Abstract
Objective
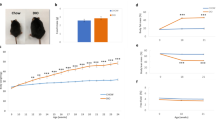
Obesity induced metabolic dysregulation results in cluster of chronic conditions mainly hyperglycemia, hyperinsulinemia, dyslipidemia, diabetes, cardiovascular complications and insulin resistance. To investigate the effect of i.m. injection of human adipose tissue derived mesenchymal stem cells and its secretome in correcting obesity induced metabolic dysregulation in high fat diet fed obese model of mice and understand its mechanism of action.
Subjects
We injected human adipose tissue derived mesenchymal stem cells (ADMSCs) suspension (CS), conditioned medium (CM) and the cell lysate (CL) intramuscularly in high fat diet (HFD)-induced C57BL/6 mice. Metformin was used as a positive control. ADMSCs were traced in vivo for its bio distribution after injection at different time points.
Results
ADMSCs-treated mice exhibited remarkable decrease in insulin resistance as quantified by HOMA-IR and triglyceride glucose index with concomitant decrease in oxidized LDL and IL6 as compared with the untreated control. CS injection showed improvement in glucose tolerance and reduction in fatty infiltration in the liver, macrophage infiltration in adipose and hypertrophy of the islets resulting from HFD. Upregulation of miRNA-206, MyoD and increase in protein content of the skeletal muscle in CS-treated mice indicates plausible mechanism of action of ADMSCs treatment in ameliorating IR in HFD mice.
Conclusion
Of all the three treatments, CS was found to be the best. ADMSCs were found to have migrated to different organs in order to bring about the correction in dysregulated metabolism induced by obesity. Our results open up a novel treatment modality for possible therapeutic usage in human subjects by employing autologous or allogeneic ADMSCs for the better management of obesity induced metabolic dysregulation.





Similar content being viewed by others
References
Hursting SD, Dunlap SM. Obesity, metabolic dysregulation, and cancer: a growing concern and an inflammatory (and microenvironmental) issue. Ann N Y Acad Sci. 2012;1271:82–7.
Collins KH, Herzog W, MacDonald GZ, Reimer RA, Rios JL, Smith IC, et al. Obesity, metabolic syndrome, and musculoskeletal disease: common inflammatory pathways suggest a central role for loss of muscle integrity. Front Physiol. 2018;23:112.
Ranganath SH, Levy O, Inamdar MS, Karp JM. Harnessing the mesenchymal stem cell secretome for the treatment of cardiovascular disease. Cell Stem Cell. 2012;10:244–58.
Semedo P, Burgos-Silva M, Donizetti-Oliveira C, Saraiva Camara NO. How do mesenchymal stem cells repair? Stem Cells in Clinic and Research; 2011.
Pileggi A. Mesenchymal stem cells for the treatment of diabetes. Diabetes. 2012;61:1355–56.
Cao M, Pan Q, Dong H, Yuan X, Li Y, Sun Z, et al. Adipose-derived mesenchymal stem cells improve glucose homeostasis in high-fat diet-induced obese mice. Stem Cell Research & Therapy. 2015;6:208.
Badimon L, Onate B, Vilahur G. Adipose-derived mesenchymal stem cells and their reparative potential in ischemic heart disease. Rev Esp Cardiol. 2015;68:599–611.
Si Y, Zhao Y, Hao H, Liu J, Guo Y, et al. Infusion of mesenchymal stem cells ameliorates hyperglycemia in type 2 diabetic rats: identification of a novel role in improving insulin sensitivity. Diabetes. 2012;61:1616–25.
Ji AT, Chang YC, Fu YJ, Lee OK, Ho JK. Niche-dependent regulations of metabolic balance in high-fat-diet-induced diabetic mice by mesenchymal stromal cells. Diabetes. 2015;64:926–36.
Bueno Pde G, Yochite JN, Derigge-Pisani GF, Malmegrim de Farias KC, de Avó LR, Voltarelli JC, et al. Metabolic and pancreatic effects of bone marrow mesenchymal stem cells transplantation in mice fed high-fat diet. PLoS ONE. 2015;10:e0124369.
Shree N, Venkategowda S, Venkatranganna MV, Bhonde RR. Treatment with adipose derived mesenchymal stem cells and their conditioned media reverse carrageenan induced paw oedema in db/db mice. Biomed Pharmacother. 2017;90:350–3.
Shree N, Bhonde RR. Conditioned media from adipose tissue derived mesenchymal stem cells reverse insulin resistance in cellular models. J Cell Biochem. 2017;118:2037–43.
Wang CY, Liao JK. A mouse model of diet-induced obesity and insulin resistance. Methods Mol Biol. 2012;821:421–33.
Anil TM, Harish C, Lakshmi MN, Harsha K, Onkaramurthy M, Sathish Kumar V, et al. CNX-012-570, a direct AMPK activator provides strong glycemic and lipid control along with significant reduction in body weight; studies from both diet-induced obese mice and db/db mice models. Cardiovasc Diabetol. 2014;13:27.
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 2010;8:e1000412.
Ayala JE, Samuel VT, Morton GJ, Obici S, Croniger CM, Shulman GI, et al. Standard operating procedures for describing and performing metabolic tests of glucose homeostasis in mice. Dis Model Mech. 2010;3:525–34.
Gopurappilly R, Bhonde R. Can multiple intramuscular injections of mesenchymal stromal cells overcome insulin resistance offering an alternative mode of cell therapy for type 2 diabetes? Med Hypotheses. 2012;78:393–5.
Bouzakri K, Plomgaard P, Berney T, Donath MY, Pedersen BK, Halban PA. Bimodal effect on pancreatic β-cells of secretory products from normal or insulin-resistant human skeletal muscle. Diabetes. 2012;60:1111–21.
Pedersen L, Hojman P. Muscle-to-organ cross talk mediated by myokines. Adipocyte. 2012;1:164–7.
Yajnik CS, Yudkin JS. The Y-Y paradox. Lancet. 2004;363:163.
Hardikar AA, Satoor SN, Karandikar MS, Joglekar MV, Puranik AS, Wong W, et al. Multigenerational undernutrition increases susceptibility to obesity and diabetes that is not reversed after dietary recuperation. Cell Metab. 2015;22:312–9.
Roberts CK, Hevener AL, Barnard RJ. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise. Training. Compr Physiol. 2013;3:1–58.
Wannamethee SG, Lowe GD, Shaper AG, Rumley A, Lennon L, Whincup PH. The metabolic syndrome and insulin resistance: relationship to haemostatic and inflammatory markers in older non-diabetic men. Atherosclerosis. 2005;181:101–8.
Atkinson BJ, Griesel BA, King CD, Josey MA, Olson AL. Moderate GLUT4 overexpression improves insulin sensitivity and fasting triglyceridemia in high-fat diet-fed transgenic mice. Diabetes. 2013;62:2249–58.
Auguet T, Berlanga A, Guiu-Jurado E, Martinez S, Porras JA, Aragonès G, et al. Altered fatty acid metabolism-related gene expression in liver from morbidly obese women with non-alcoholic fatty liver disease. Int J Mol Sci. 2014;15:22173–87.
Targher G, Bertolini L, Scala L, Zenari L, Lippi G, Franchini M, et al. Plasma PAI-1 levels are increased in patients with nonalcoholic steatohepatitis. Diabetes Care. 2007;30:e31–2.
Moon BC, Hernandez-Ono A, Stiles B, Wu H, Ginsberg HN. Apolipoprotein B secretion is regulated by hepatic triglyceride, and not insulin, in a model of increased hepatic insulin signaling. Arterioscler Thromb Vasc Biol. 2012;32:236–46.
Bravo E, Palleschi S, Aspichueta P, Buqué X, Rossi B, Cano A, et al. High fat diet-induced non alcoholic fatty liver disease in rats is associated with hyperhomocysteinemia caused by down regulation of the transsulphuration pathway. Lipids Health Dis. 2011;10:60.
Ferolla SM, Silva L, Ferrari Mde L, da Cunha AS, Martins Fdos S, Couto CA, et al. Dietary approach in the treatment of nonalcoholic fatty liver disease. World J Hepatol. 2015;7:2522–34.
Roat R, Rao V, Doliba NM, Matschinsky FM, Tobias JW, Garcia E, et al. Alterations of pancreatic islet structure, metabolism and gene expression in diet-induced obese C57BL/6J mice. PLoS ONE. 2014;9:e86815.
Collins KH, Hart DA, Reimer RA, Seerattan RA, Banker CW, Sibole SC, et al. High-fat high-sucrose diet leads to dynamic structural and inflammatory alterations in the rat vastus lateralis muscle. J Orthop Res. 2016;34:2069–78.
Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, de Rekeneire N, et al. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care. 2009;32:1993–7.
Abrigo J, Rivera JC, Aravena J, Cabrera D, Simon F, Ezquer F, et al. High fat diet-induced skeletal muscle wasting is decreased by mesenchymal stem cells administration: implications on oxidative stress, ubiquitin proteasome pathway activation, and myonuclear apoptosis. Oxid Med Cell Longev. 2016;2016:9047821.
Pillai RS. MicroRNA function: multiple mechanisms for a tiny RNA? RNA. 2005;11:1753–61.
Tranzer A, Stadler PF. Evolution of microRNAs. Methods Mol Biol. 2006;342:335–50.
Liu N, Williams AH, Maxeiner JM, Bezprozvannaya S, Shelton JM, Richardson JA, et al. microRNA-206 promotes skeletal muscle regeneration and delays progression of Duchenne muscular dystrophy in mice. J Clin Investig. 2012;122:2054–65.
Ma Guoda, Wang Yajun, Li You, Cui Lili, Zhao Yujuan, Zhao Bin, et al. MiR-206, a key modulator of skeletal muscle development and disease. Int J Biol Sc. 2015;11:345–52.
Dey BK, Gagan J, Dutta A. miR-206 and -486 induce myoblast differentiation by downregulating Pax7. Mol Cell Biol. 2011;31:203–14.
Gao X, Salomon C, Freeman DJ. Extracellular vesicles from adipose tissue—a potential role in obesity and type 2 diabetes? Front Endocrinol. 2017;8:202.
Vyas B, Shah A, Marathe A, Ansarullah, Vyas R, Bhonde R. Adipose tissue: a natural resource for multipotent mesenchymal stem cells with potential translation to trigerminal layers. Indian J Plast Surg. 2018;51:177–81.
Ejarque M, Ceperuelo-Mallafré V, Serena C, Maymo-Masip E, Duran X, Díaz-Ramos A et al. Adipose tissue mitochondrial dysfunction in human obesity is linked to a specific DNA methylation signature in adipose-derived stem cells. Int J Obes. 2018; https://doi.org/10.1038/s41366-018-0219-6.
Payab M, Goodarzi P, Heravani NF, Hadavandkhani M, Zarei Z, Falahzadeh K, et al. Stem cell and obesity: current state and future perspective. Adv Exp Med Biol. 2018;1089:1–22.
Goodarzi P, Alavi-Moghadam S, Sarvari M, Tayanloo Beik A, Falahzadeh K, Aghayan H, et al. Adipose tissue-derived stromal cells for wound healing. Adv Exp Med Biol. 2018;1089:1–22.
Acknowledgements
Authors wish to thank Dr. Anandhwardhan Hardikar, University of Sydney, Australia for his technical inputs in the miRNA study. We would also like to thank ACTREC, Tata memorial Hospital, Mumbai, India for carrying out the LCMS/MS study.
Author contributions
NS and SV carried out the experimental work. MVV suggested for experimental design and provided the animal facility. ID designed the in vivo tracking of the cells and provided the facility for the same. RRB designed the experiment, executed the experimental work and wrote the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shree, N., Venkategowda, S., Venkatranganna, M.V. et al. Human adipose tissue mesenchymal stem cells as a novel treatment modality for correcting obesity induced metabolic dysregulation. Int J Obes 43, 2107–2118 (2019). https://doi.org/10.1038/s41366-019-0438-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0438-5
- Springer Nature Limited
This article is cited by
-
Placental mesenchymal stem cells restore glucose and energy homeostasis in obesogenic adipocytes
Cell and Tissue Research (2023)
-
Effects of stem cells from inducible brown adipose tissue on diet-induced obesity in mice
Scientific Reports (2021)
-
The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice
Scientific Reports (2021)
-
The promise(s) of mesenchymal stem cell therapy in averting preclinical diabetes: lessons from in vivo and in vitro model systems
Scientific Reports (2021)