31(10):984–8. https://doi.org/10.1089/neu.2012.2829.
Singer KE, Wallen TE, Jalbert T, et al. Efficacy of noninvasive technologies in triaging traumatic brain injury and correlating with intracranial pressure: a prospective study. J Surg Res. 2021;262:27–37. https://doi.org/10.1016/j.jss.2020.12.042.
Al-Mufti F, Lander M, Smith B, et al. Multimodality monitoring in neurocritical care: decision-making utilizing direct and indirect surrogate markers. J Intensive Care Med. 2019;34(6):449–63. https://doi.org/10.1177/0885066618788022.
Robba C, Santori G, Czosnyka M, et al. Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2018;44(8):1284–94. https://doi.org/10.1007/s00134-018-5305-7.
Martin M, Lobo D, Bitot V, et al. Prediction of early intracranial hypertension after severe traumatic brain injury: a prospective study. World Neurosurg. 2019;127:e1242–e1248.
Bothwell SW, Janigro D, Patabendige A. Cerebrospinal fluid dynamics and intracranial pressure elevation in neurological diseases. Fluids Barriers CNS. 2019;16(1):9. https://doi.org/10.1186/s12987-019-0129-6.
Killer HE, Jaggi GP, Flammer J, et al. Cerebrospinal fluid dynamics between the intracranial and the subarachnoid space of the optic nerve. Is it always bidirectional? Brain. 2007;130(Pt 2):514–20. https://doi.org/10.1093/brain/awl324.
Bradbury MW. Hugh Davson—his contribution to the physiology of the cerebrospinal fluid and blood-brain barrier. Cell Mol Neurobiol. 2000;20(1):7–11. https://doi.org/10.1023/a:1006987709018.
Czosnyka M, Czosnyka Z, Agarwal-Harding KJ, et al. Modeling of CSF dynamics: legacy of Professor Anthony Marmarou. Acta Neurochir Suppl. 2012;113:9–14. https://doi.org/10.1007/978-3-7091-0923-6_2.
Wilson MH. Monro-Kellie 2.0: The dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab. 2016;36(8):1338–50. https://doi.org/10.1177/0271678X16648711.
Kelman SE, Sergott RC, Cioffi GA, et al. Modified optic nerve decompression in patients with functioning lumboperitoneal shunts and progressive visual loss. Ophthalmology. 1991;98(9):1449–53. https://doi.org/10.1016/s0161-6420(91)32113-4.
Ocamoto GN, Russo TL, Mendes Zambetta R, et al. Intracranial compliance concepts and assessment: a scoping review. Front Neurol. 2021;12:756112. https://doi.org/10.3389/fneur.2021.756112.
Cardim D, Robba C, Czosnyka M, et al. Noninvasive intracranial pressure estimation with transcranial doppler: a prospective observational study. J Neurosurg Anesthesiol. 2020;32(4):349–53. https://doi.org/10.1097/ANA.0000000000000622.
Trocha G, Bonilla A, Romero C, Palacios J, Molano-Gonzalez N. Ultrasound measurement of optic nerve sheath diameter in a healthy adult Colombian population. BMC Neurol. 2023;23(1):16.
Reier L, Fowler JB, Arshad M, et al. Optic disc edema and elevated intracranial pressure (ICP): a comprehensive review of papilledema. Cureus. 2022;14(5):e24915. https://doi.org/10.7759/cureus.24915.
Aspide R, Bertolini G, Albini Riccioli L, et al. A proposal for a new protocol for sonographic assessment of the optic nerve sheath diameter: the CLOSED protocol. Neurocrit Care. 2020;32(1):327–32. https://doi.org/10.1007/s12028-019-00853-x.
Hirzallah MI, Lochner P, Hafeez MU, et al. Quality assessment of optic nerve sheath diameter ultrasonography: scoping literature review and Delphi protocol. J Neuroimaging. 2022;32(5):808–24. https://doi.org/10.1111/jon.13018.
Aletreby W, Alharthy A, Brindley PG, et al. Optic nerve sheath diameter ultrasound for raised intracranial pressure: a literature review and meta-analysis of its diagnostic accuracy. J Ultrasound Med. 2022;41(3):585–95. https://doi.org/10.1002/jum.15732.
Acknowledgements
We would like to thank the noninvasive intracranial pressure monitoring international consensus participants for their comments on this article based on their experience in the field: Fabio Silvio Taccone (Belgium), Frank Rasulo (Italy), Rafael Badenes R (Spain), David Menon (UK), Aarti Sarwal A (USA), Danilo Cardim D (USA), Marek Czosnyka (UK), Mohammad Hirzallah (USA), Thomas Geeraerts (France), Pierre Bouzat (France), Pier G. Lochner (Germany), Marcel Aries (Netherlands), Yu Lin Wong (Singapore), Yasser Abulhassan (Kuwait), Gene Sung (USA), Hemanshu Prabhakar (India), Gentle Shrestha (Nepal), Luis Bustamante (Colombia), Manuel Jibaja (Ecuador), Juan Pinedo (Peru), Diana Sanchez (Colombia), Julio Mijangos Mendez (Mexico), Franly Vásquez (Dominican Republic), Dhaval P Shukla (India), Getaw Worku (Ethiopia), Abenezer Tirsit (Ethiopia), Bhagavatula Indiradevi (India), Hamisi Shabani (Tanzania), Amos Adeleye (Nigeria), Thangaraj Munusamy (Malaysia), Amelia Ain (Philippines), Wellingson Paiva (Brazil), Daniel Godoy (Argentina), Sérgio Brasil (Brazil), Chiara Robba (Italy), Andrés Rubiano (Colombia), Sebastián Vásquez-García (Colombia).
Funding
Open Access funding provided by Colombia Consortium. This work received no funding.
Author information
Authors and Affiliations
Consortia
Contributions
KM-P: Methodology (equal), Writing—Original draft preparation (equal) SV-G: Methodology (equal), Writing—Original draft preparation (equal) OF: Software, Visualization, Writing—Reviewing and editing CR: Writing—Reviewing and editing AMR: Conceptualization, Supervision, Writing—Reviewing and editing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report in this project.
Ethical Approval/Informed Consent
This scoping review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews [16]. Although a protocol was written before beginning the review, the protocol was not published due to project time constraints. A total of two databases (PubMed and EMBASE) were searched, with initial search strategy formation being undertaken in PubMed. The final searches were completed in June of 2022, yielding 106 studies for review. All identified citations were collated and uploaded into Covidence, and one duplicated study was removed. Studies were screened by two independent researchers (KM and SV) and one collaborator (OF). After examining 105 titles and abstracts for inclusion, 74 irrelevant studies were removed, 31 full-text studies were assessed for eligibility, and 15 studies were excluded for reasons described in Fig. 1. Any conflicts that arose in the selection process were resolved by a tie-breaking vote from the third member who did not participate in the initial vote. The results of the search are reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist [16]. Data were extracted from included studies by all three researchers using a data extraction tool developed in the protocol and modified after initial review of the articles to present data in the clearest manner (Table 1). After two researchers completed extraction, consensus was achieved by mediation between the two researchers involved. In accordance with Joanna Briggs Institute methodology for scoping reviews specifically, included studies were not reviewed for quality or risk of bias.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martínez-Palacios, K., Vásquez-García, S., Fariyike, O.A. et al. Using Optic Nerve Sheath Diameter for Intracranial Pressure (ICP) Monitoring in Traumatic Brain Injury: A Scoping Review. Neurocrit Care 40, 1193–1212 (2024). https://doi.org/10.1007/s12028-023-01884-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01884-1