Abstract
Purpose
A phenotype of metabolically healthy obesity (MHO) has been described in youth with obesity, but data are still scarce in this age group. The aim of the current study was to describe and compare clinical and laboratory parameters related to obesity among three different groups of youth, namely youth with normal weight (NW), with MHO, and with metabolically unhealthy obesity (MUO).
Methods
One hundred and three youngsters with obesity were divided according to 2018 consensus-based criteria into those with MHO [n = 49, age (±SD): 10.9 ± 2.9 years] and those with MUO [n = 54, 11.5 ± 2.7 years] and were compared to age-, sex- and Tanner-matched NW [n = 69, 11.3 ± 2.9 years]. Several obesity-related parameters were investigated for all three groups of children. Comparisons were made by analysis of variance (ANOVA) followed by the Fisher’s PLSD test.
Results
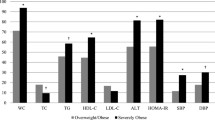
Youth with MHO had lower systolic (p < 0.001) and diastolic (p < 0.01) blood pressure z-score and triglycerides (p < 0.01), but higher HDL-C (p < 0.001), total cholesterol (p < 0.05), and apo-A1 (p < 0.05) compared to those with MUO. Compared to controls, both children with MHO and MUO showed higher fasting insulin (p < 0.05), HOMA-IR (p < 0.05), and QUICKI (p < 0.001). Similarly, both groups had higher hsCRP, fibrinogen, uric acid, and leptin compared to controls (for all, p < 0.001), while their adiponectin was lower (p < 0.05). Visfatin was higher in children with MUO compared to controls (p < 0.01), and it showed a trend to be lower in children with MHO compared to those with MUO (p = 0.1).
Conclusion
This study provides evidence that children identified as having MHO by the consensus-based criteria had better metabolic profiles than youth with MUO, but worse than NW. Further research is needed in pediatric populations both regarding MHO criteria and the nature of the MHO phenotype per se.
Similar content being viewed by others
References
J. Bentham, M. Di Cesare, V. Bilano, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 390: 2627–2642 (2017)
R. Lakshman, C.E. Elks, K.K. Ong, Childhood obesity. Circulation 126, 1770–1779 (2012)
S.J. Olshansky, D.J. Passaro, R.C. Hershow et al. A potential decline in life expectancy in the united states in the 21st century. N. Engl. J. Med. 352, 1138–1145 (2005)
A. Tsatsoulis, S.A. Paschou, Metabolically healthy obesity: criteria, epidemiology, controversies, and consequences. Curr. Obes. Rep. 9, 109–120 (2020)
H. Lin, L. Zhang, R. Zheng et al. The prevalence, metabolic risk and effects of lifestyle intervention for metabolically healthy obesity: a systematic review and meta-analysis. Medicine 96, e8838 (2017)
R.L. Prince, J.L. Kuk, K.A. Ambler et al. Predictors of metabolically healthy obesity in children. Diabetes Care 37, 1462–1468 (2014)
D.Y. Yoon, Y.A. Lee, J. Lee et al. Prevalence and clinical characteristics of metabolically healthy obesity in Korean children and adolescents: data from the Korea National Health and Nutrition Examination Survey. J. Korean Med. Sci. 32, 1840–1847 (2017)
R. Vukovic, T.J. Dos Santos, M. Ybarra et al. Children with metabolically healthy obesity: a review. Front. Endocrinol. 10, 865 (2019)
R. Weiss, S.E. Taksali, S. Dufour et al. The “Obese insulin-sensitive” adolescent: Importance of adiponectin and lipid partitioning. J. Clin. Endocrinol. Metab. 90, 3731–3737 (2005)
R. Vukovic, T. Milenkovic, K. Mitrovic et al. Preserved insulin sensitivity predicts metabolically healthy obese phenotype in children and adolescents. Eur. J. Pediatr. 174, 1649–1655 (2015)
D. Weghuber, S. Zelzer, I. Stelzer et al. High risk vs “metabolically healthy” phenotype in juvenile obesity—neck subcutaneous adipose tissue and serum uric acid are clinically relevant. Exp. Clin. Endocrinol. Diabetes 121, 384–390 (2013)
L. Bervoets, G. Massa, Classification and clinical characterization of metabolically “healthy” obese children and adolescents. J. Pediatr. Endocrinol. Metab. 29, 553–560 (2016)
C. Cadenas-Sanchez, J.R. Ruiz, I. Labayen et al. Prevalence of metabolically healthy but overweight/obese phenotype and its association with sedentary time, physical activity, and fitness. J. Adolesc. Heal. 61, 107–114 (2017)
M.L. Evia-Viscarra, R. Guardado-Mendoza. Comparison between metabolically healthy obesity and metabolically unhealthy obesity by different definitions among Mexican children. J. Pediatr. Endocrinol. Metab. 33, 215–222 (2020)
S. Damanhoury, A.S. Newton, M. Rashid et al. Defining metabolically healthy obesity in children: a scoping review. Obes. Rev. 19, 1476–1491 (2018)
F. Magkos, Metabolically healthy obesity: what’s in a name? Am. J. Clin. Nutr. 110, 533–537 (2019)
R. Caleyachetty, G.N. Thomas, K.A. Toulis et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J. Am. Coll. Cardiol. 70, 1429–1437 (2017)
M. Blüher, Obesity: the myth of innocent obesity. Nat. Rev. Endocrinol. 13, 691–692 (2017)
K.D. Tambalis, D.B. Panagiotakos, G. Arnaoutis et al. Establishing cross-sectional curves for height, weight, body mass index and waist circumference for 4- to 18-year-old Greek children, using the Lambda Mu and Sigma (LMS) statistical method. Hippokratia 19, 239–248 (2015)
B. Falkner, S.R. Daniels. Summary of the fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Hypertension 44, 387–388 (2004)
W.A. Marshall, J.M. Tanner, Variations in the pattern of pubertal changes in boys. Arch. Dis. Child 45, 13–23 (1970)
W.A. Marshall, J.M. Tanner, Variations in pattern of pubertal changes in girls. Arch. Dis. Child 44, 291–303 (1969)
D.R. Matthews, J.P. Hosker, A.S. Rudenski et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985)
A. Katz, S.S. Nambi, K. Mather et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J. Clin. Endocrinol. Metab. 85, 2402–2410 (2000)
W.T. Friedewald, R.I. Levy, D.S. Fredrickson. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502 (1972)
U. Lausten-Thomsen, M. Christiansen, C.E. Fonvig et al. Reference values for serum total adiponectin in healthy non-obese children and adolescents. Clin. Chim. Acta 450, 11–14 (2015)
M.B. Horlick, M. Rosenbaum, M. Nicolson et al. Effect of puberty on the relationship between circulating leptin and body composition. J. Clin. Endocrinol. Metab. 85, 2509–2518 (2000)
D. Taşkesen, B. Kirel, T. Us. Serum visfatin levels, adiposity and glucose metabolism in obese adolescents. J. Clin. Res. Pediatr. Endocrinol. 4, 76–81 (2012)
U. Sack, U. Burkhardt, M. Borte et al. Age-dependent levels of select immunological mediators in sera of healthy children. Clin. Diagn. Lab. Immunol. 5, 28–32 (1998)
D. Altman, Sample size, in Practical Statistics for Medical Research (Chapman & Hall, London, 1994), pp. 456–60
G. O’Malley, N. Santoro, V. Northrup et al. High normal fasting glucose level in obese youth: a marker for insulin resistance and beta cell dysregulation. Diabetologia 53, 1199–1209 (2010)
E. Hagman, T. Reinehr, J. Kowalski et al. Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int. J. Obes. 38, 40–45 (2014)
K.A. Christou, G.A. Christou, A. Karamoutsios et al. Metabolically healthy obesity is characterized by a proinflammatory phenotype of circulating monocyte subsets. Metab. Syndr. Relat. Disord. 17, 259–265 (2019)
S. Genovesi, L. Antolini, A. Orlando, et al. Cardiovascular risk factors associated with the metabolically healthy obese (MHO) phenotype compared to the metabolically unhealthy obese (MUO) phenotype in children. Front. Endocrinol. (Lausanne) 11, 27–35 (2020)
J. Fu, Y. Li, I.C. Esangbedo et al. Circulating osteonectin and adipokine profiles in relation to metabolically healthy obesity in Chinese children: Findings from BCAMS. J. Am. Heart Assoc. 7, e009169 (2018)
W. Ding, H. Cheng, F. Chen et al. Adipokines are associated with hypertension in metabolically healthy obese (MHO) children and adolescents: a prospective population-based cohort study. J. Epidemiol. 28, 19–26 (2018)
G. Labruna, F. Pasanisi, C. Nardelli, et al. High leptin/adiponectin ratio and serum triglycerides are associated with an at-risk phenotype in young severely obese patients. Obesity (Silver Spring) 19, 1492–1496 (2011)
I. Aldhoon-Hainerová, H. Zamrazilová, M. Hill et al. Insulin sensitivity and its relation to hormones in adolescent boys and girls. Metabolism 67, 90–98 (2017)
M.B. Vos, S.H. Abrams, S.E. Barlow et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the expert committee on NAFLD (ECON) and the North American society of pediatric gastroenterology, hepatology and nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 64, 319–334 (2017)
Y. Kim, Y. Chang, Y.K. Cho, et al. Metabolically healthy versus unhealthy obesity and risk of fibrosis progression in non-alcoholic fatty liver disease. Liver Int. 39, 1884–1894 (2019)
P.K.C. Selvakumar, M.N. Kabbany, R. Lopez et al. Prevalence and risk factors of nonalcoholic fatty liver disease in metabolically healthy obese adolescents in the United States: an analysis of national health and nutrition examination survey data. J. Hepatol. 66, S587–S588 (2017)
A. Lonardo, A. Mantovani, S. Lugari et al. Epidemiology and pathophysiology of the association between NAFLD and metabolically healthy or metabolically unhealthy obesity. Ann. Hepatol. 19, 359–366 (2020)
M. Blüher, Metabolically healthy obesity. Endocr. Rev. 41, 405–420 (2020)
G. Farello, A. Antenucci, S. Stagi et al. Metabolically healthy and metabolically unhealthy obese children both have increased carotid intima-media thickness: a case control study. BMC Cardiovasc. Disord. 18, 140–146 (2018)
M. Zhao, A. López-Bermejo, C.A. Caserta et al. Metabolically healthy obesity and high carotid intima-media thickness in children and adolescents: international childhood vascular structure evaluation Consortium. Diabetes Care 42, 119–125 (2019)
Author information
Authors and Affiliations
Contributions
VG and AS contributed to the study conception and design. Material preparation and data collection were performed by AS and ES. Data analysis was performed by VG and SP. The first draft of the manuscript was written by AS and VG. ES and SP made substantial contributions to the final version of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval (include appropriate approvals or waivers)
Approved by the Institutional Scientific Review Board at Ioannina University Hospital.
Consent to participate (include appropriate statements)
Written informed consent and each child’s assent were obtained from all participants and their parents of all groups for participating in the study.
Consent for publication (include appropriate statements)
Written informed consent and each child’s assent were obtained from all participants and their parents of all groups for publishing the study’s results.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Serbis, A., Giapros, V., Paschou, S.A. et al. Children with metabolically healthy obesity have a worse metabolic profile compared to normal-weight peers: a cross-sectional study. Endocrine 73, 580–587 (2021). https://doi.org/10.1007/s12020-021-02762-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02762-6