Abstract
Purpose of review
The purpose of this review is to summarize and discuss current options and new advances in the treatment of sleep-related hypermotor epilepsy (SHE), focusing on pharmacological and surgical treatments.
Recent findings
Carbamazepine (CBZ) has traditionally been regarded as the first-line treatment option in SHE patients. In patients showing an unsatisfactory response to monotherapy, topiramate (TPM), lacosamide (LCM) and acetazolamide (ACZ) could be reasonable add-on strategies. The increasing understanding of the role of neuronal nicotinic acetylcholine receptor (nAChR) in SHE pathophysiology has led to the evaluation of compounds able to modulate this receptor system, including nicotine patches and fenofibrate. Despite polytherapy with two or more antiepileptic drugs (AEDs), about one-third of SHE patients suffer from drug-resistant seizures. In selected drug-resistant patients, epilepsy surgery is a therapeutic approach that offers high probability of recovery, with up to two-third of patients becoming seizure-free after resection of the epileptogenic zone.
Summary
An evidence-based approach from randomized placebo-controlled trials in SHE patients is lacking, and current treatment recommendations are based only on case reports and small series.
Furthermore, most of these case reports and case series involve patients with a known genetic defect, which only accounts for a small proportion of SHE patients. Therefore, a prospective study in a large cohort of sporadic SHE patients is necessary in order to provide clinicians with an evidence-based treatment for this rare form of epilepsy. An early and effective anti-epileptic treatment is mandatory for SHE patients, in order to prevent the risk of increasing seizure frequency throughout the disease course with relevant impact on patients’ cognitive profile and daytime performances.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lugaresi E, Cirignotta F. Hypnogenic paroxysmal dystonia : epileptic seizure or a new syndrome ? Sleep. 1981;4(2):129–38.
Tinuper P, Cerullo A, Cirignotta F, Cortelli P, Lugaresi E, Montagna P. Nocturnal paroxysmal dystonia with short-lasting attacks: three cases with evidence for an epileptic frontal lobe origin of seizures. Epilepsia. 1990;31(5):549–56.
•• Tinuper P, Bisulli F, Cross JH, Hesdorffer D, Kahane P, Nobili L, et al. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology. 2016;86(19):1834–42. The paper summarized the results of the Consensus Conference held in Bologna, Italy in 2014 on SHE during which the Nocturnal Frontal Lobe Epilepsy was renamed Sleep-Related Hypermotor Epilepsy (SHE). Major points of agreement emerged on the relationship of the seizures with sleep and not with the circadian pattern of seizure occurrence and on the possible extrafrontal origin of hypermotor seizures. Diagnostic criteria with different level of certainty are also provided.
Tinuper P, Bisulli F. From nocturnal frontal lobe epilepsy to sleep-related hypermotor epilepsy: a 35-year diagnostic challenge. Seizure. 2017;44:87–92.
Montagna P, Sforza E, Tinuper P, Cirignotta F, Lugaresi E. Paroxysmal arousals during sleep. Neurology. 1990;40:1063–6.
Vignatelli L, Bisulli F, Giovannini G, Licchetta L, Naldi I. Prevalence of nocturnal frontal lobe epilepsy in the adult population of Bologna and Modena, Emilia Romagna region. Italy Sleep. 2015;38(3):479–85.
•• Provini F, Plazzi G, Tinuper P, Vandi S, Lugaresi E, Montagna P. Nocturnal frontal lobe epilepsy: a clinical and polygraphic overview of 100 consecutive cases. Brain. 1999;122(6):1017–31. The most large series of clinical and polysomnographic data of NFLE including a detailed characterization of the different seizure types that constitute NFLE. In these series, carbamazepine completely abolishes the seizures in approximately 20% of the cases and gives remarkable relief (reduction of the seizures by at least 50%) in another 48%.
Scheffer IE, Bhatia KP, Lopes-Cendes I, Fish DR, Marsden CD, Andermann F, et al. Autosomal dominant frontal epilepsy misdiagnosed as sleep disorder. Lancet. 1994;343(8896):515–7.
Becchetti A, Aracri P, Meneghini S, Brusco S, Amadeo A. The role of nicotinic acetylcholine receptors in autosomal dominant nocturnal frontal lobe epilepsy. Front Physiol. 2015;6:1–13.
Parrino L, Halasz P, Tassinari CA, Terzano MG. CAP, epilepsy and motor events during sleep: the unifying role of arousal. Sleep Med Rev. 2006;10(4):267–85.
Heron SE, Smith KR, Bahlo M, Nobili L, Kahana E, Licchetta L, et al. Missense mutations in the sodium-gated potassium channel gene KCNT1 cause severe autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet. 2012;44(11):1188–90.
Milligan CJ, Li M, Gazina EV, Heron SE, Nair U, Trager C, et al. KCNT1 gain of function in 2 epilepsy phenotypes is reversed by quinidine. Ann Neurol. 2014;75(4):581–90.
•• Licchetta L, Bisulli F, Di VL, Mostacci B, Rinaldi C, Trippi I. Sleep-related hypermotor epilepsy long-term outcome in a large cohort. Neurology. 2017;88(1):70–7. The paper reported the poor prognosis of SHE analysing 139 patients with a 16-year median follow-up.
Vignatelli L, Bisulli F, Naldi I, Ferioli S, Pittau F, Provini F, et al. Excessive daytime sleepiness and subjective sleep quality in patients with nocturnal frontal lobe epilepsy: a case-control study. Epilepsia. 2006;47(SUPPL. 5):73–7.
Licchetta L, Poda R, Vignatelli L, Pippucci T, Zenesini C, Menghi V, et al. Profile of neuropsychological impairment in sleep-related hypermotor epilepsy. Sleep Med. 2018;48:8–15.
Raju GP, Sarco DP, Poduri A, Riviello JJ, Bergin AMR, Takeoka M. Oxcarbazepine in children with nocturnal frontal-lobe epilepsy. Pediatr Neurol. 2007;37(5):345–9.
Oldani A, Manconi M, Zucconi M, Martinelli C, Ferini-Strambi L. Topiramate treatment for nocturnal frontal lobe epilepsy. Seizure. 2006;15(8):649–52.
Willoughby JO, Pope KJ, Eaton V. Nicotine as an antiepileptic agent in ADNFLE: an N-of-one study. Epilepsia. 2003;44(9):1238–40.
Mullen SA, Carney PW, Roten A, Ching M, Lightfoot PA, Churilov L, et al. Precision therapy for epilepsy due to KCNT1 mutations: a randomized trial of oral quinidine. Neurology. 2018;90(1):e67–72.
Puligheddu M, Melis M, Pillolla G, Milioli G, Parrino L, Terzano GM, et al. Rationale for an adjunctive therapy with fenofibrate in pharmacoresistant nocturnal frontal lobe epilepsy. Epilepsia. 2017;58(10):1762–70.
Yoshimura R, Yanagihara N, Terao T, Minami K, Abe K, Izumi F. Inhibition by carbamazepine of various ion channels-mediated catecholamine secretion in cultured bovine adrenal medullary cells. Naunyn Schmiedeberg's Arch Pharmacol. 1995;352(3):297–303.
Scheffer IE, Bhatia KP, Lopes-Cendes I, Fish DR, Marsden CD, Andermann E, et al. Autosomal dominant nocturnal frontal lobe epilepsy. A distinctive clinical disorder. Brain. 1995;118(Pt 1):61–73.
Picard F, Bertrand S, Steinlein OK, Bertrand D. Mutated nicotinic receptors responsible for autosomal dominant nocturnal frontal lobe epilepsy are more sensitive to carbamazepine. Epilepsia. 1999;40(9):1198–209.
Di Resta C, Ambrosi P, Curia G, Becchetti A. Effect of carbamazepine and oxcarbazepine on wild-type and mutant neuronal nicotinic acetylcholine receptors linked to nocturnal frontal lobe epilepsy. Eur J Pharmacol. 2010;643(1):13–20.
Mula M, Cavanna AE, Monaco F. Psychopharmacology of topiramate: from epilepsy to bipolar disorder. Neuropsychiatr Dis Treat. 2006;2(4):475–88.
Rogawski MA, Tofighy A, White HS, Matagne A, Wolff C. Current understanding of the mechanism of action of the antiepileptic drug lacosamide. Epilepsy Res. 2015;110:189–205.
Liguori C, Romigi A, Placidi F, Sarpa MG, Mercuri NB, Izzi F. Effective treatment of nocturnal frontal lobe epilepsy with lacosamide: a report of two cases. Sleep Med. 2016;23:121–2.
Samarasekera SR, Berkovic SF, Scheffer IE. A case series of lacosamide as adjunctive therapy in refractory sleep-related hypermotor epilepsy (previously nocturnal frontal lobe epilepsy). J Sleep Res. 2018;27(5):1–4.
Reiss WG, Oles KS. Acetazolamide in the treatment of seizures. Ann Pharmacother. 1996;30(5):514–9.
Oles KS, Penry JK, Cole DL, Howard G. Use of acetazolamide as an adjunct to carbamazepine in refractory partial seizures. Epilepsia. 1989;30(1):74–8.
Varadkar S, Duncan JS, Cross JH. Acetazolamide and autosomal dominant nocturnal frontal lobe epilepsy. Epilepsia. 2003;44(7):986–7.
Brodtkorb E, Picard F. Tobacco habits modulate autosomal dominant nocturnal frontal lobe epilepsy. Epilepsy Behav. 2006;9(3):515–20.
Zerem A, Nishri D, Yosef Y, Blumkin L, Lev D, Leshinsky-Silver E, et al. Resolution of epileptic encephalopathy following treatment with transdermal nicotine. Epilepsia. 2013;54(1):2012–4.
Naldi I, Bisulli F, Vignatelli L, Licchetta L, Pittau F, Di L, et al. Tobacco habits in nocturnal frontal lobe epilepsy. Epilepsy Behav. 2013;26(1):114–7.
Mills EJ, Wu P, Lockhart I, Wilson K, Ebbert JO. Adverse events associated with nicotine replacement therapy (NRT) for smoking cessation. A systematic review and meta-analysis of one hundred and twenty studies involving 177,390 individuals. Tob Induc Dis. 2010;8(1):8.
Chong PF, Nakamura R, Saitsu H, Matsumoto N, Kira R. Ineffective quinidine therapy in early onset epileptic encephalopathy with KCNT1 mutation. Ann Neurol. 2016;79:502–3.
Mikati MA, Jiang YH, Carboni M, Shashi V, Petrovski S, Spillmann R, et al. Quinidine in the treatment of KCNT1-positive epilepsies. Ann Neurol. 2015;78(6):995–9.
Puligheddu M, Pillolla G, Melis M, Lecca S, Marrosu F, de Montis MG, et al. PPAR-alpha agonists as novel antiepileptic drugs: preclinical findings. PLoS One. 2013;8(5):e64541.
Yamada J, Zhu G, Okada M, Hirose S, Yoshida S, Shiba Y, et al. A novel prophylactic effect of furosemide treatment on autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE). Epilepsy Res. 2013;107(1–2):127–37.
Dibbens LM, de Vries B, Donatello S, Heron SE, Hodgson BL, Chintawar S, et al. Mutations in DEPDC5 cause familial focal epilepsy with variable foci. Nat Genet. 2013;31(45):546.
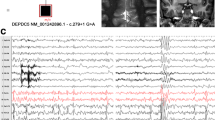
Scheffer IE, Heron SE, Regan BM, Mandelstam S, Crompton DE, Hodgson BL, et al. Mutations in mammalian target of rapamycin regulator DEPDC5 cause focal epilepsy with brain malformations. Ann Neurol. 2014;75(5):782–7.
Picard F, Makrythanasis P, Navarro V, Ishida S, de Bellescize J, Ville D, et al. DEPDC5 mutations in families presenting as autosomal dominant nocturnal frontal lobe epilepsy. Neurology. 2014;82(23):2101–6.
Pippucci T, Licchetta L, Baldassari S, Marconi C, De Luise M, Myers C, et al. Contribution of ultrarare variants in mTOR pathway genes to sporadic focal epilepsies. Ann Clin Transl Neurol. 2019;6(3):475–85.
Bar-Peled L, Chantranupong L, Cherniack AD, Chen WW, Ottina KA, Grabiner BC, et al. A tumor suppressor complex with GAP activity for the rag GTPases that signal amino acid sufficiency to mTORC1. Science. 2013;340(6136):1100–6.
Jeong A, Wong M. Targeting the mammalian target of rapamycin for epileptic encephalopathies and malformations of cortical development. J Child Neurol. 2018;33(1):55–63.
Parker WE, Orlova KA, Parker WH, Birnbaum JF, Krymskaya VP, Goncharov DA, et al. Rapamycin prevents seizures after depletion of STRADA in a rare neurodevelopmental disorder. Sci Transl Med. 2013;5(182):182ra53.
Foldvary-Schaefer N. Sleep complaints and epilepsy: the role of seizures, antiepileptic drugs and sleep disorders. J Clin Neurophysiol. 2002;19(6):514–21.
Nobili L, Sartori I, Terzaghi M, Stefano F, Mai R, Tassi L, et al. Relationship of epileptic discharges to arousal instability and periodic leg movements in a case of nocturnal frontal lobe epilepsy: a stereo-EEG study. Sleep. 2006;29(5):701–4.
•• Nobili L, Francione S, Mai R, Cardinale F, Castana L, Tassi L, et al. Surgical treatment of drug-resistant nocturnal frontal lobe epilepsy. Brain. 2007;130(2):561–73. The paper provides the evidence that patients with drug-resistant, disabling sleep-related seizures of frontal lobe origin should be considered for resective surgery, which may provide excellent results both on seizures and on epilepsy-related sleep disturbances.
Losurdo A, Proserpio P, Cardinale F, Gozzo F, Tassi L, Mai R, et al. Drug-resistant focal sleep related epilepsy: results and predictors of surgical outcome. Epilepsy Res. 2014;108(5):953–62.
Proserpio P, Cossu M, Francione S, Gozzo F, Lo Russo G, Mai R, et al. Epileptic motor behaviors during sleep: anatomo-electro-clinical features. Sleep Med. 2011;12(SUPPL. 2):S33–8.
Nobili L, Cardinale F, Magliola U, Cicolin A, Didato G, Bramerio M, et al. Taylor’s focal cortical dysplasia increases the risk of sleep-related epilepsy. Epilepsia. 2009;50(12):2599–604.
Handforth A, DeGiorgio CM, Schachter SC, Uthman BM, Naritoku DK, Tecoma ES, et al. Vagus nerve stimulation therapy for partial-onset seizures: a randomized active-control trial. Neurology. 1998;51(1):48–55.
Carreño M, Garcia-Alvarez D, Maestro I, Fernández S, Donaire A, Boget T, et al. Malignant autosomal dominant frontal lobe epilepsy with repeated episodes of status epilepticus: successful treatment with vagal nerve stimulation. Epilepsia. 2011;52(11):e168–71.
Manni R, Terzaghi M. Comorbidity between epilepsy and sleep disorders. Epilepsy Res. 2010;90(3):171–7.
Malow BA, Foldvary-Schaefer N, Vaughn BV, Selwa LM, Chervin RD, Weatherwax KJ, et al. Treating obstructive sleep apnea in adults with epilepsy: a randomized pilot trial. Neurology. 2008;71(8):572–7.
Malow BA, Weatherwax KJ, Chervin RD, Hoban TF, Marzec ML, Martin C, et al. Identification and treatment of obstructive sleep apnea in adults and children with epilepsy: a prospective pilot study. Sleep Med. 2003;4(6):509–15.
Vendrame M, Auerbach S, Loddenkemper T, Kothare S, Montouris G. Effect of continuous positive airway pressure treatment on seizure control in patients with obstructive sleep apnea and epilepsy. Epilepsia. 2011;52(11):168–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Asioli declares that he has no conflict of interest. Dr. Rossi declares that he has no conflict of interest. Dr. Bisulli declares that she has no conflict of interest. Dr. Licchetta declares that she has no conflict of interest. Dr. Tinuper reports non-financial support and other from EISAI, non-financial support and other from LIVANOVA, non-financial support and other from UCB, non-financial support and other from GW, outside the submitted work. Dr. Provini reports personal fees from Vanda Pharmaceutical, personal fees from Sanofy, personal fees from Zambon, personal fees from Fidia, personal fees from Bial, personal fees from Eisai Japan, personal fees from Italfarmaco, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Asioli, G.M., Rossi, S., Bisulli, F. et al. Therapy in Sleep-Related Hypermotor Epilepsy (SHE). Curr Treat Options Neurol 22, 1 (2020). https://doi.org/10.1007/s11940-020-0610-1
Published:
DOI: https://doi.org/10.1007/s11940-020-0610-1