Abstract
Purpose
In DTC patients, 131-radioiodine therapy has routinely been used for many years for thyroid remnant ablation after thyroid surgery. To date, two different strategies can be used to achieve sufficient TSH stimulation on thyroid remnant: (I) Levo-thyroxine withdrawal or (II) rhTSH stimulation. The aim of our study was to compare the abdominal absorbed dose ratio between differentiated thyroid cancer patients who underwent thyroid remnant ablation after either L-T4 withdrawal or rhTSH stimulation.
Methods
We reviewed the records of 63 patients affected by differentiated thyroid cancer. All patients underwent thyroid remnant ablation after either L-T4 withdrawal or rhTSH stimulation.
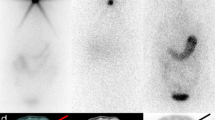
A post-therapy whole-body scan was obtained 5 days after 131-radioiodine therapy. Qualitative and quantitative image analysis was performed. Quantitative analysis was performed by drawing seven regions of interest on the abdomen (anterior and posterior views) to estimate both the activity ratio (AR) and absorbed dose ratio (DR) obtained in patients treated in hypothyroidism or after rhTSH stimulation.
Results
The values of the activity and absorbed dose ratios obtained on each abdomen region (liver, stomach, ascending colon, transverse colon, descending colon, rectum, and small intestine) were always higher in patients treated after L-T4 withdrawal than after rhTSH stimulation with p-values of 0.000, 0.000, 0.001, 0.000, 0.022, 0.007, and 0.002, respectively.
Conclusions
DTC patients treated with 131-radioiodine after rhTSH stimulation have lower abdominal radioiodine activity than hypothyroid patients. Our data could be of practical relevance in terms of patient management. The potential impact on rare radioiodine-related gastrointestinal side effects is to be established in specifically designed prospective studies.

Similar content being viewed by others
References
F. Pacini, F. Basolo, R. Bellantone, G. Boni, M.A. Cannizzaro, M. De Palma, C. Durante, R. Elisei, G. Fadda, A. Frasoldati, L. Fugazzola, R. Guglielmi, C.P. Lombardi, P. Miccoli, E. Papini, G. Pellegriti, L. Pezzullo, A. Pontecorvi, M. Salvatori, E. Seregni, P. Vitti, Italian consensus on diagnosis and treatment of differentiated thyroid cancer: joint statements of six Italian societies. J. Endocrinol. Invest. 41(7), 849–876 (2018)
A. Campennì, L. Giovanella, A. Alibrandi, M. Siracusa, R.M. Ruggeri, S. Baldari, BRAF (V600E) mutation in isthmic malignant thyroid nodules. Clin. Endocrinol. 84(1), 152–153 (2016)
A. Campennì, L. Giovanella, M. Siracusa, M.E. Stipo, A. Alibrandi, M. Cucinotta, R.M. Ruggeri, S. Baldari, Is malignant nodule topography an additional risk factor for metastatic disease in low-risk differentiated thyroid cancer? Thyroid 24(11), 1607–1611 (2014)
R. Gallicchio, S. Giacomobono, D. Capacchione, A. Nardelli, F. Barbato, A. Nappi, T. Pellegrino, G. Storto, Should patients with remnants from thyroid microcarcinoma really not be treated with iodine-131 ablation? Endocrine 44(2), 426–433 (2013)
R.M. Tuttle, H. Tala, J. Shah, R. Leboeuf, R. Ghossein, M. Gonen, M. Brokhin, G. Omry, J.A. Fagin, A. Shaha, Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system. Thyroid 20(12), 1341–1349 (2010)
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer – The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26, 1–133 (2015)
F.A. Verburg, C. Aktolun, A. Chiti, S. Frangos, L. Giovanella, M. Hoffmann, I. Iakovou, J. Mihailovic, B.J. Krause, W. Langsteger, M. Luster; EANM and the EANM Thyroid Committee, Why the European Association of Nuclear Medicine has declined to endorse the 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Eur. J. Nucl. Med. Mol. Imaging 43, 1001–1005 (2016)
A.M. Sawka, L. Thabane, L. Parlea, I. Ibrahim-Zada, R.W. Tsang, J.D. Brierley, S. Straus, S. Ezzat, D.P. Goldstein, Second primary malignancy risk after radioactive iodine treatment for thyroid cancer: a systematic review and meta-analysis. Thyroid 19, 451–457 (2009)
S. Subramanian, D.P. Goldstein, L. Parlea, L. Thabane, S. Ezzat, I. Ibrahim-Zada, S. Straus, J.D. Brierley, R.W. Tsang, A. Gafni, L. Rotstein, A.M. Sawka, Second primary malignancy risk in thyroid cancer survivors: a systematic review and meta-analysis. Thyroid 17(12), 1277–1288 (2007)
M. Silva-Vieira, S. Carrilho Vaz, S. Esteves, T.C. Ferreira, E. Limbert, L. Salgado, V. Leite, Second primary cancer in patients with differentiated thyroid cancer: does radioiodine play a role? Thyroid 27(8), 1068–1076 (2017)
F. de Vathaire, M. Schlumberger, M.J. Delisle, C. Francese, C. Challeton, E. de la Genardiére, F. Meunier, C. Parmentier, C. Hill, H. Sancho-Garnier, Leukaemias and cancers following iodine-131 administration for thyroid cancer. Br. J. Cancer 75(5), 734–739 (1997)
A. Campennì, L. Giovanella, S.A. Pignata, M.A. Violi, M. Siracusa, A. Alibrandi, M. Moleti, E. Amato, R.M. Ruggeri, F. Vermiglio, S. Baldari, Thyroid remnant ablation in differentiated thyroid cancer: searching for the most effective radioiodine activity and stimulation strategy in a real-life scenario. Nucl. Med. Commun. 36, 1100–1106 (2015)
C. Reiners, M. Lassmann, M. Luster, Recombinant human thyrotropin: safety and quality of life evaluation. J. Endocrinol. Invest. 35(6 Suppl), 30–35 (2012)
F. Pacini, P.W. Ladenson, M. Schlumberger, A. Driedger, M. Luster, R.T. Kloos, S. Sherman, B. Haugen, C. Corone, E. Molinaro, R. Elisei, C. Ceccarelli, A. Pinchera, R.L. Wahl, S. Leboulleux, M. Ricard, J. Yoo, N.L. Busaidy, E. Delpassand, H. Hanscheid, R. Felbinger, M. Lassmann, C. Reiners, Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J. Clin. Endocrinol. Metab. 91(3), 926–932 (2006)
J.A. Siegel, S.R. Thomas, J.B. Stubbs, M.G. Stabin, M.T. Hays, K.F. Koral, J.S. Robertson, R.W. Howell, B.W. Wessels, D.R. Fisher, D.A. Weber, A.B. Brill, MIRD pamphlet no. 16: techniques for quantitative radiopharmaceutical biodistribution data acquisition and analysis for use in human radiation dose estimates. J. Nucl. Med. 40(2), 37S–61S (1999)
H. Remy, I. Borget, S. Leboulleux, N. Guilabert, F. Lavielle, J. Garsi, C. Bournaud, S. Gupta, M. Schlumberger, M. Ricard, 131I effective half-life and dosimetry in thyroid cancer patients. J. Nucl. Med. 49, 1445–1450 (2008)
M. Luster, C. Aktolun, I. Amendoeira, M. Barczyński, K.C. Bible, L.H. Duntas, R. Elisei, D. Handkiewicz-Junak, M. Hoffmann, B. Jarzab, L. Leenhardt, T.J. Musholt, K. Newbold, I.J. Nixon, J. Smit, M. Sobrinho-Simões, J.A. Sosa, R.M. Tuttle, F. Verburg, L. Wartofsky, D. Führer-Sakel, European perspective on the 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Proceedings of an Interactive International Symposium. Thyroid. (2018). https://doi.org/10.1089/thy.2017.0129.
E.L. Mazzaferri, S.M. Jhiang, Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am. J. Med. 97, 418–428 (1994)
A.M. Sawka, K. Thephamongkhol, M. Brouwers, L. Thabane, G. Browman, H.C. Gerstein, Clinical review 170: a systematic review and metaanalysis of the effectiveness of radioactive iodine remnant ablation for well-differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 89(8), 3668–3676 (2004)
E. Ruel, S. Thomas, M. Dinan, J.M. Perkins, S.A. Roman, J.A. Sosa, Adjuvant radioactive iodine therapy is associated with improved survival for patients with intermediate-risk papillary thyroid cancer. J. Clin. Endocrinol. Metab. 100(4), 1529–1536 (2015)
A. Campennì, S.A. Pignata, S. Baldari, Post-operative radioiodine therapy (RaIT) as adjuvant therapy in low–intermediate risk differentiated thyroid cancer. Clin. Transl. Imaging. (2018). https://doi.org/10.1007/s40336-018-0298-3
Y. Luo, Y. Zhao, K. Chen, J. Shen, J. Shi, S. Lu, J. Lei, Z. Li, D. Luo, Clinical analysis of cervical lymph node metastasis risk factors in patients with papillary thyroid microcarcinoma. J. Endocrinol. Invest. (2018). https://doi.org/10.1007/s40618-018-0908-y
A. Campennì, L. Giovanella, S.A. Pignata, A. Vento, A. Alibrandi, L. Sturiale, R. Laudicella, A.D. Comis, R. Filice, G. Giuffrida, M.E. Stipo, S. Giovinazzo, F. Trimarchi, R.M. Ruggeri, S. Baldari, Undetectable or low ( < 1 ng/ml) postsurgical thyroglobulin values do not rule out metastases in early stage differentiated thyroid cancer patients. Oncotarget 9, 17491–17500 (2018)
H. Hänscheid, M. Lassmann, M. Luster, S.R. Thomas, F. Pacini, C. Ceccarelli, P.W. Ladenson, R.L. Wahl, M. Schlumberger, M. Ricard, A. Driedger, R.T. Kloos, S.I. Sherman, B.R. Haugen, V. Carriere, C. Corone, C. Reiners, Iodine biokinetics and dosimetry in radioiodine therapy of thyroid cancer: procedures and results of a prospective international controlled study of ablation after rhTSH or hormone withdrawal. J. Nucl. Med. 47, 648–654 (2006)
M. Lassmann, H. Hänscheid, F.A. Verburg, M. Luster, The use of dosimetry in the treatment of differentiated thyroid cancer. Q. J. Nucl. Med. Mol. Imaging 55(2), 107–115 (2011)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Campennì, A., Amato, E., Laudicella, R. et al. Recombinant human thyrotropin (rhTSH) versus Levo-thyroxine withdrawal in radioiodine therapy of differentiated thyroid cancer patients: differences in abdominal absorbed dose. Endocrine 65, 132–137 (2019). https://doi.org/10.1007/s12020-019-01897-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01897-x