Abstract
The introduction of Ki67 immunohistochemistry in the work-up of neuroendocrine neoplasms (NENs) has opened a new approach for their diagnosis and prognostic evaluation. Since the first demonstration of the prognostic role of Ki67 proliferative index in pancreatic NENs in 1996, several studies have been performed to explore its prognostic, diagnostic, and predictive role in other neuroendocrine and endocrine neoplasms. A large amount of information is now available and published results globally indicate that Ki67 proliferative index is useful to this scope, although some differences exist in relation to tumor site and type. In gut and pancreatic NENs, the Ki67 proliferative index has a well-documented and accepted diagnostic and prognostic role and its evaluation is mandatory in their diagnostic work-up. In the lung, the Ki67 index is recommended for the diagnosis of NENs on biopsy specimens, but its diagnostic role in surgical specimens still remains to be officially accepted, although its prognostic role is now well documented. In other organs, such as the pituitary, parathyroid, thyroid (follicular cell-derived neoplasms), and adrenal medulla, the Ki67 index does not play a diagnostic role and its prognostic value still remains a controversial issue. In medullary thyroid carcinoma, the Ki67 labelling index is used to define the tumor grade together with other morphological parameters, while in the adrenal cortical carcinoma, it is useful to select patients to treated with mitotane therapy. In the present review, the most important information on the diagnostic, prognostic, and predictive role of Ki67 proliferative index is presented discussing the current knowledge. In addition, technical issues related to the evaluation of Ki67 proliferative index and the future perspectives of the application of Ki67 immunostaining in endocrine and neuroendocrine neoplasms is discussed.
Similar content being viewed by others
Introduction
The Ki67 antibody was created in 1983 by immunizing mice with nuclei of the Hodgkin lymphoma cell line L428. It was called “Ki” referring to the city Kiel where the research team worked and “67” referring to the original clone in the 96-well plate [1]. Although the function of the identified protein was not known, it was immediately clear that it was involved in cell proliferation being detected in proliferating normal and neoplastic cells. Unfortunately, the original Ki67 antibody only worked on frozen tissues and for this reason its use in routine practice was limited. Some years later, the monoclonal antibody MIB1, which works in formalin-fixed and paraffin-embedded tissues, was generated and since then the use of Ki67 immunohistochemistry in routine practice has become easy [2].
The prognostic role of Ki67 proliferative index in neuroendocrine tumors (NETs) was identified for the first time in 1996 by two independent Italian research teams [3, 4], and since then, many studies have been performed to evaluate its prognostic, diagnostic, and predictive role in other digestive neuroendocrine neoplasms (NENs). The encouraging results obtained in these investigations played a motor role to study the biological role of Ki67 in NENs located in other organs (i.e., pituitary, parathyroid, lung, etc.), but also in endocrine tumors such as follicular cell-derived thyroid tumors and adrenal cortical neoplasms. A large amount of information is now available and published results globally indicate that Ki67 proliferative index is a useful prognostic, diagnostic, and predictive biomarker, although some differences exist in relation to tumor site and type.
In the present review, the most important information on this topic will be presented and discussed. The current knowledge and the future perspectives of the application of Ki67 immunostaining will be analyzed in endocrine and neuroendocrine neoplasms arising in different organs and systems.
Ki67 Proliferative Index in Different Endocrine and Neuroendocrine Neoplasms
Pituitary Neuroendocrine Tumors (PitNETs)
Anterior pituitary tumors represent a peculiar well-differentiated neuroendocrine tumor type characterized by specific features depending on its site of origin and include distinct entities producing different hormones with variable propensity to local infiltration and/or metastatic dissemination [5]. For this reason, they are no longer considered “benign” tumors as in the past and, consequently, the terminology for their definition has recently changed from “pituitary adenomas” to “pituitary neuroendocrine tumors (PitNETs),” to better cover the spectrum of different biological characteristics [5, 6]. Once that this conceptual change has been made, the pathologist’s goal in the diagnostic work-up of PitNET is the identification of parameters able to recognize those cases associated with significant risk of recurrence or local infiltration. Considering the proposal of a common classification framework to unify the nomenclature of neuroendocrine neoplasms (NENs) arising in different organs, which is based on morphological differentiation and proliferation [7], the role of Ki67 proliferative index may be important to better define PitNETs and to stratify them in different prognostic categories. Although several attempts have been made to explore it, the predictive value of Ki67 proliferative index in PitNETs still remains to be definitively confirmed [8, 9]. The prognostic role of Ki67 index has been explored and its integration with morphological and radiological evidence of local infiltration seemed promising for identifying tumors at high risk of local recurrence and/or infiltration [10]. This approach has been confirmed in different series, which also demonstrated the strong prognostic role of PitNET subtype. Indeed, certain tumor types behave per se in a more aggressive fashion such as immature PIT1-lineage tumors, Crooke cell tumors, null cell tumors, silent corticotroph tumors, and sparsely granulated somatotroph and corticotroph tumors [11,12,13,14]. In a recent paper, an integrated multiparametric approach demonstrated that tumor type (mainly ACTH subtype), Ki67 index ≥ 3% (Fig. 1), mitotic count > 2/10 HPF, local invasion, “grade 2” of the Trouillas’ grading, and p53 protein expression were predictor of disease recurrence or progression [15]. Taken together, all these findings suggest that the Ki67 proliferative index, although may give an indication on PitNETs biology, does not have alone an independent prognostic role and needs to be integrated with other parameters. Tumor subtype currently has a major prognostic meaning [16] reflecting what observed in other NETs such as gastric ECL-cell NETs for which the most important prognostic marker is tumor subtype rather than the proliferation index alone [17].
Head and Neck Neuroendocrine Neoplasms
The new 2022 classification of head and neck tumors [18] includes a specific chapter on the classification of NENs and represents an important evolution respect to the previous classification, which used a confounding terminology that has created uncertainties among pathologists and clinicians [19]. The new classification is in line with the common classification framework proposed by WHO/IARC [7] and separates head and neck NENs into well differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs), although, for obscure reasons, it does not include mixed neuroendocrine/non-neuroendocrine neoplasm (MiNEN) as a specific entity [18]. In this context, Ki67 has been introduced as parameter for the classification, not alone but integrated with other morphological parameters such as the presence of necrosis and mitotic count, reflecting the morphological approach used in the lung (see below). The combination of Ki67 index, mitotic count, and presence of necrosis allows to classify tumors into NET G1, NET G2, and NET G3, the last still considered as a provisional entity due to limited data available in the literature (Table 1). In the head and neck region, the distinction between NET G1 and NET G2 does not use the same criteria of the digestive system. Indeed, both entities are characterized by a Ki67 index < 20% [20, 21] and their separation is based on morphological criteria using necrosis and mitoses. Obviously, this Ki67 threshold is too high and does not help the distinction between G1 and G2 NETs; thus, a more specific cutoff for their separation is needed [22] and will be welcome. Conversely, Ki67 count is crucial to identify those NETs with higher biological aggressiveness and characterized by a Ki67 percentage higher than 20% that are defined NET G3. Since the Ki67 value (> 20%) is the same observed in NECs, the differential diagnosis between NET G3 and NECs, either small or large cell subtype, is mainly based on morphology, associated with molecular profile, which can partly be evaluated using immunohistochemical surrogate-marker analyses.
Olfactory neuroblastoma is a peculiar nonepithelial neoplasm showing neuroendocrine differentiation and including different clinically relevant subgroups mainly defined using a morphological grade (Hyams grade) [18]. However, recent studies have demonstrated that the Ki67 labelling index has a prognostic relevance and, in particular, Ki67 index > 20% (Fig. 2) is associated with a worse prognosis [23, 24].
In conclusion, the 5th edition of the WHO classification of head and neck tumors represents an important evolution respect the previous one and introduces, for the first time, a diagnostic role of Ki67 labelling index that, however, needs to be better characterized in terms of refined cut-offs to use to precisely define the different entities.
Thyroid Tumors
Follicular Cell-Derived Neoplasms
The diagnostic role of Ki67 proliferative index in follicular cell-derived neoplasms has been investigated in several papers. In follicular and oncocytic neoplasms, the Ki67 index has been found to be lower in adenomas than in carcinomas [25,26,27,28], although overlaps exist between the two entities [29,30,31,32]. More recently, the Ki67 proliferative cutoff of 4% has been proposed to separate these two entities, suggesting a promising role of Ki67 in the diagnostic work-up that, however, needs to be validated [33]. For this reason, the differential diagnosis between adenoma and carcinoma, either follicular or oncocytic, still resides on morphology evaluating capsular and vascular invasion.
Ki67 index has also been investigated as a possible prognostic marker in the group of minimally invasive follicular carcinoma. Although it was found to correlate with disease-free survival, its impact was less powerful than vascular invasion and patient’s age [34]. The prognostic role of Ki67 index in widely invasive follicular carcinoma has been explored as well. Although Ki67 index > 5% seems associated with high risk of recurrence, there are not sufficient data supporting its powerful when compared with other markers such as vascular invasion [35].
Additional efforts have been made to explore the possible role of Ki67 in identifying aggressive follicular cell-derived carcinomas (i.e., poorly differentiated thyroid carcinoma -PDTC-) and in stratifying patients in different prognostic categories. Several papers suggested that the increase of Ki67 proliferative index parallels the decrease in differentiation and that PDTC generally shows a 10–30% Ki67 index [25]. However, an optimal diagnostic cut-off able to identify PDTC still remains to be defined. For this reason, in the 5th edition of WHO classification of endocrine tumors, the group of high grade follicular-derived carcinomas, which includes PDTC and differentiated high-grade thyroid carcinoma (DHGTC), is defined only using morphological parameters such mitotic count and the presence of necrosis [6].
The diagnosis of papillary thyroid carcinoma (PTC) resides on nuclear morphology and Ki67 does not have any diagnostic role in this context. However, Ki67 index has been explored as a potential prognostic marker. Some studies have suggested a possible prognostic role when combined with other biomarkers such as CK19 expression or TERT promoter/BRAFV600E mutations [36,37,38], but, in principle, aggressive histological variants of PTC generally show higher Ki67 labelling index than classical variant [25], although some exceptions have been reported.
The formerly known cribriform-morular variant of PTC [39] is now redefined as cribriform-morular thyroid carcinoma since this tumor is considered as a distinct malignant thyroid neoplasm of uncertain histogenesis [40] with relatively indolent behavior but relatively high Ki67 index [39].
In conclusion, all these findings suggest that Ki67 proliferative index does not have a prominent value in thyroid pathology. The currently used well-defined morphological diagnostic algorithms allow the correct and specific diagnosis of thyroid neoplasms, which also correlates with prognosis. The prognostic role of Ki67 index is promising but need to be better defined. In addition, it is worth noting that no well standardized methods for Ki67 count have been validated in the thyroid. Consequently, published data that have been obtained using different protocols proposed different Ki67 cut-off values making the results hard to compare [41,42,43,44,45].
Medullary Thyroid Carcinoma
Medullary thyroid carcinoma (MTC) is a primary neuroendocrine neoplasm of the thyroid composed of calcitonin-secreting C-cells. It is a rare but relatively aggressive cancer and can be sporadic or can arise in the setting of hereditary diseases [6]. In hereditary MTC early detection of cancer, performed using biochemical and/or genetic screening, plays a major role in improving patient’s outcome [46, 47]. The prediction of survival in patients with sporadic MTC additionally includes other prognostic markers that negatively influence the survival, such as large tumor size, extrathyroidal extension, old age, male gender, serum calcitonin and CEA levels, and RET mutations in exons 15 and 16 [46,47,48,49,50]. With the aim to improve the stratification of patients in different prognostic categories, two grading systems based on proliferation (mitotic count and/or Ki67 index) and necrosis have been proposed: the Sydney grading system [51] and the Memorial Sloan Kettering Cancer Center grading system (MSKCC) [52]. Starting from these observations, a group of internationally recognized experts in thyroid pathology from the USA, Europe, and Australia recently proposed the International Medullary Thyroid Carcinoma Grading System (IMTCGS) that, combining proliferation (mitotic count and Ki67 proliferative index) and necrosis, separates MTC in two different prognostic categories: low and high grade MTC (Fig. 3 and Table 2) [53]. The IMTCGS system has been validated in other series [54] and appears well reproducible [55]. In conclusion, recent findings have demonstrated that Ki67 labelling index plays a prognostic role in MTC, although the better prognostic stratification of patients is obtained combining Ki67 index with necrosis (IMTCGS system).
Parathyroid Neoplasms
The differential diagnosis between parathyroid adenoma and carcinoma depends on the presence of at least one of the following morphological features: angioinvasion, lymphatic invasion, perineural invasion, invasion into the adjacent structures/organs, or, obviously, the presence of regional or distant metastasis [6, 56]. However, since their distinction is not rarely problematic [57], several biomarkers have also been investigated during the last years to help in solving this issue. Among them, Ki67 index was evaluated, and the first studies were published in the last decade of the twentieth century [58]. Ki67 index was found to be higher in parathyroid tumors and hyperplasia than in normal glands [59] and, among tumors, in carcinoma than in adenomas [60]. Ki67 index higher than 5% has been suggested to be associated with malignancy [61], but due to the overlap of Ki67% values between adenoma and carcinoma and to the observation that in secondary parathyroid hyperplasia and multiglandular parathyroid disease Ki67 index may be higher than in adenoma and carcinoma [59], this marker cannot be used alone [62]. A diagnostic nomogram including five biomarkers (parafibromin, Rb, Ki67, PGP9.5, and galectin 3) has been proposed but Ki67 did not show as good performance as the staining for parafibromin in distinguishing adenoma from carcinoma [63]. In addition to its diagnostic role, Ki67 index has also been explored as a prognostic marker in parathyroid tumors, without definitive results [64, 65]. For these reasons, Ki67 it is not currently included in the diagnostic algorithm of parathyroid neoplasm for the differential diagnosis between parathyroid adenoma and carcinoma, although it may give an overview on the proliferative activity of the tumor. However, Ki67 should be evaluated as a complementary possible prognostic marker and reported as a continuous variable since no definite prognostic cutoff has been identified yet.
Thoracic Neuroendocrine Neoplasms
The role of Ki67 proliferative index in the diagnosis and prognostic evaluation of lung neuroendocrine tumors (carcinoids) has been matter of debate in recent years. Its more and more emerging diagnostic and prognostic relevance in the work-up of digestive neuroendocrine neoplasms has supported its application in the diagnosis of lung NENs and several papers have been published in recent years on this topic [66]. However, its introduction as a routine diagnostic marker for lung NENs has encountered some difficulties. The major obstacle has resided in the fact that morphological criteria (mitotic count and necrosis) traditionally used for diagnosing lung NENs in surgical specimens works well in identifying different NEN entities characterized by different morphological, molecular and prognostic features: typical carcinoid (TC), atypical carcinoid (AC), large cell neuroendocrine carcinoma (LCNEC), and small cell carcinoma (SCLC). Consequently, the Ki67 index has been considered not adding additional and practical advantage in this setting.
However, Ki67 has emerged as a potentially useful marker in the diagnostic work-up of lung NENs in biopsy specimens [67]. Indeed, extensive crush artifacts are frequently observed in tissue fragments obtained with biopsy procedures and this creates difficulties in interpreting the morphological picture and to get the right pre-operatory diagnosis, which is strategic for patients’ management. In this context, the Ki67 labeling index is helpful because lung NETs (carcinoids) show lower Ki67 rates (< 20–30%) than lung NECs, both small and large cell subtypes, where the Ki67 index is over 50% and not rarely exceed 70–80% [67,68,69]. For this reason, Ki67 immunohistochemistry is strongly recommended in the diagnostic work-up of bronchial or lung biopsies (Fig. 4) when the neuroendocrine nature of the lesion is confirmed by the immunoreactivity for neuroendocrine markers (synaptophysin, chromogranin, and INSM1).
Lung biopsies of neuroendocrine neoplasms frequently present crush artifacts creating difficulties in interpreting the morphological picture. In this context, Ki67 is useful to distinguish NET (carcinoid) from NEC. A refers to a NET, which shows low Ki67 labelling (B). (C) is a small cell carcinoma presenting high Ki67 immunolabelling (D) (courtesy of Prof. Giuseppe Pelosi, University of Milan, Milan, Italy)
As above discussed, the Ki67 index is not currently essential for the diagnosis and classification of lung NENs, which is based on morphological features [70]. However, Ki67 has been introduced in the last 2021 WHO classification (5th Edition) as a parameter helping the distinction among different entities, with a range of percentages of Ki67 positive cells indicated for each entity: up to 5% for typical carcinoid, up to 30% for atypical carcinoid, and > 30% for NECs (either small or large cell subtypes) [70]. Interestingly, a growing burden of information has indicated that the Ki67 labelling index also plays a prognostic role in lung NENs and is useful for better defining the biological behavior of different lung NEN subtypes and, especially, of NETs (carcinoids) [69, 71, 72]. Reflecting the classification used for digestive NENs (see below) and considering the recent proposal for a common classification framework of NENs of different sites [7], a three-tiered stratification may also be proposed with TCs corresponding to G1 NETs, ACs to G2 or G3 NETs and LCNEC and SCNECs to NECs. However, while in the digestive system, the cutoffs to separate G1 from G2 and G3 categories have been accepted, in the lung they are not well defined, and especially they do not have a direct correspondence with the specific morphologically defined entities. In other words, there are not universally accepted established Ki67 cutoff points able to separate TC from AC and for distinguishing carcinoids from both small and large cell NECs [69, 72]. However, based on expert opinion, it has been suggested that tumors with a Ki67 < 5% likely correspond to TCs (NET G1), those with Ki67 > 5% to ACs (NET G2) and those with Ki67 index > 30% likely correspond to NECs [66].
Another recent and clinically relevant issue regarding the role of Ki67 in the diagnosis and prognosis of lung NETs (carcinoids) is the identification of a subset of lung NETs (ACs) showing high proliferative rates (Fig. 5) [73,74,75,76]. These cases associate a well differentiated morphology with a high proliferation rate (> 10 mitoses per 2 mm2 and > 30% Ki67 index) and considering the last parameter they should be classified as LCNECs. Interestingly, these tumors show a molecular profile closer to carcinoids (NETs) rather than to NECs, lacking RB1 or TP53 mutations and showing a low total mutation burden, and/or presence of MEN1 mutations [77]. In addition, these tumors show a prognosis different from that of conventional LCNEC. For these reasons, the term “carcinoid tumors with elevated mitotic counts and/or Ki67 proliferation rates” has been proposed in the 5th edition of WHO classification [70]. These NETs [78] likely correspond to NET G3 well described and characterized in the digestive system [79], underlining once again a sort of parallelism between digestive and lung NENs and consequently supporting the use of a common classification framework recently proposed by WHO/IARC [7].
In conclusion, although the diagnosis and the management of patients with lung NENs currently rely on the histologic classification, the growing relevance of Ki67 as diagnostic and prognostic marker has implied the introduction of the evaluation of Ki67 index in at least three setting of the diagnostic pathology work-up. First, it is now mandatory to perform Ki67 immunohistochemistry in biopsy specimens to avoid overdiagnosing NETs (carcinoids) as NECs. Second, to identify those TCs (with > 5%) that may behave more aggressively than expected or, conversely, those ACs (with Ki67 < 5%) that may show a less aggressive fashion than expected [80,81,82,83,84]. Third, to identify those ACs with high proliferation (likely corresponding to the NET G3 category accepted in the digestive system) that have been traditionally considered LCNECs but that show a prognostic feature in the middle between NET and NEC.
The personal opinion of the author is that, not forgetting some specific site-related peculiarities, the classification of lung NENs should be uniformed with that of the digestive system including lung NET G1, NET G2, NET G3 as well-differentiated tumors and small and large cell NECs as poorly differentiated ones (Table 3). The term carcinoid should be abandoned also for clinical reasons because the carcinoid syndrome, except for rare cases of atypical carcinoid syndrome, is not observed in lung NETs and consequently this fascinating but old term may be confounding [85].
Thymic NENs are currently classified and defined using the morphological criteria used in the lung [70]. They are rare accounting for about 0.4% of all NENs of the body and, for this reason, there are not published studies including large series. In this context, the available data on the diagnostic and prognostic role of Ki67 proliferative index are limited [86, 87]. From a diagnostic point of view, Ki67 is suggested as desirable diagnostic criterium for the differential diagnosis between carcinoid (NET) and NEC (both large and small cell) in biopsy specimens, as proposed in the lung [70]. The prognostic role of Ki67 in thymic NETs has been poorly investigated and finding on small series seems to suggest that the cutoff of 10% is able to separate patients into two different groups [87].
Gut and Pancreatic Neuroendocrine Tumors
Most of published studies on Ki67 proliferative index have been performed in gut and pancreatic NENs, probably because the first investigations on the prognostic role of Ki67 index were performed in the pancreas [3, 4]. Since these first pioneer studies, Ki67 index has become increasingly important in the pathology work-up of NENs reaching a crucial pivotal role in 2006 when the European Neuroendocrine Tumor Society (ENETS) proposed a 3-tiered grading system with prognostic relevance [88, 89]. The utility of this grading system has successively been validated in several studies [90] and, for this reason, was accepted by the WHO/IARC in 2010 [91]. With only minor changes respect to the original ENETS proposal, this grading system is currently in use (Fig. 6 and Table 4) [79, 92]. However, although, as a whole, the Ki67 proliferative index is able to give prognostic information, some subtle but important differences related to tumor type and site of origin need to be considered in routine practice.
Stomach
The majority of gastric NETs are histamine-producing ECL-cell NETs that include at least five subtypes characterized by different clinico-pathologic features, strongly related per se to prognosis. Indeed, NETs not associated with hypergastrinemia (type 3) behave worse than NETs associated with high gastrin serum levels (type 1, type 2, type 4, and type 5) that, in turn, have different prognostic profile depending on the clinico-pathologic background [93]. In this context, the prognostic role of the Ki67 proliferative index needs to be integrated with the intrinsic biological characteristics of different NET types. In type 1 ECL-cell NETs (associated with chronic atrophic gastritis), Ki67 index does not play a major role since G1 and G2 tumors show similar behavior [17]. Conversely, in type 3 NET (not associated with hypergastrinemia and arising in normal gastric mucosa), Ki67-based grading stratifies patients in different prognostic groups [17]. Published data on the Ki67 role in type 2 NETs (MEN1 patients with gastrinoma) and type 4 ECL-cell NETs (associated with defect/lack of proton pump function) are not sufficient to have a clinical application. Type 5 ECL-cell NET, observed in patients long term treated with proton pump inhibitors and arising in normal or slightly hyperplastic peri-tumoral oxyntic mucosa (oxyntic gland dilatation, parietal cells with apocrine-like swelling and cytoplasm snouting), is a recently recognized subtype that can be of grade 1, 2, or 3. Since no death or distant metastasis was seen during follow-up, in this specific ECL-cell NET subtype, Ki67 index probably does not play a significant prognostic role [94].
Duodenum
Duodenal NETs include three different tumor types showing different morphological and clinical features: gastrinoma (functioning gastrin-producing NET), ampullary somatostatin-producing D-cell tumor, and non-functioning NET [95]. In addition to pure epithelial NETs, in the duodenum a fourth peculiar triphasic tumor composed of neuroendocrine, schwannian, and ganglion cells can be rarely observed. It was previously called gangliocytic paraganglioma, but it has renamed composite gangliocytoma/neuroma and neuroendocrine tumor (CoGNET) in the last 2022 WHO classification of neuroendocrine tumors arising in non-neuroendocrine organs [6]. As other digestive NETs, the duodenal ones are graded using proliferation indices, independently of the specific category. The prognostic role of Ki67 labelling index has been investigated and Ki67-based grading correlated with lymph node metastasis and, at univariate analysis, with disease-specific survival. However, Ki67 was not an independent prognosticator in G1 and G2 duodenal NETs at multivariate analysis [95]. When considering only ampullary NETs, grade proved to be a strong predictor of disease-specific survival together with patient age > 60 years, small-vessel invasion, pancreatic invasion, and distant metastasis at diagnosis [96]. G3 NETs were frequently associated with metastases suggesting that the clinical role of Ki67 expression becomes relevant when it reaches and exceeds 20% [97]. These findings suggest that Ki67 may be useful to identify duodenal NETs with increased risk of metastatic dissemination especially in G3 cases, although its impact on survival needs to be integrated with other parameters. The best prognostic approach appears to be multiparametric including Ki67 index, tumor size and duodenal wall infiltration [95, 96].
Ileum
Ileal NET is a peculiar tumor that, despite its small size, well-differentiated morphology and low Ki67 index (generally < 3%), in most cases deeply infiltrates the intestinal wall and is associated with loco-regional lymph node metastases at presentation [98, 99]. This feature suggests that Ki67 index is not a good predictor of metastatic potential in this specific site. However, Ki67 proliferative index has been found to correlate with prognosis using the cutoffs proposed by ENETS/WHO [89]. Interestingly, Panzuto et al. evaluated the risk of tumor progression and death for each increasing Ki67 unit that was 14% and 18%, respectively [100]. This approach appears biologically more correct than the use of fixed Ki67 cutoffs separating different categories, because Ki67 is a continuous variable.
Appendix
NETs of the appendix are generally small indolent tumors that, although frequently infiltrate through the appendiceal wall, rarely disseminate to local lymph nodes and almost never give distant metastases. The prognostic role of Ki67 labelling index has been explored in these tumors and some studies demonstrated that the distinction of grade 1 and grade 2 does not correlate with prognosis [101, 102], while others showed that Ki67 > 3% (grade 2), tumor size > 15.5 mm, and presence of lymphatic and vascular infiltration are associated with higher propensity to lymph node metastases [103]. However, the role and impact of lymph node metastases on patient’s prognosis still remains to be clarified.
Rectum
Rectal NETs are generally indolent tumors since in most of cases are diagnosed as small (< 10 mm) mucosal/submucosal lesions that can be easily resected during colonoscopy. In most of cases, rectal NETs are grade 1 (Ki67 < 3%) and these G1 NETs show a better survival than G2 NETs [104,105,106]. Although Ki67 correlated with prognosis at univariate analysis [105,106,107], it was not an independent prognosticator at the multivariate analysis [107] suggesting that a multiparametric approach evaluating Ki67 together with tumor size, lymphatic and vascular invasion, level of wall infiltration, and immunophenotype (L-cell versus EC-cell NET) may be the best tool to identify patients at higher risk of metastasis and tumor-related death.
Pancreas
The prognostic role of Ki67 proliferative index was investigated and demonstrated for the first time in pancreatic NETs (PanNETs) [3, 4], and since then, several other studies confirmed this observation [90]. For this reason, Ki67 index has become more and more important for the definition of PanNET behavior as demonstrated in multicentric studies including a large number of cases [108, 109]. The large body of evidence on the Ki67 prognostic role gained in PanNETs has encouraged and stimulated to explore it in other organs where, with some site- and tumor type-dependent peculiarities, it proved to play a relevant clinical role as observed in the pancreas. Consequently, Ki67 has been endorsed by WHO/IARC to be used for stratifying NETs in different prognostic categories [7]. The biological role of Ki67 in PanNETs has also been supported by a recent investigation demonstrating that gene expression profiles, mutational burden including DAXX and ATRX mutations, and LINE-1 methylation status correlate with Ki67 grade. In this study, the genetic similarities observed between G1 and G2 PanNETs suggest that only a few genes may play a role in the switch from indolent G1 to relatively aggressive G2 cases. Interestingly, the activation of a larger panel of genes was observed between G2 and G3 and, even more, between G3 and G1 PanNETs outlining the difference which exists between G1/G2 and G3 tumors [110]. All these findings suggest that Ki67 immunohistochemistry is mandatory in the work-up of PanNETs and that tumor grade represents the cornerstone for the prognostic evaluation of patients.
Adrenal Cortical Neoplasms
Adrenal cortical neoplasms include adenoma and carcinoma that have been traditionally differentiated using specific classification systems based on morphological criteria not including Ki67 evaluation: the Weiss system [111], the reticulin algorithm [112], the Lin-Weiss-Bisceglia system for oncocytic neoplasms [113], and the AFIP system for pediatric neoplasms [114]. More recently, the Ki67 proliferative index, used as a continuous value and not fixed in established cut-offs, has been incorporated together with mitotic count and necrosis in a diagnostic system (the Helsinki scoring system, Table 5) [115], which has been validated in other series including a large number of cases [116]. Ki67 index > 5% is observed in most adult adrenocortical carcinomas [117,118,119], but this cutoff is not completely validated and Ki67 index seems to work better as a continuous variable as proposed in the Helsinki scoring system. For this reason, it has not been officially included in the new 2022 WHO classification as a diagnostic marker, although reporting Ki67 value is strongly recommended also for its prognostic and predictive relevance [6, 120]. Indeed, Ki67 index has been found to have a prognostic role in adrenal cortical carcinoma for which a Ki67-based prognostic score has been proposed to separate cancers into three groups with low (< 20%), intermediate (20–50%), and high (> 50%) Ki67 values [121]. More recently, the Ki67 index > 15% has been validated as prognostic cut-off in pediatric and adult cohorts being associated with higher risks of recurrence and/or poor outcome [118, 119, 122]. Interestingly, in pediatric patients, Ki67 < 15% was not associated with a clinical malignant behavior and consequently strongly recommended to be incorporated in the pathology report [118].
The Ki67 proliferative index also plays a crucial role in the selection of patients to treat with adjuvant mitotane therapy, which, after radical surgery, is suggested for cancers with high risk of recurrence characterized by stage III, or R1 resection, or Ki67 index > 10% (Fig. 7) [123, 124].
In A is presented an example of adrenal cortical carcinoma with Ki67 index < 10% (B), while in (C) an example of adrenal carcinoma with Ki67 > 10% (D). The Ki67 proliferative index plays a role in the selection of patients to treat with adjuvant mitotane therapy, indicated when Ki67 index is higher than 10%
In conclusion, although Ki67 proliferation index is not officially included as a diagnostic marker to differentiated adrenal cortical adenoma from carcinoma in the 5th WHO classification of endocrine and neuroendocrine tumors, it should be evaluated and considered a continuous numeric value to give a prognostic indication and to select patients to undergo mitotane therapy.
Pheochromocytoma/Paraganglioma
The diagnosis of pheochromocytoma and paraganglioma is currently based on morphological and immunohistochemical criteria and, in this context, Ki67 immunolabelling does not have a diagnostic role. However, in the past, before the realization that these two tumor types are malignant, Ki67 expression was evaluated to explore its usefulness to differentiated “benign” from “malignant” neoplasms. In this context, Ki67 proliferative index has emerged as a reliable marker for identifying cases with high risk of metastatic dissemination and worse prognosis [125,126,127]. In particular, a Ki67 index > 3% was suggested to be prognostically relevant (Fig. 8), although it has not been confirmed in other recent studies [128].
As above mentioned, pheochromocytoma and paraganglioma are malignant neoplasms by definition. Once the diagnosis is morphologically and immunohistochemically performed, pathologists should search for parameters able to stratify patients in groups with different risk of metastasis and to this scope different systems have been proposed. The PASS score (pheochromocytoma of the Adrenal gland Scaled Score) was the first [129], and it was based on morphological criteria not including Ki67, which was successively integrated with growth pattern, cellularity, comedo-type necrosis, angioinvasion, and capsular invasion in the GAPP (Grading system for Adrenal Pheochromocytoma and Paraganglioma) system [130]. More recently, the COPPS score (Composite Pheochromocytoma/paraganglioma Prognostic Score), which is based on tumor size, the presence of necrosis and vascular invasion, and the loss of S100 and/or SDHB immunoreactivity but not including Ki67, has been proposed [131]. Although these systems have not proven to be sufficiently sensitive and specific to be endorsed for routine use, the 2022 WHO classification of pheochromocytoma and paraganglioma does not discourage their use [132]. As above mentioned, Ki67 is mainly considered as a prognostic marker, but it is worth noting that it may have a negative diagnostic role. Indeed, in pheochromocytomas and paragangliomas Ki67 proliferative index is generally less than 10% (Fig. 8) and a higher percentage should raise the suspicion that the tumor under examination is not a phaeochromocytoma or a paraganglioma [6].
In conclusion, Ki67 proliferative index only has a partial diagnostic role in the work-up of phaeochromocytoma and paraganglioma, but it can be useful, integrated with other prognostic marker, to identify those neoplasms at high risk of metastatic dissemination. For this reason, Ki67 immunohistochemistry is strongly recommended in the work-up of pheochromocytoma and paraganglioma [133].
Urogenital Neuroendocrine Tumors
Neuroendocrine neoplasms of the urinary tract and male genital system have been traditionally defined and classified in the old literature using different terms. Taking into account the WHO/IARC proposition of a common classification framework unifying the nomenclature of NENs arising in different organs [7], the 5th edition of WHO classification of urinary and male genital tumors dedicates a specific chapter to NENs and classifies them into NET and NEC [134]. The diagnosis is based on morphology and immunohistochemical profile and Ki67 does not play a major role in this setting. However, Ki67 may play a prognostic role but, due to rarity of these neoplasm, it needs to be definitively determined. Promising findings suggest that a Ki67 index > 3% is associated with worse behavior [135, 136].
In the last WHO classification of female genital tumors (5th edition) NENs are discussed in a specific chapter and separated into NET, NEC, and MiNEN following the WHO/IARC scheme [7]. The diagnostic criteria are based on morphology and tumor grade is based on mitotic count and on the presence/absence of necrosis, with grade 1 NET showing no necrosis and < 5 mitoses per 2mm2, and grade 2 NET with 5–10 mitoses per 2mm2 and necrosis. Strangely and not in line with the WHO/IARC recommendation, Ki67 is not included as a parameter to be considered for grading NETs [137], and this may represent a diagnostic weak point for the identification of the rare G3 NETs that, although rare, can also be observed in this system [138]. Although in some studies Ki67 has been investigated [139, 140] its real prognostic role in NET of the female genital tract still remains to be validated.
NECs
NECs are grade 3 cancers associated with dismal prognosis. Their diagnosis is based on the specific histological features and is supported by the demonstration of a neuroendocrine phenotype that includes the expression of synaptophysin, INSM1, and chromogranin, the latter being focally expressed or even negative in a not negligible number of cases. Ki67 index is by definition > 20% (digestive system) or > 30% (lung), but not rarely it reaches 70–80% or more helping in the differential diagnosis with G3-NETs that have a Ki67 index > 20% but which rarely exceeds 50–60%. The differential diagnosis between G3-NET and NEC in difficult cases can be made by integrating the Ki67 proliferative index with p53 and Rb immunohistochemistry, since most NECs show TP53 and RB mutations and consequent p53 and Rb aberrant immunohistochemical expression. The prognostic role of Ki67 in NECs has been evaluated. The first study demonstrating that the cutoff of Ki67 index of 55% was able to separate G3 NENs in two different prognostic groups, which also differently responded to platinum-based chemotherapy, was published in 2013 [141]. Although this investigation represented the start point to better understand the heterogeneity of G3-NENs, it suffered from the lack of morphological revision of enrolled cases. However, this cutoff has been demonstrated to have a prognostic role in well-characterized series of NECs where the rare NECs with Ki67 < 55% behave in a better fashion than those with Ki67 > 55% [142]. For this reason, Ki67 immunohistochemistry is suggested also when diagnosing NECs.
The role of Ki67 index in Merkel cell carcinoma (MCC) has been investigated as well. The Ki67 cutoff value of 55% was found to be able to separate two distinct prognostic groups with that showing Ki67 > 55% associated with a worse outcome, which also depends on stage IV, lack of Merkel cell Polyoma Virus (MCPyV), and p63 expression. However, at multivariate analysis, survival resulted independently influenced only by p63 expression and tumor stage [143].
Technical Issues and Practical Suggestions for the Evaluation of Ki67 Proliferative Index
Ki67 is expressed in proliferating cells, but with a variable nuclear distribution among the different phases of the cell cycle [144]. For this reason, all immunoreactive nuclei, independently of the intranuclear distribution or intensity of the staining, should be scored [145]. The Ki67 index is expressed as the percentage of Ki67 immunoreactive cells in at least 500 tumor cells counted in the highest labeled area (“hot spot”). The best method to perform this count has been matter of debate in the last years and different systems have been proposed: eyeballing evaluation, automatic computer-assisted count, manual count at the microscope, and manual count on camera-capture printed images. Among them, manual count of Ki67 positive nuclei in camera-captured printed images has appeared to be the most reliable procedure (Fig. 9) [146]. It takes an average time between 10 and 15 min (longer than the other methods) but shows good reproducibility and can be used by most pathologists, since a camera-equipped microscope is available in most laboratories. Automated counting seems to have comparable accuracy (Fig. 10), but it needs a specific software not available in all laboratories [147].
Example of Ki67 index evaluated by manually counting unlabeled and labeled nuclei on a camera-captured, printed image. In this picture, 81 Ki67-labeled cells were counted and then divided by a total of 1581 cells, resulting in a Ki67 index of 5.1% (republished with permission of Springer from the article: Klöppel et al. [90] Ki67 labeling index: assessment and prognostic role in gastroenteropancreatic neuroendocrine neoplasms. Virchows Arch 472:341–349)
Although immunohistochemical techniques have been improved and standardized in the last years with the introduction of automated staining machines, the Ki67 immunostaining is a delicate procedure influenced by several factors including tissue processing and fixation, the use of different reagents and pretreatments [148], which result in well documented interlaboratory variability [149]. For this reason, each laboratory should optimize the procedure to warrant a reproducible result.
Future Perspectives
Published papers on Ki67 expression in endocrine and neuroendocrine neoplasms have generally demonstrated that the Ki67 proliferative index plays a prognostic role, either alone (i.e., in the pancreas) or in combination with other morphological parameters including tumor subtype (i.e., in the stomach and pituitary), local invasion (i.e., in the pituitary), mitotic count and necrosis (i.e., in the lung) or necrosis alone (in the thyroid). However, the value of Ki67 index is not always the same and some specific differences in its prognostic power depend on tumor type and its site of origin.
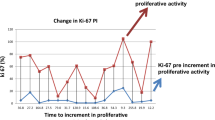
It is worth noting that in term of biological meaning the current application of Ki67 proliferative index presents a conceptual limit. Ki67 has been considered as a static parameter, a choice due to the need to have practical values useful to stratify patients in prognostic groups easy to be applied in routine diagnostic work. However, Ki67 index should be considered as a continue variable as done in the Helsinki score for adrenal cortical neoplasms [115] and this approach may better reflect its biological meaning. It is clear that grouping NENs using strict cutoff values, although easy, put together neoplasm with different biological aggressiveness as demonstrated by digestive G2-NET group where cases with Ki67 index of 3% are grouped with cases showing a higher Ki67 index (i.e., 19%). In this context, the use of a Ki67-related biological risk of tumor recurrence or tumor-related death may appear more accurate. In some studies, the Ki67-related biological risk has been evaluated [100, 150]. In lung ACTH-secreting NETs a 1.41 increased risk of recurrence has been noted for each 1% of Ki67 index [150]. In ileal NETs, a 18% increased risk of death for each increasing unit of Ki67 index has been found [100]. This approach seems relevant and further studies are needed to better evaluate its role in different NET types.
The predictive role of Ki67 for therapeutic purpose needs to be better explored in both neuroendocrine and endocrine neoplasms and now is only well established to select patients with adrenal cortical carcinomas who can be treated with mitotane.
Availability of Data and Materials
Published literature.
References
Gerdes J, Schwab U, Lemke H, Stein H (1983) Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int J Cancer 31:13-20.
Kreipe H, Heidebrecht HJ, Hansen S, Rohlk W, Kubbies M, Wacker HH, Tiemann M, Radzun HJ, Parwaresch R (1993) A new proliferation-associated nuclear antigen detectable in paraffin-embedded tissues by the monoclonal antibody Ki-S1. Am J Pathol 142:3-9.
La Rosa S, Sessa F, Capella C, Riva C, Leone BE, Klersy C, Rindi G, Solcia E (1996) Prognostic criteria in nonfunctioning pancreatic endocrine tumours. Virchows Arch 429:323-333.
Pelosi G, Bresaola E, Bogina G, Pasini F, Rodella S, Castelli P, Iacono C, Serio G, Zamboni G (1996) Endocrine tumors of the pancreas: Ki-67 immunoreactivity on paraffin sections is an independent predictor for malignancy: a comparative study with proliferating-cell nuclear antigen and progesterone receptor protein immunostaining, mitotic index, and other clinicopathologic variables. Hum Pathol 27:1124-1134.
Asa SL, Mete O, Cusimano MD, McCutcheon IE, et al (2021) Pituitary neuroendocrine tumors: a model for neuroendocrine tumor classification. Mod Pathol 34:1634-1650.
WHO Classification of Tumours Editorial Board (2022) Endocrine and Neuroendocrine tumours. WHO classification of tumours series, 5th ed.; vol. 8. International Agency for Research on Cancer, Lyon
Rindi G, Klimstra DS, Abedi-Ardekani B, Asa SL, Bosman FT, Brambilla E, Busam KJ, de Krijger RR, Dietel M, El-Naggar AK, Fernandez-Cuesta L, Klöppel G, McCluggage WG, Moch H, Ohgaki H, Rakha EA, Reed NS, Rous BA, Sasano H, Scarpa A, Scoazec JY, Travis WD, Tallini G, Trouillas J, van Krieken JH, Cree IA (2018) A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod Pathol 31:1770-1786.
Salehi F, Agur A, Scheithauer BW, Kovacs K, Lloyd RV, Cusimano M (2009) Ki-67 in pituitary neoplasms: a review--part I. Neurosurgery 65:429-437.
Grimm F, Maurus R, Beschorner R, Naros G, Stanojevic M, Gugel I, Giese S, Bier G, Bender B, Honegger J (2019) Ki-67 labeling index and expression of p53 are non-predictive for invasiveness and tumor size in functional and nonfunctional pituitary adenomas. Acta Neurochir (Wien) 161:1149-1156.
Trouillas J, Roy P, Sturm N, et al (2013) A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol 126:123-135.
Mete O, Cintosun A, Pressman I, Asa SL (2018) Epidemiology and biomarker profile of pituitary adenohypophysial tumors. Mod Pathol 31: 900-909.
Almeida JP, Stephens CC, Eschbacher JM, Felicella MM, Yuen KCJ, White WL, Mooney MA, Bernat AL, Mete O, Zadeh G, Gentili F, Little AS (2019) Clinical, pathologic, and imaging characteristics of pituitary null cell adenomas as defined according to the 2017 World Health Organization criteria: a case series from two pituitary centers. Pituitary 22: 514-519.
Balogun JA, Monsalves E, Juraschka K, Parvez K, Kucharczyk W, Mete O, Gentili F, Zadeh G (2015) Null cell adenomas of the pituitary gland: an institutional review of their clinical imaging and behavioral characteristics. Endocr Pathol 26: 63-70.
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F, Asa SL, Zadeh G (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir (Wien) 154: 1493-1498
Guaraldi F, Zoli M, Righi A, Gibertoni D, Marino Picciola V, Faustini-Fustini M, Morandi L, Bacci A, Pasquini E, Mazzatenta D, Asioli S (2020) A practical algorithm to predict postsurgical recurrence and progression of pituitary neuroendocrine tumours (PitNET)s. Clin Endocrinol (Oxf) 93:36-43.
Asa SL, Mete O, Perry A, Osamura RY (2022) Overview of the 2022 WHO classification of pituitary tumors. Endocr Pathol 33:6-26.
Vanoli A, La Rosa S, Miceli E, Klersy C, Maragliano R, Capuano F, Persichella A, Martino M, Inzani F, Luinetti O, Di Sabatino A, Sessa F, Paulli M, Corazza GR, Rindi G, Bordi C, Capella C, Solcia E (2018) Prognostic evaluations tailored to specific gastric neuroendocrine neoplasms: Analysis of 200 cases with extended follow-up Neuroendocrinology 107:114–126.
WHO Classification of Tumours Editorial Board (2022). Head and neck tumours. WHO classification of tumours series, 5th ed.; vol. 9. International Agency for Research on Cancer, Lyon.
El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ (2017) WHO Classification of Head and Neck Tumours, 4th Edition. International Agency for Research on Cancer, Lyon.
Kao HL, Chang WC, Li WY, Chia-Heng Li A, Fen-Yau Li A (2012) Head and neck large cell neuroendocrine carcinoma should be separated from atypical carcinoid on the basis of different clinical features, overall survival, and pathogenesis. Am J Surg Pathol 36:185-192.
Shah K, Perez-Ordóñez B (2016) Neuroendocrine neoplasms of the sinonasal tract: neuroendocrine carcinomas and olfactory neuroblastoma. Head Neck Pathol 10:85-94.
Bal M, Sharma A, Rane SU, Mittal N, Chaukar D, Prabhash K, Patil A (2022) Neuroendocrine neoplasms of the larynx: a clinicopathologic analysis of 27 neuroendocrine tumors and neuroendocrine carcinomas. Head Neck Pathol 16:375-387.
Turri-Zanoni M, Maragliano R, Battaglia P, Giovannardi M, Antognoni P, Lombardi D, Morassi ML, Pasquini E, Tarchini P, Asioli S, Foschini MP, Sessa F, Nicolai P, Castelnuovo P, La Rosa S (2017) The clinicopathological spectrum of olfactory neuroblastoma and sinonasal neuroendocrine neoplasms: refinements in diagnostic criteria and impact of multimodal treatments on survival. Oral Oncol 74:21-29.
Classe M, Burgess A, El Zein S, Wassef M, Herman P, Mortuaire G, Leroy X, Malouf GG, Verillaud B (2019) Evaluating the prognostic potential of the Ki67 proliferation index and tumour-infiltrating lymphocytes in olfactory neuroblastoma. Histopathology 75:853-864.
Kakudo K, Wakasa T, Ohta Y, Yane K, Ito Y, Yamashita H (2015) Prognostic classification of thyroid follicular cell tumors using Ki-67 labeling index: risk stratification of thyroid follicular cell carcinomas. Endocr J 62:1-12.
Müller-Höcker J (1999) Immunoreactivity of p53, Ki-67, and Bcl 2 in oncocytic adenomas and carcinomas of the thyroid gland. Hum Pathol 30:926-933.
Erickson LA, Jin L, Wollan PC, Thompson GB, van Heerden J, Lloyd RV (1998) Expression of p27kip1 and Ki-67 in benign and malignant thyroid tumors. Mod Pathol 11:169-174.
Pisani T, Pantellini F, Centanni M, Vecchione A, Giovagnoli MR (2003) Immunocytochemical expression of Ki67 and laminin in Hurthle cell adenomas and carcinomas. Anticancer Res 23: 3323-3326.
Katoh R, Bray CE, Suzuki K, Komiyama A, Hemmi A, Kawaoi A, Oyama T, Sugai T, Sasou S (1995) Growth activity in hyperplastic and neoplastic human thyroid determined by an immunohistochemical staining procedure using monoclonal antibody MIB-1. Hum Pathol 26: 136-146.
Sofiadis A, Tani E, Foukakis T, Kjellman P, Skoog L, Höög A, Wallin G, Zedenius J, Larsson C (2009) Diagnostic and prognostic potential of MIB-1 proliferation index in thyroid fine needle aspiration biopsy. Int J Oncol 35: 369-374.
Cho Mar K, Eimoto T, Nagaya S, Tateyama H (2006) Cell proliferation marker MCM2, but not Ki67, is helpful for distinguishing between minimally invasive follicular carcinoma and follicular adenoma of the thyroid. Histopathol 48: 801-807.
Tan A, Etit D, Bayol U, Altinel D, Tan S (2011) Comparison of proliferating cell nuclear antigen, thyroid transcription factor-1, Ki-67, p63, p53 and high-molecular weight cytokeratin expressions in papillary thyroid carcinoma, follicular carcinoma, and follicular adenoma. Ann Diagn Pathol 15:108-116.
Hellgren LS, Stenman A, Paulsson JO, Höög A, Larsson C, Zedenius J, Juhlin CC (2022) Prognostic utility of the Ki-67 labeling index in follicular thyroid tumors: a 20-year experience from a tertiary thyroid center. Endocr Pathol 33:231-242.
Ito Y, Hirokawa M, Miyauchi A, Masuoka H, Yabuta T, Fukushima M, Kihara M, Higashiyama T, Kobayashi K, Miya A (2016) Prognostic impact of Ki-67 labeling index in minimally invasive follicular thyroid carcinoma. Endocr J 63:913-917.
Ito Y, Hirokawa M, Fujishima M, Masuoka H, Higashiyama T, Kihara M, Onoda N, Miya A, Miyauchi A (2021) Prognostic significance of vascular invasion and cell-proliferation activity in widely invasive follicular carcinoma of the thyroid. Endocr J 68:881-888.
Viana AOR, Gonçalves Filho J, Francisco ALN, Pinto CAL, Kowalski LP (2020) Ki-67 and CK-19 are predictors of locoregional recurrence in papillary thyroid carcinoma. Acta Otorhinolaryngol Ital 40:190-197.
Tang J, Gui C, Qiu S, Wang M (2018) The clinicopathological significance of Ki67 in papillary thyroid carcinoma: a suitable indicator? World J Surg Oncol 16: 100.
Matsuse M, Yabuta T, Saenko V, Hirokawa M, Nishihara E, Suzuki K, Yamashita S, Miyauchi A, Mitsutake N (2017) TERT Promoter mutations and Ki-67 labeling index as a prognostic marker of papillary thyroid carcinomas: combination of two independent factors. Sci.Rep 7:41752.
Hirokawa M, Matsuda K, Kudo T, Higuchi M, Suzuki A, Takada N, Nakashima M, Miyauchi A (2019) Cribriform-morular variant of papillary thyroid carcinoma shows high Ki-67 labeling indices, despite its excellent prognosis. Pathobiology 86:248-253.
Christofer Juhlin C, Mete O, Baloch ZW (2022) The 2022 WHO classification of thyroid tumors: novel concepts in nomenclature and grading. Endocr Relat Cancer 30: e220293.
Tallini G, Garcia-Rostan G, Herrero A, Zelterman D, Viale G, Bosari S, Carcangiu ML (1999) Downregulation of p27KIP1 and Ki67/Mib1 labeling index support the classification of thyroid carcinoma into prognostically relevant categories. Am J Surg Pathol 23:678-685.
Kjellman P, Wallin G, Höög A, Auer G, Larsson C, Zedenius J (2003) MIB-1 index in thyroid tumors: a predictor of the clinical course in papillary thyroid carcinoma. Thyroid 13:371-80.
Ito Y, Miyauchi A, Kakudo K, Hirokawa M, Kobayashi K, et al. (2010) Prognostic significance of Ki-67 labelling index in papillary carcinoma. World J Surg, 34: 3015-3021.
Fujishima M, Miyauchi A, Ito Y, Kudo T, Noda T, Sasaki T, Sano T, Ando T, Yamamoto M, Masuoka H, Higashiyama T, Kihara M, Hayashi T, Hirokawa M, Onoda N, Miya A (2013) Ki-67 labelling index is a predictor of postoperative persistent disease and cancer growth and prognostic indicator in papillary thyroid carcinoma. Eur Thyroid J 2:57-64.
Gnemmi V, Renaud F, Do Cao C, Salleron J, Lion G, Wemeau JL, Copin MC, Carnaille B, Leteurtre E, Pattou F, Aubert S (2014) Poorly differentiated thyroid carcinomas: application of the Turin proposal provides prognostic results similar to those from assessment of high-grade features. Histopathology 64:263-273.
Wells SA Jr, Asa SL, Dralle H, et al (2015) Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567-610.
Mathiesen JS, Kroustrup JP, Vestergaard P, Stochholm K, Poulsen PL, Rasmussen ÅK, Feldt-Rasmussen U, Schytte S, Londero SC, Pedersen HB, Hahn CH, Bentzen J, Möller S, Gaustadnes M, Rossing M, Nielsen FC, Brixen K, Frederiksen AL, Godballe C (2019) Survival and long-term biochemical cure in medullary thyroid carcinoma in Denmark 1997-2014: a nationwide study. Thyroid 29:368-377.
Ho AS, Wang L, Palmer FL, Yu C, Toset A, Patel S, Kattan MW, Tuttle RM, Ganly I (2015) Postoperative nomogram for predicting cancer-specific mortality in medullary thyroid cancer. Ann Surg Oncol 22:2700-2706.
Turkdogan S, Forest VI, Hier MP, Tamilia M, Florea A, Payne RJ (2018) Carcinoembryonic antigen levels correlated with advanced disease in medullary thyroid cancer. J Otolaryngol Head Neck Surg 47:55.
Moura MM, Cavaco BM, Pinto AE, Domingues R, Santos JR, Cid MO, Bugalho MJ, Leite V (2009) Correlation of RET somatic mutations with clinicopathological features in sporadic medullary thyroid carcinomas. Br J Cancer 100:1777-1783.
Fuchs TL, Nassour AJ, Glover A, Sywak MS, Sidhu SB, Delbridge LW, Clifton-Bligh RJ, Gild ML, Tsang V, Robinson BG, Clarkson A, Sheen A, Sioson L, Chou A, Gill AJ (2020) A proposed grading scheme for medullary thyroid carcinoma based on proliferative activity (Ki-67 and mitotic count) and coagulative necrosis. Am J Surg Pathol 44:1419-1428.
Alzumaili B, Xu B, Spanheimer PM, Tuttle RM, Sherman E, Katabi N, Dogan S, Ganly I, Untch BR, Ghossein RA (2020) Grading of medullary thyroid carcinoma on the basis of tumor necrosis and high mitotic rate is an independent predictor of poor outcome. Mod Pathol 33:1690-1701.
Xu B, Fuchs TL, Ahmadi S, Alghamdi M, Alzumaili B, Bani MA, Baudin E, Chou A, De Leo A, Fagin JA, Ganly I, Glover A, Hartl D, Kanaan C, Khneisser P, Najdawi F, Nigam A, Papachristos A, Repaci A, Spanheimer PM, Solaroli E, Untch BR, Barletta JA, Tallini G, Al Ghuzlan A, Gill AJ, Ghossein RA (2022) International medullary thyroid carcinoma grading system: a validated grading system for medullary thyroid carcinoma. J Clin Oncol 40:96-104.
Vissio E, Maletta F, Fissore J, Osella Abate S, Retta F, Brizzi MP, Piovesan A, Rossetto Giaccherino R, Volante M, Papotti M (2022) External validation of three available grading systems for medullary thyroid carcinoma in a single institution cohort. Endocr Pathol 33:359-370.
Williams JF, Zhao M, Najdawi F, Ahmadi S, Hornick JL, Wong KS, Barletta JA (2022) Grading of medullary thyroid carcinoma: an interobserver reproducibility study. Endocr Pathol 33:371-377.
Erickson LA, Mete O, Juhlin CC, Perren A, Gill AJ (2022) Overview of the 2022 WHO classification of parathyroid tumors. Endocr Pathol 33:64-89.
Davies MP, John Evans TW, Tahir F, Balasubramanian SP (2021) Parathyroid cancer: a systematic review of diagnostic biomarkers. Surgeon 19:e536-e548.
Abbona GC, Papotti M, Gasparri G, Bussolati G (1995) Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining. Hum Pathol 26:135-138.
Thomopoulou GE, Tseleni-Balafouta S, Lazaris AC, Koutselini H, Kavantzas N, Davaris PS (2003) Immunohistochemical detection of cell cycle regulators, Fhit protein and apoptotic cells in parathyroid lesions. Eur J Endocrinol 148:81-87.
Inic Z, Inic M, Jancic S, Paunovic I, Tatic S, Tausanovic K, Zivavljevic V, Zegarac M, Inic I, Dunjdjerovic D (2015) The relationship between proliferation activity and parathyroid hormone levels in parathyroid tumors. J BUON 20:562:566.
Uljanovs R, Sinkarevs S, Strumfs B, Vidusa L, Merkurjeva K, Strumfa I (2022) Immunohistochemical profile of parathyroid tumours: a comprehensive review. Int J Mol Sci 23:6981.
Erickson LA, Mete O (2018) Immunohistochemistry in diagnostic parathyroid pathology. Endocr Pathol 29:113-129.
Silva-Figueroa AM, Bassett R Jr, Christakis I, Moreno P, Clarke CN, Busaidy NL, Grubbs EG, Lee JE, Perrier ND, Williams MD (2019) Using a novel diagnostic nomogram to differentiate malignant from benign parathyroid neoplasms. Endocr Pathol 30:285-296.
Schulte JJ, Pease G, Taxy JB, Hall C, Cipriani NA (2021) Distinguishing parathyromatosis, atypical parathyroid adenomas, and parathyroid carcinomas utilizing histologic and clinical features. Head Neck Pathol 15:727-736.
Hu Y, Cui M, Chang X, Wang O, Chen T, Xiao J, Wang M, Hua S, Liao Q (2022) Patterns and predictors of cervical lymph node metastasis in parathyroid carcinoma. Cancers (Basel). 14:4004.
Pelosi G, Travis WD (2021) The Ki-67 antigen in the new 2021 World Health Organization classification of lung neuroendocrine neoplasms. Pathologica 113:377-387.
Pelosi G, Rodriguez J, Viale G (2005) Typical and atypical pulmonary carcinoid tumor overdiagnosed as small-cell carcinoma on biopsy specimens: a major pitfall in the management of lung cancer patients. Am J Surg Pathol 29:179-187.
Aslan DL, Gulbahce HE, Pambuccian SE (2005) Ki-67 immunoreactivity in the differential diagnosis of pulmonary neuroendocrine neoplasms in specimens with extensive crush artifact. Am J Clin Pathol 123:874-878.
Pelosi G, Rindi G, Travis WD (2014) Ki-67 antigen in lung neuroendocrine tumors: unraveling a role in clinical practice. J Thorac Oncol 9:273-284.
WHO Classification of Tumours Editorial Board (2021) Thoracic tumours. WHO classification of tumours series, 5th ed.; vol. 5): International Agency for Research on Cancer, Lyon.
Dermawan JKT, Farver CF (2020) The role of histologic grading and Ki-67 index in predicting outcomes in pulmonary carcinoid tumors. Am J Surg Pathol 44:224-231.
Rindi G, Klersy C, Inzani F, Fellegara G, Ampollini L, Ardizzoni A, Campanini N, Carbognani P, De Pas TM, Galetta D, Granone PL, Righi L, Rusca M, Spaggiari L, Tiseo M, Viale G, Volante M, Papotti M, Pelosi G (2013) Grading the neuroendocrine tumors of the lung: an evidence-based proposal. Endocr Relat Cancer 21:1-16.
Rekhtman N, Desmeules P, Litvak AM (2019) Stage IV lung carcinoids: spectrum and evolution of proliferation rate, focusing on variants with elevated proliferation indices. Mod Pathol 32:1106-1122.
Pelosi G, Massa F, Gatti G (2019) Ki-67 evaluation for clinical decision in metastatic lung carcinoids: a proof of concept. Clin Pathol 12:2632010X19829259.
Kasajima A, Konukiewitz B, Oka N (2019) Clinicopathological profiling of lung carcinoids with a Ki67 index > 20. Neuroendocrinology 108:109-120.
Pelosi G, Bianchi F, Hofman P (2019) Recent advances in the molecular landscape of lung neuroendocrine tumors. Expert Rev Mol Diagn 19:281-297.
Rekhtman N, Pietanza MC, Hellmann MD, Naidoo J, Arora A, Won H, Halpenny DF, Wang H, Tian SK, Litvak AM, Paik PK, Drilon AE, Socci N, Poirier JT, Shen R, Berger MF, Moreira AL, Travis WD, Rudin CM, Ladanyi M (2016) Next-generation sequencing of pulmonary large cell neuroendocrine carcinoma reveals small cell carcinoma-like and non-small cell carcinoma-like subsets. Clin Cancer Res 22:3618-3629.
Kasajima A, Kloppel G (2022) Neuroendocrine tumor G3 of bronchopulmonary origin and its classification. Pathol Int 2:488-495.
Klimstra DS, Klöppel G, La Rosa S, Rindi G (2019) Classification of neuroendocrine neoplasms of the digestive system. In: WHO Classification of Tumours Editorial Board. Digestive system tumours. WHO classification of tumours series, 5th ed.; vol. 1. International Agency for Research on Cancer, Lyon (France), pp 16–19.
Marchiò C, Gatti G, Massa F, Bertero L, Filosso P, Pelosi G, Cassoni P, Volante M, Papotti M (2017) Distinctive pathological and clinical features of lung carcinoids with high proliferation index. Virchows Arch 471:713-720.
Garg R, Bal A, Das A (2019) Proliferation marker (Ki67) in sub-categorization of neuroendocrine tumours of the lung. Turk Patoloji Derg 35:15-21.
Grimaldi F, Muser D, Beltrami CA (2011) Partitioning of bronchopulmonary carcinoids in two different prognostic categories by Ki-67 score. Front Endocrinol (Lausanne) 2:20.
Joseph MG, Shibani A, Panjwani N (2015) Usefulness of Ki-67, mitoses, and tumor size for predicting metastasis in carcinoid tumors of the lung: a study of 48 cases at a Tertiary Care Centre in Canada. Lung Cancer Int 2015:545601.
Marchevsky AM, Hendifar A, Walts AE (2018) The use of Ki-67 labeling index to grade pulmonary well-differentiated neuroendocrine neoplasms: current best evidence. Mod Pathol 31:1523-1531.
Chetty R (2008) Requiem for the term 'carcinoid tumour' in the gastrointestinal tract? Can J Gastroenterol 22:357-358.
Zaleski M, Kalhor N, Moran CA (2021) Typical and atypical carcinoid tumors of the mediastinum: a biomarker analysis of 27 cases with clinical correlation. Int J Surg Pathol 29: 358-367.
Crona J, Björklund P, Welin S, Kozlovacki G, Oberg K, Granberg D (2013) Treatment, prognostic markers and survival in thymic neuroendocrine tumours. a study from a single tertiary referral centre. Lung Cancer 79: 289-293.
Rindi G, Klöppel G, Alhman H, et al (2006) TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch 449:395-401
Rindi G, Klöppel G, Couvelard A, Komminoth P, Körner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A, Scoazec JY, Wiedenmann B (2007) TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch 451:757-762.
Klöppel G, La Rosa S (2018) Ki67 labeling index: assessment and prognostic role in gastroenteropancreatic neuroendocrine neoplasms. Virchows Arch 472:341-349.
Bosman FT, Carneiro F, Hruban RH, Theise ND (eds) (2010) WHO Classification of Tumours of the Digestive System, 4th Edition. IARC, Lyon
Rindi G, Mete O, Uccella S, Basturk O, La Rosa S, Brosens LAA, Ezzat S, de Herder WW, Klimstra DS, Papotti M, Asa SL (2022) Overview of the 2022 WHO classification of neuroendocrine neoplasms. Endocr Pathol 33:115-154.
La Rosa S, Solcia E (2020) New insights into the classification of gastric neuroendocrine tumours, expanding the spectrum of ECL-cell tumours related to hypergastrinaemia. Histopathology 77:862-864.
Trinh VQ, Shi C, Ma C (2020) Gastric neuroendocrine tumours from long-term proton pump inhibitor users are indolent tumours with good prognosis. Histopathology 77:865-876.
Vanoli A, La Rosa S, Klersy C, Grillo F, Albarello L, Inzani F, Maragliano R, Manca R, Luinetti O, Milione M, Doglioni C, Rindi G, Capella C, Solcia E (2017) Four neuroendocrine tumor types and neuroendocrine carcinoma of the duodenum: analysis of 203 cases. Neuroendocrinology 104:112-125.
Vanoli A, Grami O, Klersy C, Milanetto AC, Albarello L, Fassan M, Luchini C, Grillo F, Spaggiari P, Inzani F, Uccella S, Parente P, Nappo G, Mattiolo P, Milione M, Pietrabissa A, Cobianchi L, Schiavo Lena M, Partelli S, Di Sabatino A, Sempoux C, Capella C, Pasquali C, Doglioni C, Sessa F, Scarpa A, Rindi G, Paulli M, Zerbi A, Falconi M, Solcia E, La Rosa S (2022) Ampullary neuroendocrine neoplasms: identification of prognostic factors in a multicentric series of 119 cases. Endocr Pathol 33:274-288.
Ryu DG, Kim SJ, Choi CW, Kang DH, Kim HW, Park SB, Nam HS, Lee SH, Hwang SH (2022). Clinical outcomes of gastroduodenal neuroendocrine tumors according to their WHO grade: a single-institutional retrospective analysis. Medicine (Baltimore) 101:e30397.
Strosberg JR, Weber JM, Feldman M, Coppola D, Meredith K, Kvols LK (2013) Prognostic validity of the American Joint Committee on Cancer staging classification for midgut neuroendocrine tumors J Clin Oncol 31:420-425.
Araujo PB, Cheng S, Mete O, Serra S, Morin E, Asa SL, Ezzat S (2013) Evaluation of the WHO 2010 grading and AJCC/UICC staging systems in prognostic behavior of intestinal neuroendocrine tumors PloS One 8:e61538.
Panzuto F, Campana D, Fazio N, Brizzi MP, Boninsegna L, Nori F, Di Meglio G, Capurso G, Scarpa A, Dogliotti L, De Braud F, Tomassetti P, Delle Fave G, Falconi M (2012) Risk factors for disease progression in advanced jejunoileal neuroendocrine tumors. Neuroendocrinology 96:32-40.
Volante M, Daniele L, Asioli S, Cassoni P, Comino A, Coverlizza S, De Giuli P, Fava C, Manini C, Berruti A, Papotti M (2013) Tumor staging but not grading is associated with adverse clinical outcome in neuroendocrine tumors of the appendix: a retrospective clinical pathologic analysis of 138 cases. Am J Surg Pathol 37:606-612.
Rault-Petit B, Do Cao C, Guyétant S, Guimbaud R, Rohmer V, Julié C, Baudin E, Goichot B, Coriat R, Tabarin A, Ramos J, Goudet P, Hervieu V, Scoazec JY, Walter T (2019) Current management and predictive factors of lymph node metastasis of appendix neuroendocrine tumors: a national study from the French Group of Endocrine Tumors (GTE). Ann Surg 270:165-171.
Brighi N, La Rosa S, Rossi G, Grillo F, Pusceddu S, Rinzivillo M, Spada F, Tafuto S, Massironi S, Faggiano A, Antonuzzo L, Santini D, Sessa F, Maragliano R, Gelsomino F, Albertelli M, Vernieri C, Panzuto F, Fazio N, De Divitiis C, Lamberti G, Colao A, Fave GD, Campana D (2020) Morphological factors related to nodal metastases in neuroendocrine tumors of the appendix: a multicentric retrospective study. Ann Surg 271:527-533.
Hong SM, Kim YS, Moon JS, Kim JN, Oh MK, Kwon SO, Jeong SY, Hong SW, Kang YK (2013) Prognostic significance of Ki-67 expression in rectal carcinoid tumors Korean J Gastroenterol 61:82–87.
Jernman J, Valimaki MJ, Louhimo J, Haglund C, Arola J (2012) The novel WHO 2010 classification for gastrointestinal neuroendocrine tumours correlates well with the metastatic potential of rectal neuroendocrine tumours Neuroendocrinology 95:317–324.
Sugimoto S, Hotta K, Shimoda T, Imai K, Yamaguchi Y, Nakajima T, Oishi T, Mori K, Takizawa K, Kakushima N, Tanaka M, Kawata N, Matsubayashi H, Ono H (2016) The Ki-67 labeling index and lymphatic/venous permeation predict the metastatic potential of rectal neuroendocrine tumors Surg Endosc 30:4239–4248.
Sohn JH, Cho MY, Park Y, et al (2015) Prognostic significance of defining L-cell type on the biologic behavior of rectal neuroendocrine tumors in relation with pathological parameters. Cancer Res Treat 47:813-822.
Rindi G, Falconi M, Klersy C, Albarello L, Boninsegna L, Buchler MW, Capella C, Caplin M, Couvelard A, Doglioni C, Delle Fave G, Fischer L, Fusai G, de Herder WW, Jann H, Komminoth P, de Krijger RR, La Rosa S, Luong TV, Pape U, Perren A, Ruszniewski P, Scarpa A, Schmitt A, Solcia E, Wiedenmann B (2012) TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst 104:764-777.
Rindi G, Klersy C, Albarello L, Baudin E, Bianchi A, Buchler MW, Caplin M, Couvelard A, Cros J, de Herder WW, Delle Fave G, Doglioni C, Federspiel B, Fischer L, Fusai G, Gavazzi F, Hansen CP, Inzani F, Jann H, Komminoth P, Knigge UP, Landoni L, La Rosa S, Lawlor RT, Luong TV, Marinoni I, Panzuto F, Pape UF, Partelli S, Perren A, Rinzivillo M, Rubini C, Ruszniewski P, Scarpa A, Schmitt A, Schinzari G, Scoazec JY, Sessa F, Solcia E, Spaggiari P, Toumpanakis C, Vanoli A, Wiedenmann B, Zamboni G, Zandee WT, Zerbi A, Falconi M (2018). Competitive testing of the WHO 2010 versus the WHO 2017 grading of pancreatic neuroendocrine neoplasms: data from a large international cohort study. Neuroendocrinology 107:375-386.
Simbolo M, Bilotta M, Mafficini A, Luchini C, Furlan D, Inzani F, Petrone G, Bonvissuto D, La Rosa S, Schinzari G, Bianchi A, Rossi E, Menghi R, Giuliante F, Boccia S, Scarpa A, Rindi G (2021) Gene expression profiling of pancreas neuroendocrine tumors with different ki67-based grades. Cancers (Basel) 13:2054
Weiss LM (1984) Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors. Am J Surg Pathol 8:163-169.
Duregon E, Fassina A, Volante M, Nesi G, Santi R, Gatti G, Cappellesso R, Dalino Ciaramella P, Ventura L, Gambacorta M, Dei Tos AP, Loli P, Mannelli M, Mantero F, Berruti A, Terzolo M, Papotti M (2013) The reticulin algorithm for adrenocortical tumor diagnosis: a multicentric validation study on 245 unpublished cases. Am J Surg Pathol 37:1433-1440.
Bisceglia M, Ludovico O, Di Mattia A, Ben-Dor D, Sandbank J, Pasquinelli G, Lau SK, Weiss LM (2004) Adrenocortical oncocytic tumors: report of 10 cases and review of the literature. Int J Surg Pathol 12:231-243.
Wieneke JA, Thompson LD, Heffess CS (2003) Adrenal cortical neoplasms in the pediatric population: a clinicopathologic and immunophenotypic analysis of 83 patients. Am J Surg Pathol 27:867-881.
Pennanen M, Heiskanen I, Sane T, Remes S, Mustonen H, Haglund C, Arola J (2015) Helsinki score-a novel model for prediction of metastases in adrenocortical carcinomas. Hum Pathol 46:404-410.
Duregon E, Cappellesso R, Maffeis V, Zaggia B, Ventura L, Berruti A, Terzolo M, Fassina A, Volante M, Papotti M (2017) Validation of the prognostic role of the "Helsinki Score" in 225 cases of adrenocortical carcinoma. Hum Pathol 62:1-7.
Wachenfeld C, Beuschlein F, Zwermann O, Mora P, Fassnacht M, Allolio B, Reincke M (2001) Discerning malignancy in adrenocortical tumors: are molecular markers useful? Eur J Endocrinol 145:335-341.
Picard C, Orbach D, Carton M, Brugieres L, Renaudin K, Aubert S, Berrebi D, Galmiche L, Dujardin F, Leblond P, Thomas-Teinturier C, Dijoud F (2019) Revisiting the role of the pathological grading in pediatric adrenal cortical tumors: results from a national cohort study with pathological review. Mod Pathol 32:546-559.
Martins-Filho SN, Almeida MQ, Soares I, Wakamatsu A, Alves VAF, Fragoso MCBV, Zerbini MCN (2021). Clinical impact of pathological features including the Ki-67 labeling index on diagnosis and prognosis of adult and pediatric adrenocortical tumors. Endocr Pathol 32:288-300.
Mete O, Erickson LA, Juhlin CC, de Krijger RR, Sasano H, Volante M, Papotti MG (2022) Overview of the 2022 WHO classification of adrenal cortical tumors. Endocr Pathol 33:155-196.
Duregon E, Molinaro L, Volante M, Ventura L, Righi L, Bolla S, Terzolo M, Sapino A, Papotti MG (2014) Comparative diagnostic and prognostic performances of the hematoxylin-eosin and phospho-histone H3 mitotic count and Ki-67 index in adrenocortical carcinoma. Mod Pathol 27:1246-1254
Mete O, Gucer H, Kefeli M, Asa SL (2018) Diagnostic and Prognostic Biomarkers of Adrenal Cortical Carcinoma. Am J Surg Pathol 42: 201-213.
Fassnacht M, Dekkers OM, Else T, Baudin E, Berruti A, de Krijger R, Haak HR, Mihai R, Assie G, Terzolo M (2018) European Society of Endocrinology clinical practice guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 179:G1-G46.
Tőke J, Uhlyarik A, Lohinszky J, Stark J, Huszty G, Micsik T, Borka K, Reismann P, Horányi J, Igaz P, Tóth M (2022) Prognostic factors and mitotane treatment of adrenocortical cancer. Two decades of experience from an institutional case series. Front Endocrinol (Lausanne) 13: 952418.
Tavangar SM, Shojaee A, Moradi Tabriz H, Haghpanah V, Larijani B, Heshmat R, Lashkari A, Azimi S (2010) Immunohistochemical expression of Ki67, c-erbB-2, and c-kit antigens in benign and malignant pheochromocytoma. Pathol Res Pract 206:305-309.
August C, August K, Schroeder S, Bahn H, Hinze R, Baba HA, Kersting C, Buerger H (2004) CGH and CD 44/MIB-1 immunohistochemistry are helpful to distinguish metastasized from nonmetastasized sporadic pheochromocytomas. Mod Pathol 17:1119-1128.
Elder EE, Xu D, Höög A, Enberg U, Hou M, Pisa P, Gruber A, Larsson C, Bäckdahl M (2003) Ki-67 and hTERT expression can aid in the distinction between malignant and benign pheochromocytoma and paraganglioma. Mod Pathol 16:246-255.
Wang LL, Wei XJ, Zhang QC, Li F (2022) Morphological and immunohistochemical characteristics associated with metastatic and recurrent progression in pheochromocytoma/paraganglioma: a cohort study. Ann Diagn Pathol 60: 151981.
Thompson LD (2002) Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol 26:551-566.
Kimura N, Takayanagi R, Takizawa N, et al (2014) Pathological grading for predicting metastasis in phaeochromocytoma and paraganglioma. Endocr Relat Cancer 21:405-414.
Pierre C, Agopiantz M, Brunaud L, Battaglia-Hsu SF, Max A, Pouget C, Nomine C, Lomazzi S, Vignaud JM, Weryha G, Oussalah A, Gauchotte G, Busby-Venner H (2019) COPPS, a composite score integrating pathological features, PS100 and SDHB losses, predicts the risk of metastasis and progression-free survival in pheochromocytomas/paragangliomas. Virchows Arch. 474:721-734.
Mete O, Asa SL, Gill AJ, Kimura N, de Krijger RR, Tischler A (2022) Overview of the 2022 WHO classification of paragangliomas and pheochromocytomas. Endocr Pathol 33:90-114.
Thompson LDR, Gill AJ, Asa SL, Clifton-Bligh RJ, de Krijger RR, Kimura N, Komminoth P, Lack EE, Lenders JWM, Lloyd RV, Papathomas TG, Sadow PM, Tischler AS (2021) Data set for the reporting of pheochromocytoma and paraganglioma: explanations and recommendations of the guidelines from the International Collaboration on Cancer Reporting. Hum Pathol 110:83-97.
WHO Classification of Tumours Editorial Board (2022) Urinary and male genital tumours. WHO classification of tumours series, 5th ed.; vol. 8. International Agency for Research on Cancer, Lyon.
Aung PP, Killian K, Poropatich CO, Linehan WM, Merino MJ (2013) Primary neuroendocrine tumors of the kidney: morphological and molecular alterations of an uncommon malignancy. Hum Pathol 44: 873-880.
Kim B, Kim HS, Moon KC (2019) Primary renal well-differentiated neuroendocrine tumors: report of six cases with an emphasis on the Ki-67 index and mitosis. Diagn Pathol. 14: 12.
WHO genitale femminile WHO Classification of Tumours Editorial Board (2020) Female genital tumours. WHO classification of tumours series, 5th ed.; vol. 4. International Agency for Research on Cancer, Lyon.
Katafuchi T, Kawakami F, Iwagoi Y, Saito F, Mikami Y (2022) "Neuroendocrine tumor grade 3 (NET G3)" of the uterine cervix: a report of 2 cases. Int J Gynecol Pathol 41: 470-475.
Rouzbahman M, Clarke B (2013) Neuroendocrine tumors of the gynecologic tract: select topics. Semin Diagn Pathol 30: 224-233.
Opalińska M, Sowa-Staszczak A, Olearska H, Ulatowska-Bialas M, Gilis-Januszewska A, Hubalewska-Dydejczyk A (2021) Clinical Approach to Neuroendocrine Neoplasm Associated With Ovarian Teratoma. Front Endocrinol (Lausanne) 12: 770266.
Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K, Birkemeyer E, Thiis-Evensen E, Biagini M, Gronbaek H, Soveri LM, Olsen IH, Federspiel B, Assmus J, Janson ET, Knigge U (2013) Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol 24: 152-160.
Milione M, Maisonneuve P, Spada F, Pellegrinelli A, Spaggiari P, Albarello L, Pisa E, Barberis M, Vanoli A, Buzzoni R, Pusceddu S, Concas L, Sessa F, Solcia E, Capella C, Fazio N, La Rosa S (2017) The clinicopathologic heterogeneity of grade 3 gastroenteropancreatic neuroendocrine neoplasms: morphological differentiation and proliferation identify different prognostic categories. Neuroendocrinology 104:85-93.
La Rosa S, Bonzini M, Sciarra A, Asioli S, Maragliano R, Arrigo M, Foschini MP, Righi A, Maletta F, Motolese A, Papotti M, Sessa F, Uccella S (2020) exploring the prognostic role of ki67 proliferative index in merkel cell carcinoma of the skin: clinico-pathologic analysis of 84 cases and review of the literature. Endocr Pathol 31:392-400.
Pelosi G, Rindi G, Travis WD, Papotti M (2014) Ki-67 antigen in lung neuroendocrine tumors: unraveling a role in clinical practice. J Thorac Oncol 9:273-284.
Adsay V (2012) Ki67 labeling index in neuroendocrine tumors of the gastrointestinal and pancreatobiliary tract: to count or not to count is not the question, but rather how to count Am J Surg Pathol 36:1743–1746.
Reid MD, Bagci P, Ohike N, Saka B, Erbarut Seven I, Dursun N, Balci S, Gucer H, Jang KT, Tajiri T, Basturk O, Kong SY, Goodman M, Akkas G, Adsay V (2015) Calculation of the Ki67 index in pancreatic neuroendocrine tumors: a comparative analysis of four counting methodologies Mod Pathol 28:686–694.
Tang LH, Gonen M, Hedvat C, Modlin IM, Klimstra DS (2012) Objective quantification of the Ki67 proliferative index in neuroendocrine tumors of the gastroenteropancreatic system: a comparison of digital image analysis with manual methods Am J Surg Pathol 36:1761–1770.
Cree IA (2022) From counting mitoses to Ki67 assessment: technical pitfalls in the new who classification of endocrine and neuroendocrine tumors. Endocr Pathol 33:3-5.
Blank A, Wehweck L, Marinoni I, Boos LA, Bergmann F, Schmitt AM, Perren A (2015) Interlaboratory variability of MIB1 staining in well-differentiated pancreatic neuroendocrine tumors Virchows Arch 467:543–550.
La Rosa S, Volante M, Uccella S, Maragliano R, Rapa I, Rotolo N, Inzani F, Siciliani A, Granone P, Rindi G, Dominioni L, Capella C, Papotti M, Sessa F, Imperatori A (2019) ACTH-producing tumorlets and carcinoids of the lung: clinico-pathologic study of 63 cases and review of the literature. Virchows Arch 475:587-597.
Funding
Open access funding provided by Università degli Studi dell'Insubria within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Not applicable.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
La Rosa, S. Diagnostic, Prognostic, and Predictive Role of Ki67 Proliferative Index in Neuroendocrine and Endocrine Neoplasms: Past, Present, and Future. Endocr Pathol 34, 79–97 (2023). https://doi.org/10.1007/s12022-023-09755-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-023-09755-3