Abstract
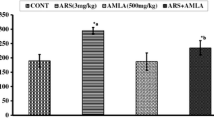
Herein, we investigated whether L-ascorbic acid (L-AA) and α-tocopherol (α-T) co-administration has the potential to alleviate arsenic-induced immunotoxicities in the thymus, spleen, and circulating leukocytes. Forty-eight adult male Wistar rats were randomly divided into four groups before the treatment: group I (control); group II (sodium arsenite, 3 mg/kg/day/rat); group III (sodium arsenite + L-AA (200 mg/kg/day/rat) and α-T (400 mg/kg/day/rat)); group IV (L-AA and α-T). The result showed that sodium arsenite exposure (consecutive 30 days) caused weight reduction, structural alterations in the thymus and spleen, accompanied by a decrease in thymocyte and splenocyte count. Decreased superoxide dismutase and catalase activity, increased malondialdehyde and protein–carbonyl content, reduced Nrf2 and Bcl2 expression, and increased p-ERK, NF-kβ, Bax, and cleaved-caspase-3 expression were also observed in the thymus and spleen of arsenic-exposed rats. Enhanced plasma ACTH and corticosterone, ROS-induced apoptosis of lymphocytes were also observed. L-AA and α-T co-administration has the potential to abrogate the deleterious impact of arsenic on the thymus, spleen, and circulating lymphocytes. Whole transcriptome analysis of leukocytes revealed that arsenic treatment augmented the expression of Itga4, Itgam, and MMP9 genes, which might help in transient migration of the leukocytes through the endothelial cell layer. Co-administration with L-AA and α-T maintained Itga4, Itgam, and MMP9 gene expression within leukocytes at a lower level.
Graphical Abstract














Similar content being viewed by others
Data Availability
The data that supports the finding of the study are available from the corresponding author upon reasonable request.
References
Duan X, Gao S, Li J et al (2017) Acute arsenic exposure induces inflammatory responses and CD4+ T cell subpopulations differentiation in spleen and thymus with the involvement of MAPK, NF-kB, and Nrf2. Mol Immunol 81:160–172. https://doi.org/10.1016/j.molimm.2016.12.005
Nicomel N, Leus K, Folens K et al (2015) Technologies for arsenic removal from water: current status and future perspectives. Int J Environ Res Public Health 13:62. https://doi.org/10.3390/ijerph13010062
Islam K, Wang QQ, Naranmandura H (2015) Molecular mechanisms of arsenic toxicity. Advances in Molecular Toxicology 9: 77–107. https://doi.org/10.1016/B978-0-12-802229-0.00002-5
Buchet JP, Lauwerys R, Roels H (1981) Comparison of the urinary excretion of arsenic metabolites after a single oral dose of sodium arsenite, monomethylarsonate, or dimethylarsinate in man. Int Arch Occup Environ Health 48:71–79. https://doi.org/10.1007/BF00405933
Lin K, Lu S, Wang J, Yang Y (2015) The arsenic contamination of rice in Guangdong Province, the most economically dynamic provinces of China: arsenic speciation and its potential health risk. Environ Geochem Health 37:353–361. https://doi.org/10.1007/s10653-014-9652-1
Babar MM, Tariq A (2018) Status of arsenic toxicity in the world. In: Mechanisms of arsenic toxicity and tolerance in plants. Springer, Singapore. 11:457–481. https://doi.org/10.1007/978-981-13-1292-2_18
Hamad SH, Schauer JJ, Shafer MM et al (2014) Risk assessment of total and bioavailable potentially toxic elements (PTEs) in urban soils of Baghdad-Iraq. Sci Total Environ 494–495:39–48. https://doi.org/10.1016/j.scitotenv.2014.06.006
Weindorf DC, Paulette L, Man T (2013) In-situ assessment of metal contamination via portable X-ray fluorescence spectroscopy: Zlatna, Romania. Environ Pollut 182:92–100. https://doi.org/10.1016/j.envpol.2013.07.008
Varsányi I, Kovács LÓ (2006) Arsenic, iron and organic matter in sediments and groundwater in the Pannonian Basin, Hungary. Appl Geochemistry 21:949–963. https://doi.org/10.1016/j.apgeochem.2006.03.006
Acharyya SK, Lahiri S, Raymahashay BC, Bhowmik A (2000) Arsenic toxicity of groundwater in parts of the Bengal basin in India and Bangladesh: the role of Quaternary stratigraphy and Holocene sea-level fluctuation. Environ Geol 39:1127–1137. https://doi.org/10.1007/s002540000107
Shaji E, Santosh M, Sarath KV et al (2021) Arsenic contamination of groundwater: a global synopsis with focus on the Indian Peninsula. Geosci Front 12:101079. https://doi.org/10.1016/j.gsf.2020.08.015
Niedzwiecki MM, Liu X, Zhu H et al (2018) Serum homocysteine, arsenic methylation, and arsenic-induced skin lesion incidence in Bangladesh: a one-carbon metabolism candidate gene study. Environ Int 113:133–142. https://doi.org/10.1016/j.envint.2018.01.015
Kuo C-C, Moon KA, Wang S-L et al (2017) The association of arsenic metabolism with cancer, cardiovascular disease, and diabetes: a systematic review of the epidemiological evidence. Environ Health Perspect 125:087001. https://doi.org/10.1289/EHP577
Mohammed Abdul KS, Jayasinghe SS, Chandana EPS et al (2015) Arsenic and human health effects: a review. Environ Toxicol Pharmacol 40:828–846. https://doi.org/10.1016/j.etap.2015.09.016
Leonardi G, Vahter M, Clemens F et al (2012) Inorganic arsenic and basal cell carcinoma in areas of Hungary, Romania, and Slovakia: a case–control study. Environ Health Perspect 120:721–726. https://doi.org/10.1289/ehp.1103534
Kumar A, Ali M, Kumar R et al (2021) Arsenic exposure in Indo Gangetic plains of Bihar causing increased cancer risk. Sci Rep 11:2376. https://doi.org/10.1038/s41598-021-81579-9
Gera R, Singh V, Mitra S et al (2017) Arsenic exposure impels CD4 commitment in thymus and suppress T cell cytokine secretion by increasing regulatory T cells. Sci Rep 7:7140. https://doi.org/10.1038/s41598-017-07271-z
Rahman HH, Niemann D, Singh D (2020) Arsenic exposure and association with hepatitis E IgG antibodies. Occup Dis Environ Med 08:111–122. https://doi.org/10.4236/odem.2020.83009
Raqib R, Ahmed S, Sultana R et al (2009) Effects of in utero arsenic exposure on child immunity and morbidity in rural Bangladesh. Toxicol Lett 185:197–202. https://doi.org/10.1016/j.toxlet.2009.01.001
Andrew AS, Jewell DA, Mason RA et al (2008) Drinking-water arsenic exposure modulates gene expression in human lymphocytes from a U.S. population. Environ Health Perspect 116:524–531. https://doi.org/10.1289/ehp.10861
Moore S, Prentice A, Wagatsuma Y et al (2009) Early-life nutritional and environmental determinants of thymic size in infants born in rural Bangladesh. Acta Paediatr 98:1168–1175. https://doi.org/10.1111/j.1651-2227.2009.01292.x
Xu H, McClain S, Medina S et al (2016) Differential sensitivities of bone marrow, spleen and thymus to genotoxicity induced by environmentally relevant concentrations of arsenite. Toxicol Lett 262:55–61. https://doi.org/10.1016/j.toxlet.2016.09.008
Jamal Z, Das J, Ghosh S et al (2020) Arsenic-induced immunomodulatory effects disorient the survival-death interface by stabilizing the Hsp90/Beclin1 interaction. Chemosphere 238:124647. https://doi.org/10.1016/j.chemosphere.2019.124647
Chen F, Luo Y, Li C et al (2021) Sub-chronic low-dose arsenic in rice exposure induces gut microbiome perturbations in mice. Ecotoxicol Environ Saf 227:112934. https://doi.org/10.1016/j.ecoenv.2021.112934
Soto-Peña GA, Luna AL, Acosta-Saavedra L et al (2006) Assessment of lymphocyte subpopulations and cytokine secretion in children exposed to arsenic. FASEB J 20:779–781. https://doi.org/10.1096/fj.05-4860fje
Biswas R, Ghosh P, Banerjee N et al (2008) Analysis of T-cell proliferation and cytokine secretion in the individuals exposed to arsenic. Hum Exp Toxicol 27:381–386. https://doi.org/10.1177/0960327108094607
Yan N, Xu G, Zhang C et al (2020) Chronic arsenic exposure induces the time-dependent modulation of inflammation and immunosuppression in spleen. Cell Biosci 10:91. https://doi.org/10.1186/s13578-020-00448-6
Delgado J, Dufour L, Grimaldo J et al (2000) Effects of arsenite on central monoamines and plasmatic levels of adrenocorticotropic hormone (ACTH) in mice. Toxicol Lett 117:61–67. https://doi.org/10.1016/S0378-4274(00)00240-X
Goggin SL, Labrecque MT, Allan AM (2012) Perinatal exposure to 50 ppb sodium arsenate induces hypothalamic-pituitary-adrenal axis dysregulation in male C57BL/6 mice. Neurotoxicology 33:1338–1345. https://doi.org/10.1016/j.neuro.2012.08.010
Barone KS, O’Brien PCM, Stevenson JR (1993) Characterization and mechanisms of thymic atrophy in protein-malnourished mice: role of corticosterone. Cell Immunol 148:226–233. https://doi.org/10.1006/cimm.1993.1105
Matsuoka K, Tsuji D, Taki T, Itoh K (2011) Thymic involution and corticosterone level in Sandhoff disease model mice: new aspects the pathogenesis of GM2 gangliosidosis. J Inherit Metab Dis 34:1061–1068. https://doi.org/10.1007/s10545-011-9316-6
Hernandez ME, Martinez-Mota L, Salinas C et al (2013) Chronic stress induces structural alterations in splenic lymphoid tissue that are associated with changes in corticosterone levels in Wistar-Kyoto rats. Biomed Res Int 2013:1–6. https://doi.org/10.1155/2013/868742
Biswas P, Mukhopadhyay A, Kabir SN, Mukhopadhyay PK (2019) High-protein diet ameliorates arsenic-induced oxidative stress and antagonizes uterine apoptosis in rats. Biol Trace Elem Res 192:222–233. https://doi.org/10.1007/s12011-019-1657-2
Flora SJS, Mittal M, Mehta A (2008) Heavy metal induced oxidative stress & its possible reversal by chelation therapy. Indian J Med Res 128:501–523
Pal P, De A, Roychowdhury T, Mukhopadhyay PK (2022) Vitamin C and E supplementation can ameliorate NaF mediated testicular and spermatozoal DNA damages in adult Wistar rats. Biomarkers 27:361–374. https://doi.org/10.1080/1354750X.2022.2048891
Hamdan DI, Tawfeek N, El-Shiekh RA et al (2022) Salix subserrata bark extract-loaded chitosan nanoparticles attenuate neurotoxicity induced by sodium arsenate in rats in relation with HPLC–PDA-ESI–MS/MS profile. AAPS PharmSciTech 24:15. https://doi.org/10.1208/s12249-022-02478-4
Sankar P, Gopal Telang A, Kalaivanan R et al (2015) Effects of nanoparticle-encapsulated curcumin on arsenic-induced liver toxicity in rats. Environ Toxicol 30:628–637. https://doi.org/10.1002/tox.21940
Organisation for Economic Co-operation and Development (2008) Test No. 407: repeated dose 28-day oral toxicity study in rodents. OECD Guidelines for the Testing of Chemicals, Section 4, OECD Publishing, Paris. https://doi.org/10.1787/9789264070684
Chandravanshi LP, Patel DK (2017) Subchronic early life arsenic exposure at low doses impaired the biogenic amine neurotransmitter and nitric oxide levels in different brain regions of rats. J Environ Anal Toxicol 07: https://doi.org/10.4172/2161-0525.1000477
Baran-Gale J, Morgan MD, Maio S et al (2020) Ageing compromises mouse thymus function and remodels epithelial cell differentiation. Elife 9:. https://doi.org/10.7554/eLife.56221
Ghosh C, Bishayi B (2015) Characterization of Toll-like receptor-4 (TLR-4) in the spleen and thymus of Swiss albino mice and its modulation in experimental endotoxemia. J Immunol Res 2015:1–13. https://doi.org/10.1155/2015/137981
Martin JP, Dailey M, Sugarman E (1987) Negative and positive assays of superoxide dismutase based on hematoxylin autoxidation. Arch Biochem Biophys 255:329–336. https://doi.org/10.1016/0003-9861(87)90400-0
Claiborne, A. (1985). Catalase activity. In: Greenwald, R.A. (ed.) Handbook of methods of oxygen radical research. CRC Press, Boca Raton, Florida, p 283–284
Levine RL, Williams JA, Stadtman EP, Shacter E (1994) Carbonyl assays for determination of oxidatively modified proteins. 233:346–357. https://doi.org/10.1016/S0076-6879(94)33040-9
Brown-Borg H, Johnson WT, Rakoczy S, Romanick M (2001) Mitochondrial oxidant generation and oxidative damage in Ames dwarf and GH transgenic mice. Age (Omaha) 24:85–96. https://doi.org/10.1007/s11357-001-0012-6
Khanam R, Sengupta A, Mukhopadhyay D, Chakraborty S (2022) Identification of Adamts4 as a novel adult cardiac injury biomarker with therapeutic implications in patients with cardiac injuries. Sci Rep 12:9898. https://doi.org/10.1038/s41598-022-13918-3
Killick KE, Browne JA, DE Park S et al (2011) Genome-wide transcriptional profiling of peripheral blood leukocytes from cattle infected with Mycobacterium bovis reveals suppression of host immune genes. BMC Genomics 12:611. https://doi.org/10.1186/1471-2164-12-611
Gong T, Wang C-F, Yuan J-R et al (2015) Inhibition of tumor growth and immunomodulatory effects of flavonoids and scutebarbatines of Scutellaria barbata D. Don in Lewis-bearing C57BL/6 mice. Evid Based Complement Alternat Med 2015:630760. https://doi.org/10.1155/2015/630760
Kile ML, Houseman EA, Baccarelli AA et al (2014) Effect of prenatal arsenic exposure on DNA methylation and leukocyte subpopulations in cord blood. Epigenetics 9:774–782. https://doi.org/10.4161/epi.28153
Burns LA, Munson AE (1993) Gallium arsenide selectively inhibits T cell proliferation and alters expression of CD25 (IL-2R/p55). J Pharmacol Exp Ther 265:178–186
Burchiel SW, Lauer FT, Factor-Litvak P et al (2020) Arsenic exposure associated T cell proliferation, smoking, and vitamin D in Bangladeshi men and women. PLoS One 15:e0234965. https://doi.org/10.1371/journal.pone.0234965
Akter R, Neelotpol S, Kabir MT (2022) Effect of Allium sativum methanol extract in amelioration of arsenic-induced toxicity in Swiss albino mice. Phytomedicine Plus 2:100192. https://doi.org/10.1016/j.phyplu.2021.100192
Ozerkan D, Ozsoy N, Cebesoy S (2014) Response of thymus lymphocytes to streptozotocin-induced diabetes and exogenous vitamin C administration in rats. Microscopy 63:409–417. https://doi.org/10.1093/jmicro/dfu029
Kim H, Bae S, Yu Y et al (2012) The analysis of vitamin C concentration in organs of gulo -/- mice upon vitamin C withdrawal. Immune Netw 12:18. https://doi.org/10.4110/in.2012.12.1.18
Moriguchi S (1998) The role of vitamin E in T-cell differentiation and the decrease of cellular immunity with aging. BioFactors 7:77–86. https://doi.org/10.1002/biof.5520070111
Herman JP, Cullinan WE, Young EA et al (1992) Selective forebrain fiber tract lesions implicate ventral hippocampal structures in tonic regulation of paraventricular nucleus corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) mRNA expression. Brain Res 592:228–238. https://doi.org/10.1016/0006-8993(92)91680-D
Löwenberg M, Verhaar AP, Bilderbeek J et al (2006) Glucocorticoids cause rapid dissociation of a T-cell-receptor-associated protein complex containing LCK and FYN. EMBO Rep 7:1023–1029. https://doi.org/10.1038/sj.embor.7400775
Löwenberg M, Tuynman J, Bilderbeek J et al (2005) Rapid immunosuppressive effects of glucocorticoids mediated through Lck and Fyn. Blood 106:1703–1710. https://doi.org/10.1182/blood-2004-12-4790
Baschant U, Tuckermann J (2010) The role of the glucocorticoid receptor in inflammation and immunity. J Steroid Biochem Mol Biol 120:69–75. https://doi.org/10.1016/j.jsbmb.2010.03.058
Zhang N, Zhao W, Hu Z-J et al (2021) Protective effects and mechanisms of high-dose vitamin C on sepsis-associated cognitive impairment in rats. Sci Rep 11:14511. https://doi.org/10.1038/s41598-021-93861-x
Tveden-Nyborg P, Johansen LK, Raida Z et al (2009) Vitamin C deficiency in early postnatal life impairs spatial memory and reduces the number of hippocampal neurons in guinea pigs. Am J Clin Nutr 90:540–546. https://doi.org/10.3945/ajcn.2009.27954
Chang B-J, Jang B-J, Son TG et al (2012) Ascorbic acid ameliorates oxidative damage induced by maternal low-level lead exposure in the hippocampus of rat pups during gestation and lactation. Food Chem Toxicol 50:104–108. https://doi.org/10.1016/j.fct.2011.09.043
Gurer H, Ercal N (2000) Can antioxidants be beneficial in the treatment of lead poisoning? Free Radic Biol Med 29:927–945. https://doi.org/10.1016/S0891-5849(00)00413-5
Tomé AR, Feng D, Freitas RM (2010) The effects of alpha-tocopherol on hippocampal oxidative stress prior to in pilocarpine-induced seizures. Neurochem Res 35:580–587. https://doi.org/10.1007/s11064-009-0102-x
Nesari A, Mansouri MT, Khodayar MJ, Rezaei M (2021) Preadministration of high-dose alpha-tocopherol improved memory impairment and mitochondrial dysfunction induced by proteasome inhibition in rat hippocampus. Nutr Neurosci 24:119–129. https://doi.org/10.1080/1028415X.2019.1601888
Mahmoud KZ, Edens FW, Eisen EJ, Havenstein GB (2004) Ascorbic acid decreases heat shock protein 70 and plasma corticosterone response in broilers (Gallus gallus domesticus) subjected to cyclic heat stress. Comp Biochem Physiol Part B Biochem Mol Biol 137:35–42. https://doi.org/10.1016/j.cbpc.2003.09.013
Ibrahim IAA, Kamisah Y, Nafeeza MI, Azlina MFN (2012) The effects of palm vitamin E on stress hormone levels and gastric lesions in stress-induced rats. Arch Med Sci 1:22–29. https://doi.org/10.5114/aoms.2012.27276
Janasik B, Reszka E, Stanislawska M et al (2018) Effect of arsenic exposure on NRF2-KEAP1 pathway and epigenetic modification. Biol Trace Elem Res 185:11–19. https://doi.org/10.1007/s12011-017-1219-4
Jin W, Xue Y, Xue Y et al (2020) Tannic acid ameliorates arsenic trioxide-induced nephrotoxicity, contribution of NF-κB and Nrf2 pathways. Biomed Pharmacother 126:110047. https://doi.org/10.1016/j.biopha.2020.110047
Khadrawy O, Gebremedhn S, Salilew-Wondim D et al (2019) Endogenous and exogenous modulation of Nrf2 mediated oxidative stress response in bovine granulosa cells: potential implication for ovarian function. Int J Mol Sci 20:1635. https://doi.org/10.3390/ijms20071635
Khan MM, Kim YK, Bilkis T et al (2020) Reduction of oxidative stress through activating the Nrf2 mediated HO-1 antioxidant efficacy signaling pathway by MS15, an antimicrobial peptide from Bacillus velezensis. Antioxidants 9:934. https://doi.org/10.3390/antiox9100934
Xu L-L, Zhao B, Sun S-L et al (2020) High-dose vitamin C alleviates pancreatic injury via the NRF2/NQO1/HO-1 pathway in a rat model of severe acute pancreatitis. Ann Transl Med 8:852–852. https://doi.org/10.21037/atm-19-4552
Feng Z, Liu Z, Li X et al (2010) α-Tocopherol is an effective phase II enzyme inducer: protective effects on acrolein-induced oxidative stress and mitochondrial dysfunction in human retinal pigment epithelial cells. J Nutr Biochem 21:1222–1231. https://doi.org/10.1016/j.jnutbio.2009.10.010
Vineetha RC, Binu P, Arathi P, Nair RH (2018) L-ascorbic acid and α-tocopherol attenuate arsenic trioxide-induced toxicity in H9c2 cardiomyocytes by the activation of Nrf2 and Bcl2 transcription factors. Toxicol Mech Methods 28:353–360. https://doi.org/10.1080/15376516.2017.1422578
Rui W, Guan L, Zhang F et al (2016) PM 2.5 -induced oxidative stress increases adhesion molecules expression in human endothelial cells through the ERK/AKT/NF-κB-dependent pathway. J Appl Toxicol 36:48–59. https://doi.org/10.1002/jat.3143
Bodaghi-Namileh V, Sepand MR, Omidi A et al (2018) Acetyl- l -carnitine attenuates arsenic-induced liver injury by abrogation of mitochondrial dysfunction, inflammation, and apoptosis in rats. Environ Toxicol Pharmacol 58:11–20. https://doi.org/10.1016/j.etap.2017.12.005
Fry RC, Navasumrit P, Valiathan C et al (2007) Activation of inflammation/NF-κB signaling in infants born to arsenic-exposed mothers. PLoS Genet 3:e207. https://doi.org/10.1371/journal.pgen.0030207
Aguilera O, Muñoz-Sagastibelza M, Torrejón B et al (2016) Vitamin C uncouples the Warburg metabolic switch in KRAS mutant colon cancer. Oncotarget 7:47954–47965. https://doi.org/10.18632/oncotarget.10087
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta - Mol Cell Res 1863:2977–2992. https://doi.org/10.1016/j.bbamcr.2016.09.012
Tzifi F, Economopoulou C, Gourgiotis D et al (2012) The role of BCL2 family of apoptosis regulator proteins in acute and chronic leukemias. Adv Hematol 2012:1–15. https://doi.org/10.1155/2012/524308
Xia Y, Hao G, Yang Y (2009) Study on reproductive and immune toxicity of male rats exposed to As2O3. Wei Sheng Yan Jiu 38:720–722
Rousselot P, Larghero J, Labaume S et al (2004) Arsenic trioxide is effective in the treatment of multiple myeloma in SCID mice. Eur J Haematol 72:166–171. https://doi.org/10.1046/j.0902-4441.2003.00194.x
Burchiel SW, Lauer FT, Beswick EJ et al (2014) Differential susceptibility of human peripheral blood T cells to suppression by environmental levels of sodium arsenite and monomethylarsonous acid. PLoS One 9:e109192. https://doi.org/10.1371/journal.pone.0109192
Grollman AP, Moriya M (1993) Mutagenesis by 8-oxoguanine: an enemy within. Trends Genet 9:246–249. https://doi.org/10.1016/0168-9525(93)90089-Z
Shockley AH, Doo DW, Rodriguez GP, Crouse GF (2013) Oxidative damage and mutagenesis in Saccharomyces cerevisiae : genetic studies of pathways affecting replication fidelity of 8-oxoguanine. Genetics 195:359–367. https://doi.org/10.1534/genetics.113.153874
Ba X, Boldogh I (2018) 8-Oxoguanine DNA glycosylase 1: beyond repair of the oxidatively modified base lesions. Redox Biol 14:669–678. https://doi.org/10.1016/j.redox.2017.11.008
Ebert F, Weiss A, Bültemeyer M et al (2011) Arsenicals affect base excision repair by several mechanisms. Mutat Res Mol Mech Mutagen 715:32–41. https://doi.org/10.1016/j.mrfmmm.2011.07.004
Sykora P, Snow ET (2008) Modulation of DNA polymerase beta-dependent base excision repair in cultured human cells after low dose exposure to arsenite. Toxicol Appl Pharmacol 228:385–394. https://doi.org/10.1016/j.taap.2007.12.019
Idriss HT, Al-Assar O, Wilson SH (2002) DNA polymerase β. Int J Biochem Cell Biol 34:321–324. https://doi.org/10.1016/S1357-2725(01)00131-5
Andrew AS, Karagas MR, Hamilton JW (2003) Decreased DNA repair gene expression among individuals exposed to arsenic in United States drinking water. Int J Cancer 104:263–268. https://doi.org/10.1002/ijc.10968
Kadirvel R, Sundaram K, Mani S et al (2007) Supplementation of ascorbic acid and α-tocopherol prevents arsenic-induced protein oxidation and DNA damage induced by arsenic in rats. Hum Exp Toxicol 26:939–946. https://doi.org/10.1177/0960327107087909
Tarng D-C, Liu T-Y, Huang T-P (2004) Protective effect of vitamin C on 8-hydroxy-2′-deoxyguanosine level in peripheral blood lymphocytes of chronic hemodialysis patients. Kidney Int 66:820–831. https://doi.org/10.1111/j.1523-1755.2004.00809.x
Rossner P, Uhlirova K, Beskid O et al (2011) Expression of XRCC5 in peripheral blood lymphocytes is upregulated in subjects from a heavily polluted region in the Czech Republic. Mutat Res Mol Mech Mutagen 713:76–82. https://doi.org/10.1016/j.mrfmmm.2011.06.001
Astley SB, Elliott RM, Archer DB, Southon S (2004) Evidence that dietary supplementation with carotenoids and carotenoid-rich foods modulates the DNA damage:repair balance in human lymphocytes. Br J Nutr 91:63–72. https://doi.org/10.1079/BJN20031001
Remely M, Ferk F, Sterneder S et al (2017) Vitamin E modifies high-fat diet-induced increase of DNA strand breaks, and changes in expression and DNA methylation of Dnmt1 and MLH1 in C57BL/6J male mice. Nutrients 9:607. https://doi.org/10.3390/nu9060607
Solovjov DA, Pluskota E, Plow EF (2005) Distinct roles for the α and β subunits in the functions of integrin αMβ2. J Biol Chem 280:1336–1345. https://doi.org/10.1074/jbc.M406968200
Jawhara S, Pluskota E, Cao W et al (2017) Distinct effects of integrins αXβ2 and αMβ2 on leukocyte subpopulations during inflammation and antimicrobial responses. Infect Immun 85:. https://doi.org/10.1128/IAI.00644-16
Schaefer A, Hordijk PL (2015) Cell-stiffness-induced mechanosignaling – a key driver of leukocyte transendothelial migration. J Cell Sci 128:2221–2230. https://doi.org/10.1242/jcs.163055
Gerhardt T, Ley K (2015) Monocyte trafficking across the vessel wall. Cardiovasc Res 107:321–330. https://doi.org/10.1093/cvr/cvv147
Weninger W, Biro M, Jain R (2014) Leukocyte migration in the interstitial space of non-lymphoid organs. Nat Rev Immunol 14:232–246. https://doi.org/10.1038/nri3641
Schwartz AB, Campos OA, Criado-Hidalgo E et al (2021) Elucidating the biomechanics of leukocyte transendothelial migration by quantitative imaging. Front Cell Dev Biol 9:. https://doi.org/10.3389/fcell.2021.635263
Lindner JR, Kahn ML, Coughlin SR et al (2000) Delayed onset of inflammation in protease-activated receptor-2-deficient mice. J Immunol 165:6504–6510. https://doi.org/10.4049/jimmunol.165.11.6504
Khandoga A, Kessler JS, Hanschen M et al (2006) Matrix metalloproteinase-9 promotes neutrophil and T cell recruitment and migration in the postischemic liver. J Leukoc Biol 79:1295–1305. https://doi.org/10.1189/jlb.0805468
Kroon J, Schaefer A, van Rijssel J et al (2018) Inflammation-sensitive myosin-X functionally supports leukocyte extravasation by Cdc42-mediated ICAM-1–rich endothelial filopodia formation. J Immunol 200:1790–1801. https://doi.org/10.4049/jimmunol.1700702
de Oliveira S, Rosowski EE, Huttenlocher A (2016) Neutrophil migration in infection and wound repair: going forward in reverse. Nat Rev Immunol 16:378–391. https://doi.org/10.1038/nri.2016.49
Cantin AM, Hartl D, Konstan MW, Chmiel JF (2015) Inflammation in cystic fibrosis lung disease: pathogenesis and therapy. J Cyst Fibros 14:419–430. https://doi.org/10.1016/j.jcf.2015.03.003
Wright HL, Moots RJ, Edwards SW (2014) The multifactorial role of neutrophils in rheumatoid arthritis. Nat Rev Rheumatol 10:593–601. https://doi.org/10.1038/nrrheum.2014.80
Tsukamoto T, Chanthaphavong RS, Pape H-C (2010) Current theories on the pathophysiology of multiple organ failure after trauma. Injury 41:21–26. https://doi.org/10.1016/j.injury.2009.07.010
Ley K, Laudanna C, Cybulsky MI, Nourshargh S (2007) Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol 7:678–689. https://doi.org/10.1038/nri2156
Luster AD, Alon R, von Andrian UH (2005) Immune cell migration in inflammation: present and future therapeutic targets. Nat Immunol 6:1182–1190. https://doi.org/10.1038/ni1275
Lawson JA, Fisher MA, Simmons CA et al (1998) Parenchymal cell apoptosis as a signal for sinusoidal sequestration and transendothelial migration of neutrophils in murine models of endotoxin and fas-antibody-induced liver injury. Hepatology 28:761–767. https://doi.org/10.1002/hep.510280324
Uchimura E, Watanabe N, Niwa O et al (2000) Transient infiltration of neutrophils into the thymus in association with apoptosis induced by whole-body X-irradiation. J Leukoc Biol 67:780–784. https://doi.org/10.1002/jlb.67.6.780
Iyoda T, Nagata K, Akashi M, Kobayashi Y (2005) Neutrophils accelerate macrophage-mediated digestion of apoptotic cells in vivo as well as in vitro. J Immunol 175:3475–3483. https://doi.org/10.4049/jimmunol.175.6.3475
Kluger MA, Zahner G, Paust H-J et al (2013) Leukocyte-derived MMP9 is crucial for the recruitment of proinflammatory macrophages in experimental glomerulonephritis. Kidney Int 83:865–877. https://doi.org/10.1038/ki.2012.483
Funding
This work was supported by a grant from the research programme (No: 5/8–4/17/Env/2020-NCD-II) funded by the Indian Council of Medical Research (ICMR), Department of Health Research, Ministry of Health and Family welfare, Government of India (New Delhi, India). We are also grateful to DST-FIST, Government of India (DLS[SR/FST/LSI-560/2013(C)]) and DBT-BUILDER (BT/INF/22/SP45088/2022).
Author information
Authors and Affiliations
Contributions
Jeet Maity: conceptualisation, data curation, analysis, investigation, validation, writing — original draft. Priyankar Pal: data curation. Prabir Kumar Mukhopadhyay and Ranjana Pal: conceptualisation, funding acquisition, project administration, resources, validation.
Corresponding author
Ethics declarations
Ethical Consent from Institutional Animal Ethical Committee
Prior to the start of the animal experiment, the Institutional Animal Ethics Committee provided its formal consent (Sanction No. PU/IAEC/PM/24).
Competing interests
The authors declare no competing interests.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maity, J., Pal, P., Pal, R. et al. Co-administration of L-Ascorbic Acid and α-Tocopherol Alleviates Arsenic-Induced Immunotoxicities in the Thymus and Spleen by Dwindling Oxidative Stress-Induced Inflammation. Biol Trace Elem Res 202, 2199–2227 (2024). https://doi.org/10.1007/s12011-023-03841-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03841-7