Abstract
Over the past years, adipose tissue has become an invaluable source of mesenchymal stem cells (MSCs) due to development of improved isolation methodologies. In a recent work, our group established a primary culture of human adipose-derived stem cells (hADSCs), which were characterized for their stem cell characteristics in detail and studied their myogenic differentiation potential in presence of boron. In the current study, we focused on the effects of a boron-containing compound, sodium pentaborate pentahydrate (NaB), on the adipogenic differentiation of hADSCs. Incorporation of boron in various chemical derivates has been a novel interest in drug-discovery attempts due to increasing number of reports on their anticancer, antibacterial, antiviral, and antifungal activities. In this report, a striking suppressive activity of boron on adipogenic differentiation of hADSCs is observed in a dose-dependent manner. Higher concentrations of NaB (20, 50, and 100 μg/mL (68, 170 and 340 μM)) resulted in a progressive decrease of lipid deposition, suppressed master regulators of adipogenesis transcriptional programming at the mRNA and protein levels, while having no evident cytotoxicity on the cells. The findings of this study are encouraging to undertake further investigations on potential beneficial effects boron in terms of its impact on normal and dysfunctional adipose biology. In that respect, these results pave the path to evaluate boron-based compounds in prevention and treatment of obesity which is a modern age pandemic that is predominant worldwide and found in strong association with comorbidities, including type 2 diabetes, hypertension, cardiovascular disease, cancers, and others.”
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is considered as a chronic disease due to excessive increase in fat deposition, particularly at the visceral level [1]. The prevalence of obesity in 2014 has almost tripled—particularly—in industrialized parts of the world since 1975; therefore, it is recognized as one of the major health challenges of the twenty-first century. For example, 650 million being obese, more than 1.9 billion adults (18 years and older), were recorded as overweight in 2016. Furthermore, based on 2016 numbers, the prevalence of childhood obesity is also on an alarming rise, 41 million children under the age of 5 and 340 million children between 5 and 19 were overweight or obese [2]. Worryingly, 70 million children under the age of 5 are predicted to be obese by 2025 [3]. Obesity is a complex disease, being often comorbid with type 2 diabetes mellitus, cardiovascular disease, hypertension, dyslipidemia, liver disease, and also various types of cancer, is thought to account for approximately 65% of all deaths and other debilitating health consequences, medical care for which creates profound economic burden worldwide [4]. Although precise mechanisms underlying its pathology are not fully understood, recent studies point to the dysregulation of the adipose tissue in terms of its response to many factors and/or those that it secretes, which are specifically termed as adipokines. Adipogenesis is a cell differentiation process and plays an important role in adipose development and systemic energy homeostasis. Furthermore, uncontrolled hyperplasia and/or hypertrophy of adipocytes are also recognized as major contributors of obesity development [5]. It is regulated by several transcription factors including CCAAT-enhancer-binding proteins (C/EBPα) and peroxisome proliferator-activated receptor gamma (PPARγ). Moreover, PPARγ is also required for the maintenance of differentiation and fat deposition mechanism [6].
Several strategies with a wide targeting range, including those that act on central nervous system (CNS) in control of satiety and appetite, to those targeting adipose tissue itself or other peripheral regulatory sites of energy homeostasis produced a number of pharmacotherapeutic agents. The performance of currently available antiobesity drugs is mostly insufficient in terms of achieving targets in weight loss and reversing unfavorable consequences of obesity and often results in severe side effects including hypertension, cardiovascular problems, liver complications, and psychological disorders. Hence, novel treatment methods that focus on targeting pathways in control of lipid metabolism to limit lipid storage and adipocyte generation with minimal side effects are in need [3]. That being mentioned elemental boron and its derivatives have been proposed to possess a therapeutic activity on these metabolic processes in recent studies [7, 8].
Elemental boron (B) is a semi-metal that is known to be essential for plants since the 1920s. Increasing evidence points to beneficial effects of boron not only for plants, but also for most animals and human cells. Boron has been associated with the bone development and maintenance, brain function, regulation of certain steroid hormones, and immune response [9]. It was reported that boron deprivation significantly affects both physiological and metabolic systems (lipid, mineral, bone, energy metabolism, and endocrine function) in mammalians [10,11,12,13,14,15]. Previous studies have shown that low-dose oral boric acid intake reduces body weight [16, 17]. Kucukkurt et al. indicated that 100-mg/kg boron supplementation in diet decreased body weight in rats [18]. In another study, moderate body weight reduction was observed in chicks that were kept on a diet supplemented with 3-mg/kg boron compounds [19]. In another work, severe body weight reduction was observed in male rats fed with boron compounds for 90 days [20]. To date, a limited number of studies reported weight loss inducing effects of boron and its derivatives. However, precise intracellular mechanisms underlying the antiobesity action of boron are not fully understood. To our knowledge, the current study is the first attempt to uncover the molecular pathways that are altered in response to presence of boron in a primary culture of human cells that were established from a lipoaspirated adipose tissue sample.
The aim of this study was to investigate the dose-dependent effect of sodium pentaborate pentahydrate (NaB) on in vitro adipogenesis and lipid formation in human adipose-derived stem cells (hADSCs).
Materials and Methods
Cell Culture and Maintenance
Mesenchymal stem cells (MSCs) used in the differentiation protocols of this study were obtained from Yeditepe University Biotechnology Laboratories [21]. hADCSs were cultured in complete growth medium which is composed of Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% (v/v) fetal bovine serum (FBS) and 1% (v/v) penicillin-streptomycin-amphotericin (PSA) (10.000 units/mL penicillin, 10.000 μg/mL streptomycin, 25 μg/mL amphotericin B; Invitrogen, Gibco, UK). Culture medium was changed every other day. After reaching 80–90% confluency, the cells were transferred to a T-150 flask (Zelkultur Flaschen, Switzerland) and were maintained at 37 °C and 5% CO2 in a humidified incubator. Cells from passages 4–6 were used in all experiments.
Characterization of hADSCs
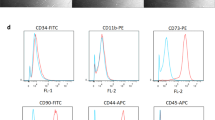
hADSCs were from our prior study were also used as the in vitro model in the current study Preservation of stem cell markers by these cells that were at late passages was verified according to the protocol described previously [22]. For characterization, cells were trypsinized and incubated with primary antibodies against CD14 (ab82434), CD31 (ab28364), CD34 (ab18227), CD44 (ab157107), CD45 (ab134202), CD73 (ab157335), CD90 (ab95700), CD105 (ab53321), Integrin (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA), and CD29 (Zymed, San Francisco, CA, USA) that were prepared in phosphate-buffered saline (PBS). After being washed with PBS, cells were incubated with the conjugated antibodies at 4 °C from 2 h to overnight. Flow cytometric analysis of the cells was performed using Becton Dickinson FACS Calibur flow cytometer system (Becton Dickinson, San Jose, CA, USA).
Cytotoxicity Assay
Five different concentrations of NaB (National Boron Research Institute-BOREN (Ankara, Turkey) including, 10, 20, 50, 100, and 150 μg/mL (34, 68, 170, 340, and 510 μM), 20% dimethyl sulfoxide (DMSO) (Fisher Scientific, New Jersey, cat. no. BP231-100) as a positive control (PC) and negative control (NC) were prepared in complete growth medium. Cells were seeded in 96-well-plates (BIOFIL, TCP, Switzerland) at a density of 5,000 cells/well. The following day, cells were treated with different concentrations of NaB and 20% (v/v) DMSO as PC. Cell viability was measured by the [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay (CellTiter96 Aqueous One Solution, Promega, UK) according to the manufacturer’s instructions. MTS is a yellow tetrazolium salt which is catabolized to formazan by a dehydrogenase enzyme in mitochondria of the living cells. Formazan is a purple compound, and the detection in this assay is based on the measurement of formazan compounds by an ELISA plate reader. After incubating the cells with NaB for 24, 48, and 72 h, treatment medium was replaced with a mix of 10 μL MTS and 100 μL full growth medium, where the cells were incubated for another 2 h before measuring the absorbance at 490 nm in a plate reader (BioTek Instruments, Inc., VT, USA).
Differentiation of hADSCs
The adipogenic differentiation process was triggered to allow differentiation of hADSCs into adipogenic cells using a previously published method [23]. Twenty-four hours after seeding hADSC cells in 6-well plates at a density of 1.5 × 105cells/well, complete growth medium was replaced by the differentiation medium that was composed of DMEM, 10% (v/v) FBS, 1 μM dexamethasone, 100 μM indomethacin (Sigma, USA), 500 μM IBMX (Calbiochem, Merck Millipore, Germany), and 0.01 mg/mL insulin (Gibco, UK). Twenty-four hours after medium change, cells were incubated with different concentrations (20, 50, and 100 μg/mL (68, 170, and 340 μM)) of NaB or without at 37 °C and 5% CO2 for a 10-day period when the culture medium was changed every other day. Positive control groups were treated with only differentiation medium while negative control groups were cultured only in complete medium.
Oil Red O Staining
Oil Red O is a staining protocol that allows an accurate visualization of lipid droplets as an indicator of adipogenic differentiation. Oil Red O solution was prepared by dissolving 0.5 g Oil Red O (Sigma, USA) in 100 mL isopropanol. The cells were then fixed with 2% (w/v) paraformaldehyde for 30 min followed by three washes in PBS. The cells were then incubated with Oil Red O solution (diluted at 6:4 ratio in PBS) for 1 h for staining. Cells were washed with PBS and observed under the light microscope [24].
Reverse Transcription Polymerase Chain Reaction Analysis
Total RNA isolation from differentiated cells was performed using the High Pure RNA Isolation Kit (Roche, Germany) according to the manufacturer’s instructions. Complementary DNA (cDNA) synthesis from isolated RNA samples was done using High Fidelity cDNA Synthesis Kit (Roche, Germany). Real-time PCR was performed using Maxima SYBR Green/ROX (Fermentas, USA) to determine the expression levels of marker genes after differentiation. cDNAs from the differentiated cells were used as template and were mixed with primers and Maxima SYBR Green/ROX qPCR Master Mix (2X). The housekeeping gene, glyceraldehyde 3-phosphate dehydrogenase (GAPDH), was used for the normalization of the data. The results of real-time PCR data were normalized to the mRNA level of GAPDH. Primer sequences for marker genes are shown in Table 1.
Protein Isolation and Western Blot Analysis
Whole-cell pellets were dissolved in RIPA buffer containing phosphatase and proteinase inhibitors (sc-24,948; Santa Cruz Biotechnology), and total protein concentrations were estimated using a Pierce BCA Protein Assay Kit (Thermo Fisher). Proteins (20 μg) were loaded on Mini-PROTEAN TGX Precast Gels (Bio-Rad) and transferred to nitrocellulose membranes (Thermo Fisher). The membranes were incubated overnight at 4 °C with the following primary antibodies: anti-CEBPα (#2295), anti-PPARγ (#2430), and GAPDH (#5174) (Cell Signaling Technology). The membranes were then probed with horseradish peroxidase (HRP)-conjugated anti-rabbit antibody (Cell Signaling Technology) for 1 h at room temperature. The images were taken using a luminometer system (Bio-Rad), and band intensities were measured by Image Lab Software V.5.2.1.
Statistical Analysis
All data are shown as the means ± standard errors (S.E.). The statistical analysis of the results was analyzed with one-way ANOVA with the multiple comparison Tukey’s test using GraphPad Prism statistical software 5.0 (GraphPad Prism, USA). Statistical significance was determined at p < 0.05.
Results
Isolation and Characterization of Mesenchymal Stem Cell-Derived from Human Fat Tissue
hADSCs, which were successfully isolated and expanded from lipoaspirated fat tissue samples, showed fibroblast-like cell morphology. Isolated cells at passage 3 were characterized for their MSC surface markers using flow cytometry. hADSCs were characterized for the surface markers including CD29, CD34, CD45, CD73, CD90, CD105, CD133, and CD166 by flow cytometry. Cells were positive for CD29, CD44, CD73, CD90, and CD105, MSC surface markers, whereas they were negative for CD14, CD34, and CD45, hematopoietic stem cell (HSC), surface markers, and for CD31, endothelial cell marker (Fig. 1a).
Cytotoxicity of NaB in hADSCs
The impact of various NaB concentrations (10, 20, 50, 100, and 150 μg/mL (34, 68, 170, 340, and 510 μM)) on hADSC viability were tested for 3 days at 24, 48, and 72-h time points using the MTS assay. The results showed that none of the concentrations tested NaB was found to be toxic to hADSCs (Fig. 1b). On the contrary, NaB increased the survival of cells at each concentration for days 2 and 3 when compared to NC.
Assessment of Adipogenesis in Presence of NaB
The impact of NaB on adipogenic differentiation at different concentrations (20, 50, and 100 μg/mL (68, 170, and 340 μM) was studied based on fat droplet size and changes in gene expression levels of key transcriptional factors both at mRNA and protein levels.
Fat Droplet Visualization During Adipogenic Differentiation
Oil Red O staining was performed to visualize the intracellular lipid vesicles after adipogenic differentiation at day 10. Lipid vesicles were detected in high abundance in the PC. hADSCs were exposed to NaB at different doses (20, 50, and 100 μg/mL (68, 170, and 340 μM)), and cell differentiation was performed by incubating cells in the differentiation medium. As shown in Fig. 2, treatment of hADSCs with NaB markedly inhibited adipocyte differentiation in a dose-dependent manner. These results indicated that NaB may have efficiently suppressed adipocyte differentiation and has potential antiobesity effects on hADSCs.
Effects of NaB on adipocyte differentiation in hADSCs. Oil Red O staining of hADSCs undergoing adipogenic differentiation at 20, 50, and 100 μg/mL (68, 170, and 340 μM) NaB concentrations. Scale bar 100 μm. NaB, sodium pentaborate pentahydrate; hADSCs, human adipose-derived stem cells; PC, positive control; NC, negative control
Changes in Gene Expression Levels in Key Transcription Factors
Expression levels of markers for terminal adipocyte differentiation, including adiponectin, adipocyte protein 2 (αP2), Lipoprotein lipase (LPL), CEBP α, and peroxisome proliferator-activated receptor γ (PPAR-γ), were detected by real-time PCR analysis at day 10. During adipogenic differentiation, cells treated with NaB showed lower mRNA expression levels for all of the above-mentioned marker genes compared to the levels detected in the PC at all concentrations of NaB (20, 50, and 100 μg/mL (68, 170, and 340 μM)). Since the mRNA levels of all the terminal marker genes were completely diminished at 100 μg/mL (340 μM) NaB compared to the maximal levels seen in PC, this NaB treatment is the most effective in blocking adipogenic differentiation (Fig. 3).
Quantification of PPAR-γ and CEBPα Protein Levels
To determine the effects of NaB treatment on adipogenic protein expression, CEBPα and PPAR-γ protein levels were detected. Levels of PPAR-γ protein were decreased significantly at the end of 10-day-differentiation period in all of the NaB treatment groups (20, 50, and 100 μg/mL (68, 170, and 340 μM)). Twenty-microgram per milliliter and 50-μg/mL NaB treatment exerted similar effect on PPAR-γ protein level compared to that seen in 100-μg/mL NaB treatment. On the other hand, expression levels of CEBPα protein were lowered in a dose-dependent manner throughout the NaB treatment gradient (20, 50, and 100 μg/mL (68, 170, and 340 μM)). Maximal repression in CEBPα and PPAR-γ protein levels was detected at the 100-μg/mL NaB concentration (Fig. 4).
Discussion
Adipogenesis plays a central role in mechanisms controlling fat deposition by regulating adipose development and systemic energy homeostasis that is often deregulated in obesity [25, 26]. PPARγ and C/EBPα are two of the key transcription factors in regulation of fat deposition [27]. Up/downregulation of PPARγ modulates adipogenesis in MSCs by controlling fat deposition [28,29,30]. In addition, C/EBPα triggers adipogenesis via PPARγ-related pathways [27, 31]. Targeting the activities of these transcription factors in control of adipogenesis has been proposed as a promising approach for the treatment of obesity and related diseases [32,33,34,35]. There are challenges in antiobesity drug development, because multiple factors ranging from imbalance in energy metabolism, mutations in genes responsible for metabolism, to the differences in habits in artificial food consumption amongst individuals impact development of obesity [31]. Moreover, antiobesity drugs, that have been developed so far, performed limited therapeutic effect due to their cytotoxic and other unfavorable side effects. Therefore, novel therapeutic approaches that are more effective, specific, safe, and better-tolerated are in need for the treatment of obesity. Findings from previous studies point to the antiobesity activity of boron or boron-containing compounds in animal cells [36]; however, details of molecular circuitry underlying their mechanism-of-action are not fully understood.
In this study, both the toxicity and the potency to inhibit adipogenic differentiation for NaB were investigated in the human ADSC in vitro model. First, characteristics of MSCs isolated from fat tissue were confirmed using flow cytometry. Cells were positive for MSC cell-surface marker and negative for HSC surface marker criteria for which are determined by the International Society for Cellular Therapy (ISCT) [37].
In the present study, potential cytotoxic effects of NaB at five different concentrations on hADSCs were investigated by measuring cell viability on the first, second, and third day using MTS assay. According to the MTS results, no significant differences in cell viability were observed in any of the five treatment groups for each NaB concentration compared to the NC (p < 0.05).
In order to evaluate the effects of different concentrations of NaB on adipogenesis, the hADSCs were induced to differentiate for 10 days. Following induction, adipogenesis and fat formation in the cells were confirmed by Oil Red O staining, mRNA expression levels of adiponectin, αP2, LPL, CEBPα, and PPAR-γ, and protein levels of CEBPα and PPAR-γ.
According to our results from the Oil Red O staining, the dose-dependent decrease in extent of staining observed in NaB treatment groups suggested suppression of fat deposition at increasing concentrations of NaB in hADSCs compared to the parallel cultures incubated in the adipogenic differentiation medium alone (PC). Due to their sensitivity in detecting changes both in mRNA and protein levels, RT-PCR and Western blot analysis were performed, respectively, as a read-out for adipogenesis in cell culture. mRNA expression levels of adiponectin, αP2, LPL, CEBPα, and PPAR-γ were evaluated. While hADSC cultures induced for adipogenic differentiation (positive control) progressively expressed adipogenesis-related markers, including adiponectin, αP2, LPL, and PPAR-γ, there were statistically significant decreases in the expression of these markers in NaB-treated hADSC cultures in a dose-dependent manner.
These results are pioneering in the sense that they open a whole new discussion about using boron-based compounds in treatment of obesity and its comorbidities. Current studies in our laboratory focus on how boron alters adipose biology in vivo animal models. To further investigate how boron impacts adipose physiology, changes in levels of several other factors in control of adipogenesis must be determined. Both in the current and the previous study, a suppressive activity of boron on differentiation of pre-adipocytes into mature adipocytes was observed which are the predominant cell type found in adipose tissue in addition to pre-adipocytes and endothelial and immune cells that are other components of adipose architecture [38]. Transitions between the three major mammalian types of adipocytes of the white adipose tissue (WAT), brown adipose tissue (BAT), and beige adipose tissue draw attention due to their therapeutic potential in battling obesity. One worthwhile question to address is whether boron would have an impact on transition of WAT adipocytes into thermogenic and heat-dissipating BAT adipocytes [39]. Finally, a chronic inflammatory response that is mediated by an acute and abnormal accumulation of macrophages in obese WAT was shown to become a systemic effect that could be responsible for the steady increase in adiposity and insulin resistance in mouse models of obesity through the enhancement of adipolysis and—thereby—increasing the plasma levels of free fatty acid [40]. While abundance of macrophages is estimated as 5% of the cells in lean adipose tissue, this number becomes as high as 50% in obese adipose tissue. Although the precise shift in anti-inflammatory-to-pro-inflammatory role of macrophages in lean versus obese adipose tissue, respectively, is only beginning to be understood; impact of boron on this switch and metabolic activity of macrophages should be investigated for a comprehensive evaluation of boron-based compounds as antiobesity agents [41].
Conclusion
To our knowledge, this is the first study that demonstrates the effects of NaB on adipogenic differentiation of ADSCs that were isolated from human adipose tissue. The results showed that the NaB does not have any cytotoxic effect on the cells isolated from fat tissue at the five different concentrations tested. In addition, adipogenic differentiation capacity of hADSCs is suppressed by the NaB treatment in a dose-dependent manner. Hence, based on our observation that boron exerts a suppressive effect on fat deposition in the hADSC model, NaB should be further evaluated for its therapeutic potential in the treatment of obesity. The results of this study are promising both for the management and for the treatment of obesity and related disorders. However, further studies need to be performed to reveal the impact of boron both on metabolic activities of all major cell types of the adipose niche and plasticity of the these cell types in order to establish its placement in the obesity armamentarium.
References
Paniagua JA (2016) Nutrition, insulin resistance and dysfunctional adipose tissue determine the different components of metabolic syndrome. World J Diabetes 7(19):483–514
W.H. Organization (2018) Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/
Barja-Fernandez S, Leis R, Casanueva F, Seoane L (2014) Drug development strategies for the treatment of obesity: how to ensure efficacy, safety, and sustainable weight loss. Drug Design, Development and Therapy 8:2391
Prieto-Hontoria PL, Perez-Matute P, Fernandez-Galilea M, Bustos M, Martinez JA, Moreno-Aliaga MJ (2011) Role of obesity-associated dysfunctional adipose tissue in cancer: a molecular nutrition approach. Biochim Biophys Acta 1807(6):664–678
Jung UJ, Choi M-S (2014) Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci 15(4):6184–6223
Shao X, Wang M, Wei X, Deng S, Fu N, Peng Q, Jiang Y, Ye L, Xie J, Lin Y (2016) Peroxisome proliferator-activated receptor-γ: master regulator of adipogenesis and obesity. Current Stem Cell Research & Therapy 11(3):282–289
Doğan A, Demirci S, Apdik H, Bayrak OF, Gulluoglu S, Tuysuz EC, Gusev O, Rizvanov AA, Nikerel E, Şahin F (2017) A new hope for obesity management: boron inhibits adipogenesis in progenitor cells through the Wnt/β-catenin pathway. Metab Clin Exp 69:130–142
Das BC, Thapa P, Karki R, Schinke C, Das S, Kambhampati S, Banerjee SK, Van Veldhuizen P, Verma A, Weiss LM, Evans T (2013) Boron chemicals in diagnosis and therapeutics. Future Med Chem 5(6):653–676
Nielsen FH, Meacham SL (2011) Growing evidence for human health benefits of boron. JEBCAM 16(3):169–180
Gallardo-Williams MT, Maronpot RR, Turner CH, Johnson CS, Harris MW, Jayo MJ, Chapin RE (2003) Effects of boric acid supplementation on bone histomorphometry, metabolism, and biomechanical properties in aged female F-344 rats. Biol Trace Elem Res 93(1–3):155–169
Hall I, Spielvogel B, Griffin T, Docks E, Brotherton R (1989) The effects of boron hypolipidemic agents on LDL and HDL receptor binding and related enzyme activities of rat hepatocytes, aorta cells and human fibroblasts. Res Commun Chem Pathol Pharmacol 65(3):297–317
Hunt CD, Herbel JL, Idso JP (1994) Dietary boron modifies the effects of vitamin D3 nutrition on indices of energy substrate utilization and mineral metabolism in the chick. J Bone Miner Res 9(2):171–182
Kurtoğlu F, Kurtoğlu V, Celik I, Kececi T, Nizamlioğlu M (2005) Effects of dietary boron supplementation on some biochemical parameters, peripheral blood lymphocytes, splenic plasma cells and bone characteristics of broiler chicks given diets with adequate or inadequate cholecalciferol (vitamin D3) content. Br Poult Sci 46(1):87–96
Kurtoĝlu V, Kurtoĝlu F, Coşkun B (2001) Effects of boron supplementation of adequate and inadequate vitamin D3-containing diet on performance and serum biochemical characters of broiler chickens. Res Vet Sci 71(3):183–187
Nielsen FH, Schuler TR, Zimmerman TJ, Uthus EO (1988) Main content area dietary magnesium, manganese and boron affect the response of rats to high dietary aluminum. Magnesium 7(3):133–147
Aysan E, Sahin F, Telci D, Erdem M, Muslumanoglu M, Yardımcı E, Bektasoglu H (2013) Mechanism of body weight reducing effect of oral boric acid intake. Int J Endocrinol 2013:1–5
Basoglu A, Baspinar N, Tenori L, Vignoli A, Gulersoy E (2017) Effects of boron supplementation on peripartum dairy cows’ health. Biol Trace Elem Res 179(2):218–225
Kucukkurt I, Akbel E, Karabag F, Ince S (2015) The effects of dietary boron compounds in supplemented diet on hormonal activity and some biochemical parameters in rats. Toxicol Ind Health 31(3):255–260
Hunt CD (1994) The biochemical effects of physiologic amounts of dietary boron in animal nutrition models. Environ Health Perspect 102(Suppl 7):35
Weir RJ Jr, Fisher RS (1972) Toxicologic studies on borax and boric acid. Toxicol Appl Pharmacol 23(3):351–364
Yildiz K, Tasli PN, Sahin F, Guneren E (2016) Comparison of cellular alterations in fat cells harvested with laser-assisted liposuction and suction-assisted liposuction. The Journal of Craniofacial Surgery 27(3):631–635
Taşlı PN, Doğan A, Demirci S, Şahin F (2013) Boron enhances odontogenic and osteogenic differentiation of human tooth germ stem cells (hTGSCs) in vitro. Biol Trace Elem Res 153(1–3):419–427
Somuncu OS, Tasli PN, Sisli HB, Somuncu S, Sahin F (2015) Characterization and differentiation of stem cells isolated from human newborn foreskin tissue. Appl Biochem Biotechnol 177(5):1040–1054
Doğan A, Yalvaç ME, Şahin F, Kabanov AV, Palotás A, Rizvanov AA (2012) Differentiation of human stem cells is promoted by amphiphilic pluronic block copolymers. Int J Nanomedicine 7:4849
Ali AT, Hochfeld WE, Myburgh R, Pepper MS (2013) Adipocyte and adipogenesis. Eur J Cell Biol 92(6–7):229–236
Lefterova MI, Lazar MA (2009) New developments in adipogenesis. Trends Endocrinol Metab 20(3):107–114
Rosen ED, Walkey CJ, Puigserver P, Spiegelman BM (2000) Transcriptional regulation of adipogenesis. Genes Dev 14(11):1293–1307
Hegele RA, Cao H, Frankowski C, Mathews ST, Leff T (2002) PPARG F388L, a transactivation-deficient mutant, in familial partial lipodystrophy. Diabetes 51(12):3586–3590
Koutnikova H, Cock T-A, Watanabe M, Houten SM, Champy M-F, Dierich A, Auwerx J (2003) Compensation by the muscle limits the metabolic consequences of lipodystrophy in PPARγ hypomorphic mice. Proc Natl Acad Sci 100(24):14457–14462
Tontonoz P, Hu E, Spiegelman BM (1994) Stimulation of adipogenesis in fibroblasts by PPARγ2, a lipid-activated transcription factor. Cell 79(7):1147–1156
Farmer SR (2006) Transcriptional control of adipocyte formation. Cell Metab 4(4):263–273
El-Jack AK, Hamm JK, Pilch PF, Farmer SR (1999) Reconstitution of insulin-sensitive glucose transport in fibroblasts requires expression of both PPARγ and C/EBPα. J Biol Chem 274(12):7946–7951
Rosen ED, Hsu C-H, Wang X, Sakai S, Freeman MW, Gonzalez FJ, Spiegelman BM (2002) C/EBPα induces adipogenesis through PPARγ: a unified pathway. Genes Dev 16(1):22–26
Wu Z, Rosen ED, Brun R, Hauser S, Adelmant G, Troy AE, McKeon C, Darlington GJ, Spiegelman BM (1999) Cross-regulation of C/EBPα and PPARγ controls the transcriptional pathway of adipogenesis and insulin sensitivity. Mol Cell 3(2):151–158
Zuo Y, Qiang L, Farmer SR (2006) Activation of CCAAT/enhancer-binding protein (C/EBP) α expression by C/EBPβ during adipogenesis requires a peroxisome proliferator-activated receptor-γ-associated repression of HDAC1 at the C/ebpα gene promoter. J Biol Chem 281(12):7960–7967
Dogan A, Demirci S, Apdik H, Bayrak OF, Gulluoglu S, Tuysuz EC, Gusev O, Rizvanov AA, Nikerel E, Sahin F (2017) A new hope for obesity management: boron inhibits adipogenesis in progenitor cells through the Wnt/beta-catenin pathway. Metab Clin Exp 69:130–142
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8(4):315–317
Apdik H, Doğan A, Demirci S, Aydın S, Şahin F (2015) Dose-dependent effect of boric acid on myogenic differentiation of human adipose-derived stem cells (hADSCs). Biol Trace Elem Res 165(2):123–130
Gómez-Hernández A, Beneit N, Díaz-Castroverde S, Escribano Ó (2016) Differential role of adipose tissues in obesity and related metabolic and vascular complications. Int J Endocrinol 2016:1–15
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112(12):1821–1830
Boutens L, Stienstra R (2016) Adipose tissue macrophages: going off track during obesity. Diabetologia 59(5):879–894
Acknowledgements
The authors thank Prof. Dr. Ilhan Satman, Director of Turkish Public Health and Chronic Diseases Institute and Dr. Yıldız Tutuncu, Faculty at Capa School of Medicine, Istanbul University, for their insightful comments and useful discussions on the manuscript.
Funding
The study was funded by Yeditepe University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Abdik, E.A., Abdik, H., Taşlı, P.N. et al. Suppressive Role of Boron on Adipogenic Differentiation and Fat Deposition in Human Mesenchymal Stem Cells. Biol Trace Elem Res 188, 384–392 (2019). https://doi.org/10.1007/s12011-018-1428-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1428-5