Abstract
Purpose
Type-2 diabetes Mellitus (T2DM) is one of the leading causes of death and disability worldwide. This study examines temporal patterns of the global, regional, and national burden of T2DM in the last three decades.
Data and methods
The estimates of age, sex and location-wise incident cases, deaths, prevalent cases, and disability-adjusted-life-years (DALYs) and risk factors for 21 regions and 204 countries are retrieved from the Global Burden of Disease 2019 study from 1990 to 2019. Socio-demographic index (SDI) is used as the indicator of the development status of countries, and quadratic regression is employed to examine the relationship between country-level age-standardized rates and SDI.
Results
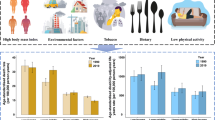
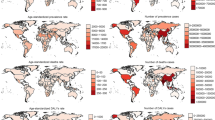
Globally, incident cases of T2DM more than doubled from 8.4 million[95% uncertainty interval, 7.8–9.1 million] in 1990 to 21.7 million[20.0–23.5 million] in 2019, and deaths more than doubled from 606,407[573,069–637,508] to 1.5 million[1.4–1.6 million] between 1990 and 2019. Global T2DM prevalence increased from 148.4 million[135.5–162.6 million] in 1990 to 437.9 million[402.0–477.0 million] in 2019. In 2019, global age-standardized prevalence rate stood at 5282.8/100,000[4853.6–5752.1], varying from 2174.5/100,000[1924.3–2470.5] in Mongolia to 19876.8/100,000[18211.1–21795.3] in American Samoa. SDI exhibited inverted-U shaped relationship with country-level age-standardised rates. Globally, high body-mass-index (51.9%), ambient particulate matter pollution (13.6%), smoking (9.9%) and secondhand smoke (8.7%) were the major contributing risk factors towards T2DM DALYs in 2019.
Conclusion
With ubiquitously rising prevalent cases globally, particularly in low and middle-income countries and regions, T2DM requires immediate attention and targeted policy response worldwide centered on lifestyle interventions (e.g., physical activity, smoking, diet, and obesity), air pollution control and cost-effective timely treatment.






Similar content being viewed by others
Data availability
All data is procured from GBD Results Tool http://ghdx.healthdata.org/gbd-results-tool.
References
IDF Atlas Ninth Edition (2019). Available at https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf. Accessed 13.3.2021
G.M. Reaven, Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37, 1595–1607 (1988)
C. Weyer, C. Bogardus, D.M. Mott, R.E. Pratley, The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J. Clin. Invest 104, 787–794 (1999)
The Emerging Risk Factors Collaboration, Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375, 2215–22 (2010)
Y. Zheng, S.H. Ley, F.B. Hu, Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14(2), 88 (2018)
C. Bommer, E. Heesemann, V. Sagalova, J. Manne-Goehler, R. Atun, T. Bärnighausen et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 5(6), 423–30 (2017)
WHO. Global action plan for the prevention and control of noncommunicable diseases 2013–20 (2013). Available at https://www.who.int/publications/i/item/9789241506236. Accessed April 16, 2022
T. Vos, S.S. Lim, C. Abbafati et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1204–22 (2020)
H. Wang, K.M. Abbas, M. Abbasifard et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the global burden of disease study 2019. Lancet 396, 1160–203 (2020)
C.J. Murray, Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull. World health Org. 72(3), 429–445 (1994)
B. Zhou, Y. Lu, K. Hajifathalian et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4· 4 million participants. Lancet 387(10027), 1513–30 (2016)
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle: Institute for Health Metrics and Evaluation (IHME). Source: Institute for Health Metrics Evaluation. Used with permission. All rights reserved. Available from http://ghdx.healthdata.org/gbd-results-tool. Accessed: Jan–Feb 2021
K.J. Foreman, R. Lozano, A.D. Lopez, C.J. Murray, Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 10(1), 1 (2012)
C.J. Murray, A.Y. Aravkin, P. Zheng et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1223–49 (2020)
A. Nordström, J. Hadrévi, T. Olsson, P.W. Franks, P. Nordström, Higher prevalence of type 2 diabetes in men than in women is associated with differences in visceral fat mass. J. Clin. Endocrinol. Metab. 101(10 Oct), 3740–6 (2016)
J. Logue, J.J. Walker, H.M. Colhoun, G.P. Leese, R.S. Lindsay, J.A. McKnight, A.D. Morris, D.W. Pearson, J.R. Petrie, S. Philip, S.H. Wild, Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia 54(12), 3003–6 (2011)
F.E. von Eyben, E. Mouritsen, J. Holm et al. Intra-abdominal obesity and metabolic risk factors: a study of young adults. Int J. Obes. Relat. Metab. Disord. 27, 941–949 (2003)
A. Chandra, I.J. Neeland, J.D. Berry et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas Heart Study. J. Am. Coll. Cardiol. 64, 997–1002 (2014)
P. Wiklund, F. Toss, L. Weinehall et al. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J. Clin. Endocrinol. Metab. 93, 4360–4366 (2008)
B. Tramunt, S. Smati, N. Grandgeorge, F. Lenfant, J.F. Arnal, A. Montagner, P. Gourdy, Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 63(3 Mar), 453–61 (2020)
F. Mauvais-Jarvis, Sex differences in metabolic homeostasis, diabetes, and obesity. Biol. Sex. Differ. 6, 14 (2015)
J.C. Chen et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301, 2129–2140 (2009)
S.H. Ley, O. Hamdy, V. Mohan, F.B. Hu, Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 383(9933), 1999–2007 (2014)
A. Majeed, A.A. El-Sayed, T. Khoja, R. Alshamsan, C. Millett, S. Rawaf, Diabetes in the Middle-East and North Africa: an update. Diabetes Res Clin. Pr. 103(2), 218–22 (2014)
Y. Li, Y. He, L. Qi, V.W. Jaddoe, E.J. Feskens, X. Yang et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes 59(10), 2400–6 (2010)
L. Chen, D.J. Magliano, P.Z. Zimmet, The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat. Rev. Endocrinol. 8(4), 228–36 (2012)
D. Dabelea, E.J. Mayer-Davis, S. Saydah, G. Imperatore, B. Linder, J. Divers et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 311(17), 1778–86 (2014)
T. Reinehr, Type 2 diabetes mellitus in children and adolescents. World J. diabetes 4(6), 270 (2013)
J. Holmes, E. Gear, J. Bottomley, S. Gillam, M. Murphy, R. Williams, Do people with type 2 diabetes and their carers lose income? (T2ARDIS-4). Health Policy 64(3), 291–6 (2003)
X. Liu, C. Zhu, Will knowing diabetes affect labor income? Evidence from a natural experiment. Econ. Lett. 124, 74–8 (2014)
T. Seuring, O. Archangelidi, M. Suhrcke, The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics 33, 811–31 (2015)
R.J. Rubin, W.M. Altman, D.N. Mendelson, Health care expenditures for people with diabetes mellitus, 1992. J. Clin. Endocrinol. Metab. 78(4), 809A-F (1994)
F.B. Hu et al. Diet, Lifestyle, and the risk of type 2 diebetes mellitus in women. N. Eng. J. Med 345, 790–97 (2001)
E.S. Schellenberg, D.M. Dryden, B. Vandermeer, C. Ha, C. Korownyk, Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann. Intern Med 159(8), 543–51 (2013)
C. Merlotti, A. Morabito, A.E. Pontiroli, Prevention of type 2 diabetes; a systematic review and meta-analysis of different intervention strategies. Diabetes Obes. Metab. 16, 719–27 (2014)
Diabetes Prevention Program Research Group, Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 3, 866–75 (2015)
Global Health Observatory data repository. Prevalence of overweight among adults, BMI ≥ 25, age-standardized. Available at http://apps.who.int/gho/data/view.main.CTRY2430A?lang=en. Accessed 26 Feb 2020
T. Kelly, W. Yang, C.S. Chen, K. Reynolds, J. He, Global burden of obesity in 2005 and projections to 2030. Int J. Obes. 32(9), 1431–7 (2008)
E.V. Balti, J.B. Echouffo-Tcheugui, Y.Y. Yako, A.P. Kengne, Air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin. Pr. 106(2), 161–72 (2014)
G. Weinmayr, F. Hennig, K. Fuks, M. Nonnemacher, H. Jakobs, S. Möhlenkamp, R. Erbel, K.H. Jöckel, B. Hoffmann, S. Moebus, Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ. Health 14(1), 1–8 (2015)
C. Liu, C. Yang, Y. Zhao, Z. Ma, J. Bi, Y. Liu, X. Meng, Y. Wang, J. Cai, H. Kan, R. Chen, Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ. Int. 92, 416–21 (2016)
S. Zhang, S. Mwiberi, R. Pickford, S. Breitner, C. Huth, W. Koenig, W. Rathmann, C. Herder, M. Roden, J. Cyrys, A. Peters, Longitudinal associations between ambient air pollution and insulin sensitivity: results from the KORA cohort study. Lancet Planet. Health 5(1), e39–49 (2021)
T. Liu, X. Chen, Y. Xu, W. Wu, W. Tang, Z. Chen, G. Ji, J. Peng, Q. Jiang, J. Xiao, X. Li, Gut microbiota partially mediates the effects of fine particulate matter on type 2 diabetes: evidence from a population-based epidemiological study. Environ. Int. 130, 104882 (2019)
T.L. Alderete, R. Habre, C.M. Toledo-Corral, K. Berhane, Z. Chen, F.W. Lurmann, M.J. Weigensberg, M.I. Goran, F.D. Gilliland, Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino children. Diabetes 66(7), 1789–96 (2017)
C. Willi, P. Bodenmann, W.A. Ghali, P.D. Faris, J. Cornuz, Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298(22), 2654–64 (2007)
L. Zhang, G.C. Curhan, F.B. Hu, E.B. Rimm, J.P. Forman, Association between passive and active smoking and incident type 2 diabetes in women. Diabetes care 34(4), 892–7 (2011)
A. Pan, Y. Wang, M. Talaei, F.B. Hu, T. Wu, Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 3(12), 958–67 (2015)
T.K. Houston, S.D. Person, M.J. Pletcher, K. Liu, C. Iribarren, C.I. Kiefe, Active and passive smoking and development of glucose intolerance among young adults in a prospective cohort: CARDIA study. Bmj 332(7549), 1064–9 (2006)
B. Zhu, X. Wu, X. Wang, Q. Zheng, G. Sun, The association between passive smoking and type 2 diabetes: a meta-analysis. Asia Pac. J. Public Health 26(3), 226–37 (2014)
X. Wei, E. Meng, S. Yu, A meta-analysis of passive smoking and risk of developing Type 2 Diabetes Mellitus. Diabetes Res Clin. Pr. 107(1), 9–14 (2015)
S. Oba, A. Goto, T. Mizoue, M. Inoue, N. Sawada, M. Noda, S. Tsugane, Passive smoking and type 2 diabetes among never‐smoking women: The Japan Public Health Center‐based Prospective Study. J. Diabetes Investig. 11(5), 1352–8 (2020)
Y. Hayashino, S. Fukuhara, T. Okamura, H. Yamato, H. Tanaka, T. Tanaka, T. Kadowaki, H. Ueshima, A prospective study of passive smoking and risk of diabetes in a cohort of workers: the High-Risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) study. Diabetes care 31(4), 732–4 (2008)
S.G. Wannamethee, C.A. Camargo, J.E. Manson, W.C. Willett, E.B. Rimm, Alcohol drinking patterns and risk of type 2 diabetes mellitus among younger women. Arch. Intern. Med. 163(11 Jun), 1329–36 (2003)
S. Carlsson, N. Hammar, V. Grill, Alcohol consumption and type 2 diabetes. Diabetologia 48(6 Jun), 1051–4 (2005)
D.O. Baliunas, B.J. Taylor, H. Irving, M. Roerecke, J. Patra, S. Mohapatra, J. Rehm, Alcohol as a risk factor for type 2 diabetes: a systematic review and meta-analysis. Diabetes care 32(11), 2123–32 (2009)
A. Pietraszek, S. Gregersen, K. Hermansen, Alcohol and type 2 diabetes. A review. Nutr., Metab. Cardiovascular Dis. 20(5 Jun), 366–75 (2010)
X.H. Li, F.F. Yu, Y.H. Zhou, J. He, Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Am. J. Clin. Nutr. 103(3 Mar), 818–29 (2016)
P. Zimmet, K.G. Alberti, D.J. Magliano, P.H. Bennett, Diabetes mellitus statistics on prevalence and mortality: facts and fallacies. Nat. Rev. Endocrinol. 12(10), 616 (2016)
Z.J. Andersen, O. Raaschou-Nielsen, M. Ketzel, S.S. Jensen, M. Hvidberg, S. Loft, A. Tjønneland, K. Overvad, M. Sørensen, Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes care 35(1), 92–8 (2012)
Acknowledgements
We thank Institute of Health Metrics and Evaluation for providing GBD 2019 estimates in the public domain.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent for publication
The authors of the study have consent and responsibility for submission to the journal.
Ethical approval and consent to participate
The research was conducted using data available in the public domain and did not include any human participants or animals. Therefore, no ethical approvals were required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nanda, M., Sharma, R., Mubarik, S. et al. Type-2 Diabetes Mellitus (T2DM): Spatial-temporal Patterns of Incidence, Mortality and Attributable Risk Factors from 1990 to 2019 among 21 World Regions. Endocrine 77, 444–454 (2022). https://doi.org/10.1007/s12020-022-03125-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03125-5